Fuchs syndrome (endothelial corneal dystrophy, Fuchs dystrophy, Fuchs spot) is a pathology characterized by the death of cells in the lower layer of the cornea. The disease develops gradually, most often one eye is affected, less often both eyes.
This disease is also called heterochromic Fuchs cyclitis, although heterochromia (different color of the iris in the left and right eyes) is not always present.
Clinic
It usually occurs in one eye and includes three mandatory symptoms:
- • protein precipitates on the cornea;
- • change in iris color;
- • clouding of the lens.
As the process progresses, other symptoms appear - anisocoria (different pupil widths) and secondary glaucoma.
The patient's friends and relatives are the first to detect signs of illness: they notice the difference in the color of the iris of the right and left eyes, then they pay attention to the different width of the pupils. The patient himself, aged 20-40 years, complains of decreased visual acuity when clouding of the lens occurs. The main manifestation of the pathology is a different color of the iris of the eyes or unequal coloring of its different areas, in which it looks lighter or, conversely, darker. Difficulties in identifying this sign are caused by brown eye color, in which it is manifested to a minimal extent. The progression of the disease occurs slowly: over several years in the absence of symptoms; therefore, in the initial stages it is diagnosed accidentally. This occurs if the patient seeks help from an ophthalmologist due to increased IOP or clouding of the cornea, which are a complication of Fuchs syndrome.
Stages of the disease:
| Stage | Characteristic symptoms |
| First | There are no subjective symptoms, but objective symptoms consist of the appearance of small accumulations of particles of pigment epithelium and other cells that do not affect the sensitivity of the cornea. |
| Second | The process begins to manifest itself as cloudiness, the formation of a veil before the eyes, interfering with normal vision. Patients note a decrease in visual acuity, and the ophthalmologist notes the appearance of larger clusters and further destruction of pigment along the edges of the pupil. |
| Third | Due to the large number of accumulations, the sensitivity of the cornea is significantly reduced, dystrophy of the iris develops, and pigmentation clearly manifests itself in the area of the angle of the iris. Patients note increased IOP, visual disturbances, and clouding of the cornea. |
The main symptom of Fuchs syndrome is heterochromia of the iris. In this case, the iris of the affected eyeball looks lighter. In patients with brown eyes, this clinical sign is less pronounced. In patients with light eyes, reverse heterochromia may develop, which is associated with the visualization of the pigment layer of the iris during destruction of the anterior stroma. The disease progresses slowly and has no other clinical manifestations for several years. Uveitis with Fuchs syndrome is not accompanied by hyperemia, photophobia and pain. As a rule, patients seek help from a specialist due to the development of a clinical picture of complications - cataracts or glaucoma.
The appearance of small translucent precipitates on the cornea is not accompanied by injection of the eyeballs and closure of the anterior chamber angle. A gradual progression is observed. At the initial stage, a small number of small precipitates appear that do not affect the sensitivity of the cornea. The second stage of Fuchs syndrome is characterized by dissemination of the process. In this case, small and medium-sized precipitates lead to the appearance of cloudiness before the eyes with further destruction of the pigmented pupillary border. Patients complain of decreased visual acuity and constant dilation of the pupil.
At the third stage of Fuchs syndrome, the sensitivity of the cornea is significantly reduced. A large number of precipitates of different sizes leads to degeneration of the iris and pronounced pigmentation in the area of the angle of the anterior chamber of the eye. Small formations appear on the anterior surface of the iris - Russell bodies, the occurrence of which is associated with the aggregation of immunoglobulins. The most common complications of Fuchs syndrome are glaucoma, posterior subcapsular cataract, and ocular hypertension.
Myopia and the causes of retinal dystrophy
Ocular myopia is a common condition that causes abnormal refraction of the eyes. The pathology is usually called myopia, because the patient can hardly distinguish between objects located in the distance, but sees objects located nearby well.
With the development of myopic disease, serious degenerative changes occur in the retina. Central or peripheral chorioretinal dystrophy often develops, but sometimes these types of pathology can be combined.
When the macular area is affected, the form of the disease can be dry or wet.
The first involves the formation of fibrosis, while extravasation and neovascularization of the retina are absent. Degenerative changes often occur in young people, and myopia will often be less pronounced.
The wet form is characterized by transudative changes in the posterior retina. The patient develops a fibrous transudate or hemorrhage. Such changes occur due to pathology of Bruch's membrane or due to subretinal neovascularization.
Degenerative changes contribute to a gradual decrease in a person’s vision. But sometimes, due to fibrotic or hemorrhagic processes, the patient experiences a significant deterioration in this function.
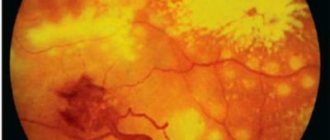
Fuchs' black spot appears at the site of hemorrhagic or fibrous lesions due to proliferation of the pigment epithelium.
The essence of pathology
Diagnostics
- Corneal precipitates
are a characteristic pathognomonic sign. They are small, round or star-shaped, gray-white in color and cover the entire endothelium of the cornea, they can appear or disappear, but do not merge and are not pigmented. Among the corneal precipitates, delicate fibrin fibers are found.
- The opalescence of the aqueous humor
is weak, the number of cells is up to +2.
- Cellular infiltration of the vitreous body
may be the leading symptom of the disease. - Gonioscopy
is unchanged or one of the following is determined: Small radially located vessels, similar to twigs, in the corner of the anterior chamber. They cause the formation of hemorrhages in the anterior chamber on the side opposite the puncture (Amsler's sign). - Membranes in the corner of the anterior chamber.
- The anterior synechiae are small and irregularly shaped.
All symptoms of Fuchs syndrome are caused by progressive atrophy of the stroma of the iris and ciliary body.
The thinned outer layer of the iris becomes lighter, and the lacunae become wider than on the fellow eye. The pigment layer of the iris begins to shine through them. By this stage of the disease, the affected eye is already darker than the healthy eye. The dystrophic process in the processes of the ciliary body leads to changes in the walls of the capillaries and the quality of the produced fluid. Protein appears in the moisture of the anterior chamber, settling in small flakes on the posterior surface of the cornea.
Precipitate rashes may disappear for a period of time and then reappear. Precipitates have a characteristic appearance: they are delicate, star-shaped, with thread-like deposits visible between large precipitates. Precipitates occupy the entire posterior surface of the cornea (unlike the picture in other anterior uveitis, when precipitates are located in the lower half of the cornea and, as a rule, have the shape of a triangle, with the base facing downwards).
Despite the long-term existence of the precipitation symptom for several years, posterior synechiae do not form in Fuchs syndrome. A change in the composition of the intraocular fluid leads to clouding of the lens. Secondary glaucoma develops.
Usually the disease is unilateral, but in 7-15% of patients it is bilateral. In the latter case, it is difficult to determine heterochromia of the irises. Biomicroscopic examination reveals blurred structures of the iris. Rubeosis of the iris is sometimes detected. In rare cases, pain or redness of the eye may occur.
Correct diagnosis of the disease requires comprehensive studies, which, if present, reveal the following signs:
- manifestations of heterochromia of the iris of varying degrees - during physical examination;
- the presence of accumulations of particles of pigment epithelium and other cells of various sizes (depending on the stage), pathological nodules on the surface of the iris and on the periphery of the pupil - biomicroscopic studies;
- pathological changes in the structure of the iris - ultrasound scanning;
- decreased sensitivity of the cornea - algesimetric research method;
- minor or serious increases in IOP with the development of secondary glaucoma - tonometry;
- decreased visual acuity - visometry.
Diagnosis of Fuchs syndrome is based on the results of external examination, biomicroscopy, gonioscopy, keratoesthesiometry, tonometry, visometry, and B-mode ultrasound. During an external examination, the severity of heterochromia of the iris is determined, which varies from doubtful to clearly expressed. As a rule, questionable results or absence of heterochromia are observed in patients with binocular lesions.
The biomicroscopy method makes it possible to identify corneal precipitates, the size of which depends on the stage of Fuchs syndrome. They look like delicate translucent formations, which in rare cases contain pigment inclusions. In 20-30% of patients, mesodermal Boussac nodules are detected on the surface of the iris, and Koeppe nodules are detected along the edge of the pupil. An ultrasound scan of the eye in B-mode indicates focal or diffuse changes in the structure of the iris. Precipitates in Fuchs syndrome are visualized as hypoechoic formations.
With keratoesthesiometry (corneal algesimetry), a decrease in its sensitivity is determined. When diagnosing the angle of the anterior chamber of the eye using gonioscopy, as a rule, it is open, has an average width, and in rare cases is narrower than normal. The development of secondary (dystrophic) glaucoma in Fuchs syndrome leads to a gradual narrowing of its lumen with further closure.
Intraocular pressure (IOP) during tonometry is normal or slightly increased. The addition of secondary glaucoma is accompanied by an increase in IOP above 20 mm. Hg Art. Invasive interventions (gonioscopy, surgery, contact tonometry) may be accompanied by the development of thread-like hemorrhage from the anterior chamber angle, which is associated with a sharp decrease in IOP. The occurrence of complications of Fuchs syndrome (cataracts, glaucoma) leads to a decrease in visual acuity, which is detected during visometry.
Iris changes
The iris also changes.
- After cataract removal, posterior adhesions appear.
- The volume of the iris stroma decreases, there is no crypt (slit-like groove on the iris), the color of the iris becomes pale and dull. The radial vessels of the iris bulge due to loss of supporting tissue.
- Using retroillumination, patchy atrophy can be detected on the posterior pigment layer.
- Nodules form on the iris.
- Newly formed vessels appear.
- Pupil dilation (mydriasis) is observed due to atrophy of the muscle responsible for its narrowing.
- Crystal deposits in the iris are rare.
- Heterochromia of the iris is an important symptom.
Treatment
Treatment tactics for Fuchs syndrome in ophthalmology are determined based on its stage, severity of complications and individual indications of patients.
| Syndrome stage | Treatment methods |
| I | There are no clinical manifestations, no treatment is carried out. It is possible to correct eye color using colored lenses. |
| II, III | Efforts are directed towards eliminating degenerative processes by stimulating trophism. For this, the patient is prescribed medication:
|
If the patient has developed cataracts, drug treatment is carried out, and if there are no results, they resort to surgical techniques - phacoemulsification with IOL implantation.
- Dexamethasone, 0.1% solution, into the conjunctival sac 1-2 drops 3-4 times/day, 10-15 days
- + (with increased intraocular pressure) Timolol, 0.25-0.5% solution, into the conjunctival sac 1-2 drops 2 times a day.
In the absence of effect from therapy aimed at reducing intraocular pressure, surgical treatment is performed. Cataract removal is usually not difficult.
Long-term use of glucocorticosteroids increases the risk of developing lens opacities and increased intraocular pressure[1]
Treatment tactics for Fuchs syndrome depend on the stage of the disease and the severity of secondary complications. At the initial stage, specific treatment is not indicated. Eye color correction is carried out using cosmetic colored contact lenses. At the second and third stages of the disease, local and systemic dedystrophic therapy is recommended, aimed at improving trophic processes. The treatment complex for Fuchs syndrome includes angioprotectors, nootropics, vasodilators and vitamins. If a large number of precipitates are formed, the course of treatment must be supplemented with corticosteroids for local use in the form of drops and enzyme therapy.
With the development of secondary posterior subcapsular cataract in the initial stages against the background of Fuchs syndrome, drug treatment is indicated. If there is no effect, microsurgical intervention is recommended, consisting of phacoemulsification of the cataract followed by implantation of an intraocular lens. The occurrence of secondary glaucoma is an indication for the prescription of local antihypertensive therapy in parallel with the main course of treatment for Fuchs syndrome.
Characteristics of Fuchs pigment spot
When such a deviation occurs, there is always an unfavorable prognosis. After all, there is a danger that central vision may be completely lost.
This pathology is a pigment lesion located inside the macula. Almost always, the deviation occurs after hemorrhage in the macula among people suffering from a high degree of myopia. Such a pigmented neoplasm serves as a sign of the appearance of a new specific membrane when pathological blood vessels that have ruptures begin to grow inside the retina.
The main symptom of the development of a deviation is the appearance of distorted lines (straight lines) located near the central fossa. A few days after the hemorrhage, these lines take on the appearance of well-defined spots, resulting in the formation of a pigmented scar. As a result, a person's central vision will deteriorate and its acuity will be significantly reduced.
The timing of the formation of a molecular Fuchs spot may vary. Sometimes this pathological deviation develops over several years, and in some cases, on the contrary, very quickly. In the second case, the impetus for pathology is severe hemorrhage.
If the disease progresses slowly, under the influence of changes in the molecular area, metamorphopsia appears (lines and objects begin to bend). The result of the disorder is a noticeable deterioration in vision or its complete loss (in the central region), and sometimes a central scotoma occurs (damage to the optic nerve).
Causes
Sometimes, even if patients have a Fuchs' spot, there is improvement. However, visual acuity is restored by approximately 0.1.
As a result of degeneration of the yellow nucleus, only the central field of vision is always affected. However, such blindness will not cause the patient to lose his ability to work. This is explained by the fact that a person, despite central blindness, can do without the help of strangers, because he is able to see objects through lateral vision.
Sometimes, due to bleeding of the choroid, disruptions in the blood supply to the retina begin. If it is this kind of bleeding that causes the degeneration of the yellow nucleus, it is important to take care of reducing the flow of blood.
Fuchs' spot on fundus photograph
Prognosis and prevention
Specific prevention of Fuchs syndrome has not been developed. Patients with this pathology need to be examined by an ophthalmologist twice a year with mandatory biomicroscopy, gonioscopy, visometry and tonometry for the purpose of early prevention and diagnosis of secondary complications such as cataracts and glaucoma. It is also recommended to correct the diet with the inclusion of a large amount of vitamins, normalize sleep and rest patterns. The prognosis for life and work ability in Fuchs syndrome is often favorable. For a long period of time, the disease has a latent course, but in the case of secondary cataracts or glaucoma, complete loss of vision with subsequent disability is possible.[2]
Fuchs syndrome
Fuchs syndrome or heterochromic uveopathy is an anterior non-granulomatous uveitis characterized by a chronic, slowly progressive course. The classic symptoms of uveal heterochromia were first described in 1906 by the Austrian ophthalmologist Ernst Fuchs. The author believed that the development of the syndrome was due to paralysis and exposure to unknown toxic substances on the body. Individual manifestations of this disease were described in 1843 by the English ophthalmologist J. Lawrence. Fuchs syndrome has a slight prevalence in ophthalmology (4% of the total number of all uveitis). In 90-92.2% of cases, the disease develops monocularly. Pathology occurs with equal frequency among males and females. As a rule, uveal heterochromia occurs at the age of 20-60 years, the peak incidence of Fuchs syndrome occurs at 40 years.