Causes
Dacryocystitis precedes phlegmon in most cases. First, the nasolacrimal duct becomes blocked. At the same time, increased proliferation of bacteria begins in the lacrimal sac, which leads to inflammation. Dacryocystitis is manifested by the following symptoms:
- pain in the eye, radiating to the nose and jaw;
- swelling and redness in the inner corner of the eye;
- increased lacrimation;
- deterioration of vision.
With insufficient treatment, suppuration forms at the site of inflammation. The contents break through the wall of the lacrimal sac and spread through the subcutaneous tissue. This is how phlegmon is formed. The patient's condition deteriorates sharply.
However, phlegmon of the lacrimal sac occurs not only due to dacryocystitis. The cause of suppuration in the tissue can be diseases of the nasal sinuses - sinusitis and sinusitis. In this case, the infection enters the eye area through the nasolacrimal duct.
The causative agents of phlegmon of the lacrimal sac are various bacteria: staphylococci, pneumococci, streptococci, etc. The disease is usually preceded by a decrease in immunity.
Pathogenesis
Normally, the tear fluid produced by the lacrimal glands washes the eyeball and flows to the inner corner of the eye. It is there that the so-called lacrimal openings are located, which lead to the lacrimal canaliculi. If there is no pathology, the tear first enters the lacrimal sac, and then through the nasolacrimal duct into the nasal cavity. If the nasolacrimal duct is obstructed, the lacrimal drainage process is disrupted and tears accumulate in the lacrimal sac. This is a cylindrical cavity that is located at the top of the nasolacrimal duct. When tears stagnate, the lacrimal sac becomes infected, which leads to the development of inflammation in it.
Symptoms
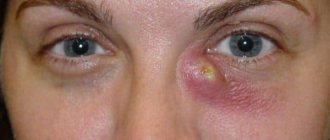
With phlegmon, the patient's general condition sharply worsens. Weakness, malaise appears, and the temperature rises. Severe swelling occurs, which spreads from the lacrimal sac area to the eyelid, nose, and cheek. The skin on the affected area turns red and becomes hot to the touch. In the area of the lacrimal sac, severe pain is felt and a compaction is palpated. This stage of the disease is called infiltrative.
After a few days, the fluctuation stage begins. The affected area becomes soft. At this stage, an abscess forms. The skin takes on a yellowish tint due to the accumulation of pus.
An abscess may break through the skin on its own. This creates a wound that heals over time. After this, all unpleasant symptoms subside. However, one should not count on such a successful outcome. Without treatment, cellulitis can lead to serious complications.
In addition, suppuration can break through the nasal cavity. In this case, a fistula is formed in the duct, through which tear fluid flows through the nose. Often, long-term non-healing fistulas form on the skin.
Tests and diagnostics
- To correctly establish a diagnosis, the doctor conducts a survey of the patient or the child’s parents and a detailed external examination, determining the presence of typical symptoms of the disease.
- The doctor also palpates the inflamed area - in the case of dacryocystitis, the inflamed area is painful, purulent contents are released from the lacrimal openings.
- Vesta color testing is also carried out. Its essence is that a dye is dripped into the patient’s eye, and a tampon is inserted into the nasal cavity. Normally, after five minutes, traces of paint should appear on the tampon.
- A contrast test is practiced. It requires local anesthesia. After this, the patient is given a drop of fluorescein . After 10 minutes, the doctor examines the eye in the light of a blue lamp. Normally, only a little fluorescein .
- X-rays of the lacrimal ducts are also performed. For this, a special radiopaque substance is used, which allows one to visualize the pathways and determine the level of duct occlusion.
- The doctor can conduct a laboratory test of the discharge to determine the pathogen and its sensitivity to antibiotics .
Features of the disease in infants
As already mentioned, phlegmon of the lacrimal sac is often observed in infants. In some newborns, the nasolacrimal duct is closed by a gelatinous plug or embryonic membrane. These formations in most cases resolve on their own in the first months of life. If this does not happen, the baby may develop dacryocystitis. With insufficient or improper treatment, the disease is complicated by phlegmon.
With dacryocystitis, a child experiences redness of the eyes, yellowish-green discharge, and swelling in the area of the lacrimal sac. When light pressure is applied to the swollen area, pus is released. If the disease is complicated by phlegmon, then the baby’s general health sharply worsens, the temperature rises, and swelling around the eye increases. The baby stops eating and becomes restless.
Diagnostics
The diagnosis of cystitis is made based on the typical picture of the disease, characteristic diseases, external examination data and palpation of the lacrimal sac. When examining a patient with dacryocystitis, ruptures and swelling in the gas zone are revealed; upon palpation of the inflamed area, pain and purulent discharge from the avulsion points are determined. The test for patency of the tear ducts in cystitis is carried out using the Western (tubular) test. To do this, a tampon is inserted into the corresponding nasal passage, and the colargol solution is instilled into the eye. In the case of patent tear ducts, traces of dye should appear on the tampon within 2 minutes. For longer swab staining times (5-10 minutes), the patency of the rupture can be doubted; If colargol is not cleared from the body within 10 minutes, the vest test is considered negative, indicating tear duct obstruction. To find out the extent and extent of the damage, a diagnostic examination of the tear ducts is performed. Passive analysis of nasal tearing in dacryocystitis confirms the blockage of the tear ducts: in this case, the fluid does not enter the nose when rinsing the tear duct and nasal canal, but flows through the tear openings. Biomicroscopy of the eye is used in the complex of ophthalmological diagnostics of dacryocystitis and fluorescein instillation test. Contrast radiography of the tear ducts (dacryocystography) with iodolipol solution is necessary in order to obtain a clear picture of the architecture of the tear ducts, the location of the stricture or the area of obliteration. To identify microbial pathogens of dacryocystitis, secretions from lacrimal openings are examined through bacteriological culture. To clarify the diagnosis, a patient with dacryocystitis should be examined by an otolaryngologist with rhinoscopy; According to indications, consultations with a dentist or maxillofacial surgeon, traumatologist, neurologist, or neurosurgeon are planned. Differential diagnosis of dacryocystitis is carried out with canaliculitis, conjunctivitis, erysipelas.
Consequences of the disease
Cellulitis is a serious disease that requires immediate treatment. Otherwise, serious consequences and complications may occur:
- Pus may rupture into the sinuses. In this case, the patient develops sinusitis or sinusitis. This is the most common and not the most severe complication of phlegmon.
- A more dangerous consequence is the spread of phlegmon to the orbital area. In this case, damage to the optic nerve and internal structures of the eye is noted. Panophthalmitis occurs. This is an extensive purulent inflammation of all tissues of the eyeball. This disease can lead to blindness or amputation of the organ of vision.
- It is important to remember that the lacrimal sac is located close to the brain. Penetration of infection from the organ of vision into the cranial cavity can lead to meningoencephalitis. This disease often ends in death.
General information
The diagnosis of “ dacryocystitis ” is made if the patient has an inflamed lacrimal sac located in the area between the nose and the inner corner of the eyelids.
Dacryocystitis, whose ICD-10 code is H-04, usually develops as a result of obstruction of the nasolacrimal duct, which conducts lacrimal fluid into the nasal cavity. Pathogenic microorganisms accumulate in the sac, as a result of which inflammation of the lacrimal sac develops. The process can be acute or chronic. This pathology develops mainly in children and accounts for about 10% of all eye diseases. This is due to the peculiarities of the development of the lacrimal ducts during intrauterine maturation of the fetus, as well as other reasons. Since the disease occurs quite often, it is important for parents to know how to recognize its onset in their baby and what to do next to prevent the problem from getting worse. But adults also face the same problem: dacryocystitis is also diagnosed in people of working age. The features of this disease and its treatment will be discussed in this article.
Treatment
Emergency assistance for phlegmon of the lacrimal sac should be provided immediately. However, only a specialist can treat such a disease. It is necessary to take the patient to an ophthalmologist as soon as possible.
Treatment of the disease is carried out in a hospital setting. At the infiltrative stage, conservative treatment of phlegmon of the lacrimal sac is indicated. Antibiotic injections are prescribed:
- "Cefazolin";
- "Ampicillin";
- "Ceftriaxone".
Treatment is supplemented with local application of eye drops with antibiotics and sulfonamides. The following drugs are prescribed:
- "Floxal";
- "Tobrex";
- "Vitabact";
- "Levomycetin";
- Vigamox.
To relieve pain and inflammation, the use of corticosteroid eye drops with dexamethasone is indicated. At the same time, physiotherapeutic procedures are prescribed: UHF, electrophoresis with antibiotics, blue light treatment.
After the abscess enters the fluctuation stage, the phlegmon of the lacrimal sac is opened. Under local anesthesia, an incision is made in the affected area. The purulent cavity is washed with antiseptic solutions, and then drainage tubes are placed to drain the contents. A bandage is applied to the wound.
In the first days after surgery, the bandages are changed several times a day. Antibacterial ointments are applied to them. Subsequently, dressings are carried out once every few days. Antibiotics are prescribed in the form of tablets or injections. In the first time after opening the abscess, the patient needs complete rest. The recovery period after surgery is no more than 1 month.
After all acute manifestations have subsided, the patient is offered to undergo surgery to restore the patency of the nasolacrimal duct. This helps prevent relapses of the pathology. For children, such surgical intervention is performed no earlier than 5-7 years.
Complete removal of the lacrimal sac is very rare these days. This operation has unpleasant consequences: the patient experiences constant lacrimation. Therefore, such surgical intervention is resorted to only in very advanced cases.
Cellulitis of the lacrimal sac
Signs
With phlegmon of the lacrimal sac, the skin in the area of the eye, eyelid, nose and cheek on the side of the affected eye turns red and swells so much that the palpebral fissure narrows or even closes.
In this case, you can feel a compaction above the lacrimal sac, which is painful on palpation and hot to the touch. This process is accompanied by increased body temperature, headache, and weakness. After a few days, the compaction becomes softer and fluctuation appears in it (accumulation of fluid, in this case pus). The skin over the lump turns yellow. Soon the abscess opens through the skin, and after this the inflammation subsides. After some time, the abscess hole closes. However, a fistula (a channel connecting the cavity to the surface of the body) may also form, through which pus and tear fluid continue to be released. Sometimes the abscess opens into the nasal cavity through the nasolacrimal canal. In this case, an intranasal fistula may subsequently form (an artificial opening through which any fluids located in the body cavity are removed).
Description
Cellulitis of the lacrimal sac is an infectious disease caused by staphylococci, pneumococci, streptococci and other microorganisms. It usually develops as a complication of chronic purulent dacryocystitis. However, sometimes it can be caused by inflammation of the nasal cavity, as well as the paranasal sinuses - the maxillary cavity or the ethmoid labyrinth.
The disease progresses rapidly, but if treatment is started in a timely manner and carried out correctly, the inflammatory process can be stopped at the very beginning and prevent purulent-necrotic tissue breakdown and the formation of an abscess.
Self-healing of phlegmon of the lacrimal sac often occurs. This happens if, in the process of melting the lacrimal sac, its complete obliteration occurs (cavity closure). However, there is no need to allow such “self-healing” to occur, since in this case the lacrimal drainage function is completely disrupted.
Complications of phlegmon of the lacrimal sac are possible. The most common of them is the spread of inflammation to the paranasal sinuses. However, this is not the most dangerous complication. The most dangerous, and, fortunately, the rarest thing is phlegmon of the orbit. In this case, not only the orbit itself is affected, but also the optic nerve and the inner membranes of the eye. In this case, the development of panophthalmitis is possible, which leads either to a severe deterioration (almost disappearance) of vision, or to the removal of the affected eye. In addition, with phlegmon of the orbit, inflammation can spread to the membranes of the brain. And in this case, even death is possible.
First aid
When the first symptoms of the disease appear, you should immediately contact an ophthalmologist.
Diagnostics
Diagnosis of phlegmon of the lacrimal sac is carried out on the basis of the characteristic picture of the disease, the patient’s complaints, examination data and palpation of the lacrimal sac area. In addition, it is necessary to take an x-ray of the orbit and paranasal sinuses.
Treatment
For phlegmon of the lacrimal sac, antibiotics are prescribed intramuscularly and orally (by mouth), and anti-inflammatory drugs. Doses and duration of treatment depend on the patient's condition.
Frequent, at least 4 times a day, instillations of antibacterial solutions and corticosteroid drugs to relieve inflammation are prescribed locally. Physiotherapy - UHF and blue light on the affected area has a good effect.
If an abscess has already formed, it is opened, pus and necrotic tissue are removed, the cavity is washed with antiseptic solutions, antibiotic powder is poured into it and a bandage is applied.
After the inflammation subsides, dacryocystorhinostomy is performed - reconstruction of the duct from the lacrimal sac into the nasal cavity. This is done to restore the outflow of tear fluid into the nasal cavity. If this manipulation is not carried out, relapses of the disease are possible.
The prognosis with timely and correct treatment is favorable.
Prevention
Prevention of phlegmon involves timely treatment of dacryocystitis and stenosis of the nasolacrimal canal.
© Dr. Peter
Prevention
The main method of preventing phlegmon is timely treatment of dacryocystitis. Symptoms such as pain in the eyeball, watery eyes, swelling and redness in the corner of the eye, and blurred vision cannot be ignored. In the early stages, dacryocystitis responds well to treatment, and surgery can still be avoided. It is also necessary to treat sinusitis and other sinus diseases in a timely manner.
Particular attention should be paid to the treatment of dacryocystitis in young children. Symptoms of inflammation of the lacrimal sac in a child may resemble signs of conjunctivitis. Parents often self-medicate and wash their baby’s eyes with tea leaves. This only leads to aggravation of painful manifestations, and subsequently dacryocystitis develops into phlegmon. Therefore, in case of persistent eye inflammation in children, it is necessary to urgently contact an ophthalmologist.