| It is proposed to rename this page to the Lacrimal Gland. Explanation of reasons and discussion - on the Wikipedia page: Towards renaming / October 26, 2017 . |
| It is proposed to combine this page with the Tear and Lacrimal apparatus pages. Explanation of reasons and discussion - on the Wikipedia page: Toward unification / October 31, 2017 . The discussion lasts at least a week (more details). Do not delete the template until the discussion is concluded. |
Drawing of the lacrimal apparatus of the human right eye.
The lacrimal gland is located at the top left. The right side of the image is towards the nose. Lacrimal glands.
- exocrine glands located in the front of the eyes, secreting tears, are part of the lacrimal apparatus. Divided into[1]:
- the actual (or main
)
lacrimal gland
is paired (one in each eye), almond-shaped [2]. - Wolfring's accessory lacrimal glands
- 8 in number are located at the inner edge of the conjunctival cartilage (3 in the upper, 1 in the lower in each eye). - accessory lacrimal glands of Krause
- in the amount of 42-96 are located in the thickness of the eyelids at the fornix of the conjunctiva - the place of transition of the conjunctiva of the eyelids to the conjunctiva of the sclera (15-40 in the upper, 6-8 in the lower in each eye).
The lacrimal gland is present in reptiles, birds and all mammals[3].
Physiology and functions
The tear secreted by the main lacrimal gland enters the conjunctival sacs through the ducts and, mixing with the secretions of other glands of the conjunctiva and eyelids, participates in the formation of excess tear fluid. Secretion by the main lacrimal gland occurs for the most part only reflexively upon irritation of the cornea, conjunctiva and nasal mucosa, or during psycho-emotional reactions (crying) and reaches 30 ml/min. Normally, with the constant formation of tear fluid, it does not participate [1]. The functioning of the lacrimal gland begins 2 months after birth[4], which is why practically no lacrimation is observed before this age; in old age, the function of the lacrimal gland gradually declines[5].
In addition to the main lacrimal gland, in the conjunctiva of the sclera and eyelids there are several dozen additional small lacrimal glands that produce tears to constantly moisturize the eyes with tear fluid under normal conditions. The tear secreted by the accessory lacrimal glands accounts for about 10% of its total secretion.
, amounting to 0.5-2 ml/day and provides basal hydration of the eyes under normal conditions. This explains, in particular, that if the main lacrimal gland is damaged, the eye does not dry out. Accessory lacrimal glands can be damaged by chemical burns of the conjunctiva[1][4].
The human lacrimal glands perform a number of essential functions that are responsible for maintaining the normal and constant functioning of the cornea and conjunctiva. The lacrimal glands produce tears, the main water-containing component of the tear fluid, which performs the optical, trophic and protective function of the outer anterior surface of the eyeball. The lacrimal glands also secrete mucins, which make up 50% of tears [1].
Pathologies of the lacrimal gland
Developmental pathologies include underdevelopment or complete absence of the gland. Often there is an obstruction or tear flow, as a result of which the tear fluid cannot function normally. Surgery is indicated. With inflammation of the lacrimal gland, hypersecretion of tear fluid is observed. Hypersecretion can also be caused by external irritants (exposure to cold, sun or allergic reactions). With mechanical damage and inflammation of the excretory ducts, there is a risk of developing stenosis. Tumors in the lacrimal glands are rare and are often benign. A symptom of papilloma, adenoma or fibroma can be excessive enlargement of the glands. Malignant tumors cause severe pain in the eye and lacrimal glands, and the quality of vision decreases. A rather rare disease is acute dacryoadenitis. It occurs as a complication after an infectious disease. With hyperfunction of the lacrimal gland, increased dryness of the eyeball is noted.
Anatomy and histology
a — lacrimal gland of the right eye, b — superior lacrimal punctum, c — superior lacrimal canal, d — lacrimal sac, e — inferior lacrimal punctum, f — inferior lacrimal canal, g — nasolacrimal duct. Drawing of a transverse histological section of the upper eyelid.
Conjunctival side on the left Lacrimal gland (lat. glandula lacrimalis) The lacrimal gland itself
- a complex alveolar-tubular exocrine gland, which consists of a large number of lobules separated by connective tissue, each of which, in turn, contains many acinar lobules. Each of the acinar lobules consists only of glandular cells and produces a watery serous secretion. The intralobular ducts join to form the interlobular ducts, which in turn become the excretory ducts. The ducts of the lacrimal gland resemble branched tubes in structure. The excretory ducts of the lacrimal gland open with several openings in the lateral (outer) corner of the superior fornix of the conjunctiva [6]. The excretory ducts themselves are covered with double-layered columnar epithelium. The gland cells have a conical shape, with their apex oriented into the lumen of the ducts [3].
The lacrimal gland is divided into two parts by the tendon of the muscle that lifts the upper eyelid (lat. musculus levator palpebrae superioris) [7] [1]:
- orbital (orbital) - a larger part (about 25 × 12 × 5 mm), located in the upper outer (lateral) part of each orbit in the lacrimal fossa
, (lat. fossa glandulae lacrimalis), on the lower surface of the orbital part of the frontal bone.
Contains interlobular ducts, which are combined with 3-5 main excretory ducts, connected to the ducts of the palpebral part, secreting tears in the lateral part of the conjunctival sac
at the upper edge of the eyelid cartilage. - century (palpebral) - the smaller part (about 11 × 8 × 2 mm), located lower at the upper fornix of the conjunctiva
closer to the inner surface of the upper eyelid. If you turn out the upper eyelid, you can see the palpebral part. Some of the ducts flow into the ducts of the orbital part of the gland, 3-9 ducts open independently in the same place as the ducts of the upper part.
The tear released from the ducts due to the capillary effect and surface tension is distributed over the conjunctival sacs and the surface of the conjunctival mucosa, and when blinking or closed eyelids, over the outer surface of the cornea, as part of the tear fluid
mixing with the secretions of other glands, some accumulate in
the lacrimal lake
at the inner edge of the eyes.
Further, in the normal state of the eyes, the excess tear fluid that has not evaporated, carrying with it the sloughed epithelium and dust particles, is removed through the drainage system of the lacrimal apparatus into the lower nasal passage
of the nasal cavity, where it is mixed with the secretions of the nasal mucosa.
With excess production of tears by the gland, reflexively, normally or pathologically, the excess tear fluid accumulated in the conjunctival sacs, without having time to be removed through the drainage system, flows out through the edge of the eyelids (lacrimation) [4]. Accessory lacrimal glands (lat. glandulae lacrimales accessoriae)
In structure and secreted serous secretion, they are similar to the lobules of the main lacrimal gland [4]. The shape is oval or round, they may have several lobes. Wolfring's accessory lacrimal glands are located at the upper edge of the superior cartilage and at the lower edge of the lower eyelid cartilage. The accessory lacrimal glands of Krause are located in the superior and inferior conjunctival fornix[1].
Innervation
The lacrimal nerve, emerging from the ophthalmic nerve (the first branch of the trigeminal nerve), provides the sensory component of the innervation of the lacrimal gland. The greater petrosal nerve (a branch of the facial nerve), emerging from the facial nerve, provides parasympathetic autonomic innervation to the lacrimal gland. Greater petrosal nerve
passes along the branches of V1 and V2 of the trigeminal nerve.
Parasympathetic innervation originates in the pons from the lachrymation nucleus of the facial nerve. From the nucleus of the pons, preganglionic parasympathetic fibers pass through the intermediate nerve (a small extension of the facial nerve) to the geniculate ganglion
, but they do not form synapses there.
From the geniculate ganglion,
preganglionic fibers then pass into
the greater petrosal nerve
, which carries parasympathetic secretomotor fibers through the foramen lacerum, where
the greater petrosal nerve
joins the deep petrosal nerve (which contains the postganglionic sympathetic fibers
of the main cervical ganglion
), forming
the nerve of the pterygoid canal
(
Vidian nerve
), which then turns through
the pterygoid canal
into
the pterygopalatine ganglion
.
Here the fibers contact the postganglionic neurons, and the postganglionic fibers connect to the fibers of the maxillary nerve. In the pterygopalatine fossa itself, parasympathetic secretory fibers connect to the zygomatic nerve and then pass into the lacrimal branch
of the ophthalmic part
of the trigeminal nerve
, which also provides sensitive innervation to the lacrimal gland.
Sympathetic postganglionic fibers arise from the main cervical ganglion
.
They pass through the internal carotid plexus and the deep petrosal nerve
, joining the
greater petrosal nerve
in
the pterygoid canal
.
Together, the greater
and
deeper petrosal nerves
form
the nerve of the pterygoid canal
, and it reaches
the pterygopalatine ganglion
in
the pterygopalatine fossa
.
Unlike their parasympathetic counterparts, sympathetic fibers do not synapse in the pterygopalatine ganglia
, the cell bodies of postganglionic neurons are located in the sympathetic trunk. Sympathetic fibers run in parallel with parasympathetic fibers innervating the lacrimal gland.
Blood supply
The lacrimal gland is supplied with blood by the lacrimal artery, which arises from the ophthalmic artery. The outflow of venous blood occurs through the superior ophthalmic vein.
Lymphatic drainage
Lymph from the lacrimal gland flows into the superficial lymph nodes.
- Ophthalmic artery of the right eye and its branches
- Nerves of the right orbit. View from above
- Medial rectus muscle, lacrimal gland and nerves of the left eye. Anatomical preparation
- Scheme of sympathetic and parasympathetic innervation of the junction of the sphenopalatine and superior cervical ganglion
Pathologies of the lacrimal duct in infants
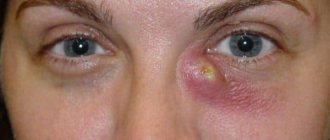
Quite often after birth, infants may experience discharge from the eyes. There are often cases when the discharge is purulent. This problem may indicate dacryocystitis. The problem is most often associated with a jelly-like plug that is located in the duct. It is necessary for the fetus to protect the nasolacrimal flow from the ingress of amniotic fluid.
With loud crying in the first minutes of life, this plug should burst. If this does not happen, then tears begin to accumulate in the future and an infection develops. The main symptoms that will indicate obstruction of the lacrimal duct include:
- Discharge that occurs when pressure is applied to the lacrimal sac.
- The presence of a tear in one of the corners of the eye.
- Redness and swelling of the eyelids.
- Unreasonable lacrimation.
As you can see, the tear duct in babies is subject to various problems in the first days of life. You can get rid of the problems that have arisen by instilling various drugs. In some cases, massages help. We have already written an article about how to massage the lacrimal canal for newborns.
Pathology
Due to disruption of the tear glands, dry, itchy and burning eyes may occur, which are signs of dry eye syndrome or Sicca keratoconjunctivitis. In this syndrome, the tear glands produce less tear fluid. This is mainly due to the aging process or taking certain medications. To determine total tear production
You can use the Schirmer test (Schirmer-I test),
the main tear production
is the Jones test (Schirmer-II test, the following can also be used:
test thread test
,
lactoferrin test
,
test with sodium fluorescein dilution
,
assessment of the height of the tear meniscus
). Many medications or diseases that cause dry eye syndrome can also cause insufficient salivation and dry mouth. Treatment varies depending on the etiology and includes avoiding irritants, stimulating lacrimation, increasing tear production, clearing the eyelids, and treating ocular inflammation[8].
In addition, there are other pathologies of the lacrimal gland [4]:
- developmental anomalies - absence or underdevelopment of the main lacrimal gland
- lacrimal gland injuries
- lacrimal gland tumors
- dacryoadenitis - inflammation of the lacrimal gland due to bacterial and viral infections, with autoimmune diseases also affecting the salivary glands, such as Sjögren's, Schauman's, Mikulicz's diseases
- dacryops - a cyst of the lacrimal glands, both main and accessory (in the latter it is associated with trachoma)
- displacement of the lacrimal gland (congenital or acquired)
Composition of tears
The lacrimal glands secrete a secretion known as tears. Tear fluid consists of water, protein, mineral salts, mucus, urea and lysozyme. Lysozyme has a bactericidal effect, so when tears are secreted, the main apple is cleansed and receives additional protection from harmful microorganisms. The continuous secretion of tear fluid during wakefulness helps flush out foreign small objects such as grains of sand or small insects from the eye. In a calm state, the lacrimal gland secretes about 1 ml of tears per day. With emotional shock and excessive crying, up to 10 ml of tear fluid can be released. With increasing age, the natural secretion of the protective tear layer decreases, and patients after 40 years of age often complain of dryness and pain in the eyes.
Notes
- ↑ 1 2 3 4 5 6 Brzhesky V.V., Somov E.E.
Corneal-conjunctival xerosis (diagnosis, clinic, treatment) / 2nd ed., revised. and additional // St. Petersburg: Lefty. Saint Petersburg. - 2003. - 120 p. ISBN 5-93356-027-8. (P. 5-12). - Clinically Oriented Anatomy, Dalley & Agur.
- ↑ 1 2 Dogel A. S.
Lacrimal glands // Encyclopedic Dictionary of Brockhaus and Efron: in 86 volumes (82 volumes and 4 additional). - St. Petersburg, 1890-1907. - ↑ 1 2 3 4 5 Avetisov S. E., Egorov E. A., Moshetova L. K., Neroev V. V., Takhchidi H. P.
Ophthalmology: national guide // M.: GEOTAR-Media. - 2008. - 944 p., ill. ISBN 978-5-9704-0707-3. (pp. 72-83, 362-399). - Tarkhanov I.R.
Tears // Encyclopedic Dictionary of Brockhaus and Efron: in 86 volumes (82 volumes and 4 additional). - St. Petersburg, 1890-1907. - “eye, human.”Encyclopædia Britannica. 2010. Encyclopædia Britannica 2010 Ultimate Reference Suite DVD 2010
- Sapin M. R., Bocharov V. Ya., Nikityuk D. B., Satyukova G. S., Selin Yu. M., Spirin B. A.
Human anatomy / In 2 vols. T. 2, 5th ed. . reworked and additional // M.: Medicine. - 2001. - 640 p., ill. ISBN 5-225-04586-3. (pp. 583-589). - Illustrated Anatomy of the Head and Neck, Fehrenbach and Herring, Elsevier, 2012, page 153.
Literature
- Diseases of the lacrimal organs: Monograph / Cherkunov B.F. - Samara: State Enterprise "Perspective", 2001. - 296 p. — ISBN 5-900031-43-8.
- Lacrimal glands // Small encyclopedic dictionary of Brockhaus and Efron: in 4 volumes - St. Petersburg, 1907-1909.
- Lacrimal glands // Great Soviet Encyclopedia: [in 30 volumes] / ch. ed. A. M. Prokhorov. — 3rd ed. - M.: Soviet Encyclopedia, 1969-1978.
- Beloglazov V. G.
Lacrimal organs // Great Medical Encyclopedia, 3rd ed. - M.: Soviet Encyclopedia. - T. 23. - Volokonenko A.I.
Conjunctiva // Great Medical Encyclopedia, 3rd ed. - M.: Soviet Encyclopedia. - T. 11.