When a tear duct is blocked, the eye's drainage system is either partially or completely blocked, preventing tears from draining naturally. This leads to watery eyes, irritation or chronic eye infection.
Most tears come from the lacrimal glands located above the eyes. Tears run down the surface of the eye, lubricating and protecting it, and then fall into tiny holes (points) in the corners of the upper and lower eyelids. They then pass through small channels in the eyelids to the lacrimal sac, the junction of the eyelids and the side of the nose, then down the nasopharyngeal duct and are either evaporated or reabsorbed before entering the nose.
Infants may have a congenital tear duct obstruction : almost one in five babies are born with a blocked tear duct, but this anomaly usually resolves after 4-6 months.
In adults, a blocked tear duct can be caused by an eye infection, swelling, injury, or tumor.
Cause of tear duct blockage
The baby's lacrimal cavity is underdeveloped. As the child grows, the canal increases in length. Before the baby is born, the transition from the eyes to the nose is covered with a small film that prevents amniotic fluid from entering the respiratory tract.
At birth, the film breaks and opens a passage for tears to flow into the nasopharynx. But in 8% of children this does not happen and a tear stagnates in one eye. In 1% of patients, the film does not disappear in both channels.
Before birth, instead of a thin membrane, a thick film consisting of unnecessary cells and secretion may form in the tear duct. At the same time, it becomes more difficult to break through the channel. The length of the lacrimal cavity in a newborn is only 8 mm, which increases the risk of bacterial infection of the lacrimal sac. This disease is called dacryocystitis.
The risk of pathology does not depend on the sex of the child and is not inherited. Treatment initially takes place at home. But there are a number of reasons why dacryocystitis in newborns requires surgical intervention: absence of a cavity, disruption of the structure of the lacrimal sac, congenital narrowing, curvature of the nose, trauma due to difficult childbirth.
Symptoms of the disease
Manifestations of dacryocystitis in newborns are externally similar to the signs of another purulent eye disease - conjunctivitis:
- In the second week of the baby's life, purulent discharge from the eyes appears.
- Pus is released from the lacrimal openings if you press lightly on the area where the lacrimal sac is located.
- The conjunctiva and skin at the inner corner of the eye turns red.
- The eyelids swell and swell.
- Tears flow from the eyes even when the child is not crying.
- When the baby wakes up, his eyelashes are stuck together.
- Such manifestations can occur in both eyes at once, or in one.
Symptoms of a blocked tear duct
Blockage of the tear duct in newborns appears within 24 hours after birth. Sometimes dacryocystitis becomes noticeable later.
Symptoms of blockage include the following:
- stagnation of tears;
- lacrimation;
- redness of the eyeball;
- swelling of the eyelid;
- the appearance of white or green pus in the lacrimal sac;
- sticking of eyelashes after sleep.
A newborn baby cries without tears. The appearance of a flowing tear should alert parents.
Tearfulness may come and go. Redness of the conjunctiva does not always occur. Occurs after the appearance of purulent discharge and infection of the conjunctiva. The more severe the condition, the greater the redness and swelling of the eyelids. With proper and timely treatment, these symptoms may not appear.
The appearance of pus is a symptom of dacryocystitis or conjunctivitis. But when the lacrimal duct is blocked, pus accumulates in the inner part of the eyelid, and when you press on the lacrimal sac with your finger, the amount of discharge increases. There is more pus when the child cries or screams for a long time.
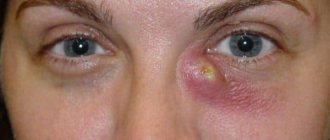
If left untreated, bacteria can multiply rapidly, causing the lacrimal sac to enlarge and stretch. In advanced cases, the swelling increases to the size of a cherry and interferes with the child. Stretching of the eyelid leads to atrophy and does not allow the production of tears to cleanse the eye, which leads to worsening of the condition. The appearance of a fistula or phlegmon is a severe complication of dacryocystitis.
Classification and symptoms
Based on the nature of its course, dacryocystitis is divided into acute and chronic.
Due to its appearance, obstruction of the lacrimal canal can be chlamydial, allergenic, traumatic, or viral. Clinical signs vary depending on the form of the disease. Acute dacryocystitis has the following striking symptoms:
- swelling of the eyelid;
- fever;
- compaction of the lacrimal sac, “fat lumps” near the eyes;
- hyperthermia of the skin near the lacrimal canal.
A constantly clogged tear duct leads to a rapid transition from acute to chronic dacryocystitis. This form is characterized by ongoing inflammation of the lacrimal sac. The resulting tumor softens, hyperthermia decreases, and an abscess forms, which can open on its own. Purulent exudate flows out of it, after which the inflammation subsides.
Massage for newborns
Blockage of the lacrimal canal in newborns in 99% of cases is treated with conservative methods without surgery. Massage is the most popular and effective. The ophthalmologist or pediatrician teaches parents the technique during the appointment.
Attention should be paid to the pressing force. Strong pressure will cause pain and discomfort to the child, weak pressure will not lead to results. Massage must be performed 4-6 times a day to achieve results. Correct actions increase the pressure in the tear duct and remove the film.
Before the massage, it is necessary to trim your nails so as not to injure the child. Wash your hands with soap to avoid eye infection. Pre-purulent discharge is removed with a soft cloth or tampon soaked in a furatsilin solution. Eye cleansing is carried out from the outer part of the eyelid to the inner. Gauze will damage the delicate mucous membrane of the newborn.
After preparation, the massage is performed according to the following rule:
- Determine the tubercle in the inner part of the lacrimal sac that protrudes as much as possible above the surface of the skin and is distant from the eye.
- Press this point not hard, but noticeably enough to create pressure in the tear duct.
- Run your finger from top to bottom towards the child’s nose, applying force.
- Repeat 5-10 times.
- If pus appears in the eye, cleanse it again and continue the massage.
- At the end of the procedure, antibacterial drops are instilled into the eyes.
Massage can be performed more than 4 times a day, but use the drops strictly according to the instructions. The medications that are best suited for the child should be prescribed by an ophthalmologist or pediatrician. It is advisable to take a pathogenic flora sensitivity test to identify the group of bacteria that caused the eye infection.
A common treatment for a blocked tear duct in a newborn is massage. The photo shows one of the technology options
Treatment is carried out for at least 2 weeks. If the massage technique is followed, the disease resolves in 99% of children under the age of 1 year, 30% of newborns recover by the age of 2 months. The older the child gets, the longer it takes to get results.
Drug therapy
Drug treatment is prescribed by an ophthalmologist to eliminate bacterial infection of the eye sac and relieve inflammation. In medical practice, eye drops are used. They are easy to use and are available for any age.
After testing for sensitivity to pathogenic flora, the doctor selects drops that will be effective. If testing is not possible, then broad-spectrum antibiotics are prescribed.
Drugs prescribed for the treatment of dacryocystitis:
| A drug | Description of the drug |
| Vitabact | It has an antimicrobial effect and is widely used in ophthalmology. Approved for use from 1 month. The drug is instilled 4 times a day, 2 drops. The course of treatment is up to 2 weeks. Longer use is allowed as prescribed by a doctor. |
| Tobrex | The manufacturer recommends use in children over 1 year of age. But pediatric ophthalmologists prescribe these drops when Vitabact is ineffective. |
| Solution 0.25% Levomycetin | Has a broad antibacterial effect. The drug is prescribed for 2 weeks, 1 drop every 4 hours. Antimicrobial drugs, including Levomycetin, should be used as prescribed by a pediatric ophthalmologist or pediatrician. |
| Collargol | Approved for use in children under 1 year of age. The composition contains silver, an overdose of which is dangerous. This drug can only be used with a prescription. |
| Albucid | Safe for children, but not prescribed for newborns due to pain during the procedure. Drops can also crystallize, which can aggravate the problem. |
| Furacilin solution | Used to wash the eye and remove accumulated pus. Grind 1 tablet and dissolve in half a glass of water. |
If the drug must be stored in the refrigerator, then before use you should warm the drops in your hands or in a water bath.
Atresia of the lacrimal opening
Anonymous user
July 5, 2018
Hello! I always watch your shows. I never thought that I would ask a question. On January 13, 2021, my son was born. My husband and I have been waiting for him for 9 years. I have polycystic ovary syndrome, so everything was quite difficult. Conception occurred due to hormones. The baby is healthy. Well, the eyes immediately began to fester back in the family home. They wiped it with some kind of solution. Then, in response to complaints, the pediatrician told me to massage and wipe, and put in drops. A month at the ophthalmologist, they recommended the same massage procedure and Tobris drops for 10 days. As a matter of fact, I already understood that we had no passage of tear ducts. I read on the Internet that mothers are able to get it through by 6 months. the probing sounded terrifying. Well, I did massage for up to 5 months. Realizing that it doesn’t help, and bags appear under the eyes. The eyes also fester. I got scared and went back to the doctor. No one was examined there, based on my words, and based on the fact that there was a tear, we were sent for probing. There is no need to take paid tests. You just pay money, the doctor apparently doesn’t look either. The child is taken away and taken out within 10-15 minutes. So our child was taken away. Then everyone ran in. And they carried our baby out. The manager came out and said: “Your child doesn’t have a lacrimal punctum, we don’t see it - it needs to be done under anesthesia, and it’s not a fact that it will help, you may need to go to another city, since we are not omnipotent.” I'm confused. There is no certainty whatsoever. They didn’t conduct a normal examination, I’m talking about the test that they do. Nothing like this. Even at a paid consultation, in a private clinic, they simply pressed on the eye, thinking that pus should come out. Then two ophthalmologists looked at the equipment and summarized that we do not see lacrimal openings. And then in words, they did not give any documents. Of course, we collect documents for anesthesia and it is very scary to trust them with your child. Well, perhaps by the will of God, the operation becomes desperate, the tests are lost, or the child begins to sniffle. Based on the above, I have several questions: 1) is it possible to give anesthesia, the child is almost 6 months old and has water in his head, based on ultrasound! ? 2) what will they do to him under anesthesia? 3) can this procedure harm him? 4) what do they mean that not everything is in their hands and they may need to go to another city? 5) can they make a mistake with the diagnosis? 6) have there been cases in your practice where this kind of diagnosis was erroneous? , It passed on its own, maybe it’s still small and that’s why the lacrimal punctum is not visible? 7) how urgently does this procedure need to be performed or can it be postponed? If this procedure is not done at all, what could be the consequences? Please, help. Don’t put my questions on hold, the child is small and his future is at stake.
I always watch your shows. I never thought that I would ask a question. On January 13, 2021, my son was born. My husband and I have been waiting for him for 9 years. I have polycystic ovary syndrome, so everything was quite difficult. Conception occurred due to hormones. The baby is healthy. Well, the eyes immediately began to fester back in the family home. They wiped it with some kind of solution. Then, in response to complaints, the pediatrician told me to massage and wipe, and put in drops. A month at the ophthalmologist, they recommended the same massage procedure and Tobris drops for 10 days. As a matter of fact, I already understood that we had no passage of tear ducts. I read on the Internet that mothers are able to get it through by 6 months. the probing sounded terrifying. Well, I did massage for up to 5 months. Realizing that it doesn’t help, and bags appear under the eyes. The eyes also fester. I got scared and went back to the doctor. No one was examined there, based on my words, and based on the fact that there was a tear, we were sent for probing. There is no need to take paid tests. You just pay money, the doctor apparently doesn’t look either. The child is taken away and taken out within 10-15 minutes. So our child was taken away. Then everyone ran in. And they carried our baby out. The manager came out and said: “Your child doesn’t have a lacrimal punctum, we don’t see it - it needs to be done under anesthesia, and it’s not a fact that it will help, you may need to go to another city, since we are not omnipotent.” I'm confused. There is no certainty whatsoever. They didn’t conduct a normal examination, I’m talking about the test that they do. Nothing like this. Even at a paid consultation, in a private clinic, they simply pressed on the eye, thinking that pus should come out. Then two ophthalmologists looked at the equipment and summarized that we do not see lacrimal openings. And then in words, they did not give any documents. Of course, we collect documents for anesthesia and it is very scary to trust them with your child. Well, perhaps by the will of God, the operation becomes desperate, the tests are lost, or the child begins to sniffle. Based on the above, I have several questions: 1) is it possible to give anesthesia, the child is almost 6 months old and has water in his head, based on ultrasound! ? 2) what will they do to him under anesthesia? 3) can this procedure harm him? 4) what do they mean that not everything is in their hands and they may need to go to another city? 5) can they make a mistake with the diagnosis? 6) have there been cases in your practice where this kind of diagnosis was erroneous? , It passed on its own, maybe it’s still small and that’s why the lacrimal punctum is not visible? 7) how urgently does this procedure need to be performed or can it be postponed? If this procedure is not done at all, what could be the consequences? Please, help. Don’t put my questions on hold, the child is small and his future is at stake.
The question is closed
No reward
Probing
If after drug treatment and massage there is no result, the doctor will suggest probing. The decision to perform this procedure is made by a qualified ophthalmologist. You must first make sure that the mother’s massage technique was correct.
If there is no improvement within a month, the child is prepared for the probing procedure:
- Consultation with an otolaryngologist is required to exclude pathologies of the nasal septum.
- A general blood test is prescribed.
- Consultation with a pediatrician to exclude acute viral infections.
- You should not feed your baby 1 hour before the procedure to prevent regurgitation.
- The newborn is swaddled tightly so that he cannot interfere with the probing.
This method should be carried out in the first six months of the child; at an older age, the film becomes dense and difficult to tear. The procedure is not used in acute forms of the disease with a large amount of pus. Probing is carried out for 20 minutes. After the operation, the child is undergoing outpatient treatment.
The procedure consists of the following steps:
- A local anesthetic is applied, and the skin around the eye is treated with a disinfectant solution.
- A Sichel probe is inserted into the canal lumen to expand the canal.
- The Bauman probe passes into the Sichel probe.
- The first probe is removed.
- Using the second probe, the purulent plug is destroyed.
- The remains of the plug are washed out of the canal.
After the procedure, at the last stage, the disinfectant solution goes into the nose. To prevent repeated probing, it is necessary to avoid viral diseases for 2 months. The attending physician prescribes eye drops to prevent re-infection. Additionally, a massage is performed to consolidate the achieved results.
Probing the lacrimal canal in a child:
Diagnostics
The diagnosis of “dacryocystitis” is made after an external examination and anamnesis. Further examination includes:
- Vesta sample. A tampon is inserted into the nostril on the side where the inflamed lacrimal canal is located, and a collargol dye solution is instilled into the eye. If everything is normal with patency, then within a couple of minutes the tampon will be colored. If this does not happen after 10 minutes, the West test indicates that the tear duct is clogged.
- Probing. The study reveals damage to the lacrimal canaliculi.
- Bacterial culture of a smear from the nasolacrimal duct. Bacterial analysis is necessary to identify the infectious agent.
Laser surgery
In newborns, laser surgery is a gentle surgical intervention to restore the outflow of tear fluid into the nasal canal. This method is used for chronic, frequently recurring blockages of the tear duct. As a result, a new cavity is formed between the nose and the lacrimal sac.
For infectious diseases of the eye, this operation is not performed. Extranasal dacryocystomy is prescribed in childhood according to strict indications. Access to the lacrimal duct is through the nose.
During the operation, the following actions are carried out:
- Local anesthesia is applied to the areas that will be involved in the operation.
- An endoscope is inserted from the nasal passage, allowing you to monitor the progress of the operation on the monitor.
- Using a laser, an incision is made and a new passage is formed between the eye and nose.
- The mucous membrane is pressed with several sutures to prevent tissue overgrowth.
This method is characterized by high speed and the absence of cosmetic defects. Reduces the risk of injury. The hole has the optimal shape and size. The operation can be performed on both sides.
To treat dacryocystitis with a laser, modern equipment and highly qualified surgeons are required. If you are allergic to painkillers, surgery will not be possible.
Surgical intervention
Blocked tear ducts in newborns can be treated without surgery. But if conservative methods do not bring results, then they resort to surgical intervention. The method is effective for severe pathologies of the nasopharynx, curvature of the nose, partial or complete absence of the lacrimal canal.
The operation includes:
- Use of local anesthesia. Cotton swabs soaked in lidocaine are applied to the lacrimal cavity, nasociliary nerve and posterior ethmoidal nerve.
- The skin and soft tissues are incised.
- The periosteum is separated.
- Using a chisel, a bone window is formed.
- Use pliers to trim the edge.
- A direct passage into the nasal cavity is formed.
- The mucous membranes are pressed to the edges to prevent fusion.
Surgical intervention for blockage of the lacrimal canal is highly traumatic. The incision takes a long time to heal and may leave a scar. It is used in the absence of effective treatment by other means.
Traditional methods
In addition to medicinal methods of treatment, folk ones are used.
There are plants that have a positive effect on the tear duct plug:
Kalanchoe juice
For treatment, fresh Kalanchoe juice is diluted with saline in a 1:1 ratio. This plant relieves inflammation and has a disinfectant effect.
Before using Kalanchoe, you must properly prepare:
- To do this, clean leaves, wrapped in a piece of cotton, are left in the refrigerator for several days.
- After that, they are crushed and the juice is squeezed out.
- The prepared diluted solution is instilled 3 drops into each nostril. Sneezing after the solution increases the pressure in the tear duct and helps break through the film.
Eyebright
The plant is used for eye diseases. Reduces inflammation, has an antimicrobial effect and promotes healing.
Preparation and use:
- One tablet of the medicine is dissolved in 1 glass of boiled warm water. The product has no contraindications and can be used in newborns.
- To wash the eyes, the eyebright solution is mixed with chamomile infusion. Take 2 tbsp. l. dry collection of chamomile, pour a glass of boiling water and leave in a water bath for 10 minutes.
- After cooling, the chamomile infusion is mixed with the eyebright solution.
- Using cotton pads soaked in the solution, remove purulent discharge.
- The procedure is carried out before using eye drops and massage.
The prognosis for timely treatment of blockage of the tear duct is favorable. Conservative methods bring results on average within 2 months of treatment for a newborn. If there is no result for a long time, bougienage, laser or surgical intervention is used.
Author of the article: Mix Alena
Article design: Svetlana Ovsyanikova
Methods for studying the lacrimal ducts
The study of the lacrimal ducts in children must be carried out in the maternity hospital, and then throughout the first six months of life. In almost 5% of newborns, the nasolacrimal duct is closed by a gelatinous plug, which dissolves in the first days of life as a result of exposure to mucolacrimal fluid containing the enzyme lysozyme, and the path for lacrimal drainage is open.
However, in approximately 1% of newborns, this plug does not dissolve, but is organized into a connective tissue septum, as a result of which tear drainage becomes impossible. In addition, the cause of obstruction of the lacrimal ducts may be changes in each of their sections, as well as in the nose.
The first sign of pathology of the lacrimal ducts is constant lacrimation, and often lacrimation. In order to establish the cause or causes of lacrimation and lacrimation, it is necessary to consistently carry out a series of studies, starting with a simple visual determination of the position of the eyelids in relation to the eyeball.
Normally, the upper and lower eyelids are in contact with the eyeball, and thus the tear duct can be considered to be fully functioning. The presence of eversion, entropion, coloboma of the eyelids, lagophthalmos and other changes predominantly in the edges of the eyelids can cause lacrimation and lacrimation.
It is also very important to establish whether the newborn has lacrimal openings, how they are expressed and where they are located. To do this, it is necessary to slightly pull each eyelid at the inner corner of the palpebral fissure and determine the condition of each lacrimal punctum. If, in the normal position of the eyelids, the lacrimal openings are not visible and appear only when the eyelid is gently pulled back, then it means that they are positioned correctly. Normally, lacrimal puncta are clearly defined as a miniature funnel-shaped depression in the lacrimal tubercle.
By pressing a finger or a glass rod on the area of the lacrimal canaliculus with the eyelid retracted, check whether there is mucous or other discharge from the lacrimal openings. As a rule, there is no discharge from the lacrimal openings during this manipulation.
The next stage of the study is to determine the presence and functioning of the lacrimal sac. For this purpose, press the skin near the lower inner corner of the orbit with a finger or a glass rod, i.e., in the area of the projection of the lacrimal sac. In this case, the eyelid should be pulled away from the eyeball so that the lacrimal punctum is visible. If, when pressing on this area, there is no discharge from the lacrimal punctum or it is very scanty, transparent and liquid (tear), then it means there is a lacrimal sac. However, it is impossible to say with certainty that it functions well and has the correct location and dimensions. If during this manipulation there is abundant mucous or mucopurulent discharge from the lacrimal openings, then this indicates obstruction of the nasolacrimal duct. In those rare cases when, when you press on the area of the lacrimal sac, its contents come out not through the lacrimal openings, but through the nose (under the inferior nasal concha), one can think about the irregular structure and shape of the lacrimal sac and the patency of the bony part of the nasolacrimal duct.
Finally, the area of the inferior turbinate is examined and the condition of the nasal septum is determined. In addition, pay attention to the presence or absence (difficulty) of nasal breathing.
After visual-manual examinations, functional lacrimal and nasolacrimal tests should be performed. Functional tests are carried out in two stages.
- the first stage - assessment of the functioning of the lacrimal ducts from the lacrimal punctum to the lacrimal sac (Vest canalicular test),
- the second - from the lacrimal sac to the release of fluid from under the inferior turbinate (Vest's nasolacrimal test).
The Vesta nasolacrimal test is performed as follows. A loose swab of cotton wool or gauze is inserted under the inferior turbinate; 2-3 drops of a 1-3% solution of collargol or fluorescein are instilled into the conjunctival cavity; note the time of instillation and the time of disappearance of the dye from the conjunctival sac (normally it should not exceed 3-5 minutes). 5 minutes after instillation of the dye, every minute the swab is removed from the nose with tweezers and the time for the appearance of its staining is determined. The West nasolacrimal test is considered positive if staining of the tampon occurred in the first 7 minutes after installation of the dye, and weakly positive or negative if staining was noted later than 10 minutes or did not occur at all.
In cases where the canalicular or nasolacrimal West test, or both together, are slow or negative, diagnostic probing should be performed with a Bowman probe (No. 1). In the process of careful probing, either free patency of each section of the lacrimal duct is revealed, starting from the lacrimal punctum and ending with the bony part of the nasolacrimal duct, or an obstacle in any of the sections.
Before and after probing, the lacrimal ducts are washed. To do this, using a syringe and a blunt-ended straight or curved needle under pressure, a weak solution of an antiseptic, antibiotic, sulfonamide drug, isotonic sodium chloride solution, and lidase is injected through the upper (if necessary, through the lower) lacrimal opening. If the solution is excreted only through the nose, then this test is positive, if through both the nose and through the second lacrimal punctum, then it is weakly positive, and if only through the second lacrimal punctum, then negative. In cases where fluid is released from the same lacrimal opening, that is, does not pass through the tubules, the sample is considered sharply negative. In order to exclude the presence of an obstruction in the nasolacrimal duct in such cases, retrograde sounding is performed together with an otolaryngologist. Finally, in order to finally establish the location and extent of the pathology of the lacrimal ducts, an X-ray examination should be performed.
Iodolipol is used as a contrast agent, which is administered through the lacrimal openings, after which an x-ray is taken. The X-ray contrast picture reveals strictures and diverticula, obstruction of various parts of the lacrimal canaliculi, lacrimal sac, and the bony part of the nasolacrimal duct. Only after consistently carrying out all diagnostic studies can a correct diagnosis be made and an adequate method of treatment be selected (bougienage, probing, reconstructive surgery on the lacrimal ducts, in the nose).
Due to the fact that the pathology of the lacrimal organs consists not only of impaired lacrimal drainage, but also of changes in the tear-producing apparatus (lacrimal gland), you need to know that dysfunction of the lacrimal gland can be judged by the indicators of the Schirmer test. The essence of this test is that a strip of filter paper 0.5 cm wide and 3.5 cm long is placed behind the lower eyelid for 3-5 minutes. If all the paper becomes homogeneously moist during this time, this indicates normal functioning of the gland. if it is faster or slower, then it means that its hyper- or hypofunction is noted, respectively.