Retinitis is an inflammation of the retina of the eyeball. Both men and women are susceptible to the disease. In most cases, the retina is affected simultaneously with the choroid. This is due to the fact that they fit tightly together. Simultaneous inflammation of the choroid and retina of the eyeball is called chorioretinitis. Due to the absence of pain receptors, the disease is not accompanied by pain.
Retinitis is classified into two types: internal and external. The first include diseases that occur as a result of infection or as a result of an autoimmune reaction. The second are inflammations that occur when the eyeball is injured and exposed to radiation. The most common are internal retinitis.
The spread of the inflammatory process can be of two types:
- Focal. When scar tissue forms around the site of inflammation, preventing the spread of inflammation.
- General. Retinitis spreads in the absence of scar tissue around the lesion. In an advanced stage, the disease progresses to chorioretinitis.
What it is?
Coates' retinitis affects between 1 and 9 people per 100 thousand of the world's population. About 78% of the cases are men. Typically, the onset of the disease occurs in the first 10-16 years of life. Most often, the onset occurs in children 5-8 years old, although it can occur at any age.
Coats disease is characterized by abnormal development of blood vessels that penetrate the retina, the inner lining of the eye.
This is expressed by the following pathologies:
- Telangiectasia , that is, dilation of the fundus capillaries.
- Exudation , or disruption of the permeability of the capillary walls. At the same time, exudate passes through the walls of the vessels - blood plasma with substances harmful to the eyes.
Cholesterol penetrates into the visual organs with exudate. It settles and accumulates in the fundus of the eye, which leads to retinitis - inflammation of the fundus of the eye. In the long term, this causes retinal separation and blindness. Because of the processes that occur in Coats disease, it is also called exudative retinitis and retinal telangiectasia.
Reasons for development
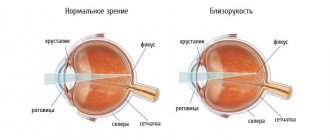
Important visual functions are performed by the retina of the eye. Visual acuity, color perception, and vision in the dark depend on it. When the retina is damaged, these indicators decrease.
Retinitis occurs as a result of infection from other organs that are inflamed. There are several causes of retinitis under the influence of external factors:
- Trauma to the eyeball. The disease can occur as a result of injury that damages the retina.
- The effect of ionizing rays on the eyes for a long time.
- Ultraviolet light regularly exposed to the eyes.
Nature and mechanism of the disease
The disease is idiopathic in nature, that is, its causes are still unknown. It is believed that it is not inherited, but is of a teratogenic nature - it begins during embryonic development.
The risk of exudative retinitis in the fetus increases when the following factors affect the pregnant woman’s body:
- drugs;
- ionizing radiation;
- alcohol;
- herpes zoster;
- rubella;
- toxoplasmosis.
Patients and their loved ones should learn about the mechanism of development of the disease. The main role in this process is given to polymorphic, that is, multiple, disruption of the structure of the eye capillaries. The initial defect lies in the endotheliocytes of the blood-retinal barrier. These are the cells of the layer that covers each vessel of the fundus and is responsible for the permeability of the capillary walls. Normally, only harmless substances that nourish the eye penetrate into the retina through the hemato-retinal filter.
IMPORTANT! The defective barrier allows too much blood to pass through. Along with it, large lipid molecules enter the eye.
The anomaly leads to hemorrhagic syndrome, which is characterized by frequent hemorrhages in the fundus.
This has the following consequences:
Lipid-containing macrophages and cholesterol crystals that enter the eye accumulate in and behind the retina and form exudative lesions. The first of them arise near the optic nerve and in the central part of the fundus.- The lesions become yellowish-golden and lose their outline. They cause chorioretinitis - inflammation of the retina and choroid. The affected tissues swell.
- Lipid lesions gradually merge into a massive exudative layer, which leads to retinal detachment.
- The exudate penetrates the vitreous body. It becomes cloudy and yellowish-white.
- The lipid layer absorbs and clouds the lens.
As the disease progresses, vision deteriorates, which over time leads to glaucoma, blindness, and then loss of the eye.
Stages of pathology
Pathology develops in stages. Scientists identify the following stages of the disease:
ARTICLES ON THE TOPIC:
- Inflammation of the retina or retinitis: symptoms and treatment of severe pathology,…
- How to recognize and treat retinoblastoma in children and adults - cancer symptoms...
- Diagnosis of retinal angiopathy in a child: what it is, symptoms and treatment...
- initial;
- developed;
- far gone;
- terminal.
The initial stage is difficult to recognize, but only at this stage can Coats disease be treated.
Initially, the disease manifests itself as follows:
- Mild hyperemia of the sclera occurs. The redness is explained by the fact that the small capillaries of the fundus are abnormally enlarged.
- Trying to focus on an object, the patient notices distortions and spots that are not really there.
- Vision decreases slightly, the outlines of visible objects become less clear.
When the disease reaches the second stage, the patient's vision declines sharply.
This stage is characterized by the following manifestations:
- Hemorrhagic syndrome progresses. At the same time, the abnormal vessels continue to enlarge and eventually merge into nodules.
- Detachment of the affected areas of the fundus begins.
In the third stage, absolute retinal detachment gradually develops, and the eye ceases to see. Subretinal inflammation leads to rubeosis, a condition where newly formed vessels appear on the iris. At this stage, cataracts and glaucoma occur.
In the terminal stage of fundus telangiectasia, total retinal detachment occurs. The affected organ atrophies and must be removed.
Treatment[ | ]
In the early stages, there are several treatment options. Laser surgery or cryotherapy (freezing) can be used to destroy abnormal blood vessels, thereby stopping the progression of the disease. However, if leaking blood vessels cluster around the optic nerve, this treatment is not recommended, as accidental damage to the nerve itself can lead to permanent blindness. Although Coats disease tends to progress to the point of vision loss, progression may stop on its own, temporarily or permanently. Cases have been reported in which the condition has reversed itself. However, if a total retinal detachment occurs, most vision loss is permanent. Removing the eye (enucleation) is an option if pain or further complications occur.
Symptoms of exudative retinitis
Coats disease usually affects one eye, and only 11% of total cases affect both eyes. Most often it can be recognized using a photo. The disease is indicated by a yellowish glow in the pupils of a person in the frame, similar to the effect of red eyes. It occurs due to cholesterol deposits.
The onset of exudative retinitis is also indicated by the following symptoms:
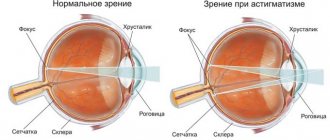
- The patient's vision is rapidly deteriorating. It all starts with mild astigmatism. Upper peripheral vision is affected first, then central vision.
- The world becomes a little blurry. The patient's vision is clouded by a slight haze.
- The perception of volume and depth of the image is impaired.
- Objects in the field of view appear somewhat distorted.
The disease progresses painlessly. The patient and his environment often do not pay attention to the first manifestations of the disease.
IMPORTANT! In addition to yellow eye syndrome, the initial stage of Coats disease is indicated by mild strabismus and frequent redness of the sclera.
As retinitis progresses, pockets of cholesterol grow in the eye, and the retinal vessels bleed and dilate more and more. As a result, the capillaries merge into nodules. The patient begins to see unusual patterns. In the final stages of the disease, partial blindness occurs, and then complete death of the affected organ.
Diagnostics
ICD-10 classifies Coats' retinitis among other retinal diseases. The disease code is H.35.0.
At the initial stage, ophthalmoscopy, an examination by an ophthalmologist, allows identifying pathology. The doctor examines the patient's fundus using special equipment - an ophthalmoscope and a device with a fundus lens.
The examination reveals abnormalities in the structure of the following elements of the eye:
- retina;
- optic nerve head;
- fundus vessels.
With the help of ophthalmoscopy, it is determined how far the initial stage of retinitis has progressed. If the disease began recently, then many hard exudative islands are found on the periphery of the retina. When the disease is close to entering the advanced stage, cholesterol lesions fill the central part of the retina. In both cases, the fundus capillaries are distorted and dilated.
A routine examination is not the only way to detect Coats disease. The following methods are also used for this:
- Perimetry is the study of the visual field and its boundaries using an apparatus called perimeter. Allows you to identify the impairment of peripheral vision from which the disease begins.
- Visometry is the simplest way to assess visual acuity. In this case, the patient is seated at a distance of 5-6 meters from the poster with optotypes - special symbols. Based on how many of them a person distinguished before and distinguishes now, conclusions are drawn about the dynamics of vigilance.
- Retinal fluorescein angiography , also known as FA. During the test, the patient is injected intravenously with a contrast agent—fluorescein sodium salt. The contrast allows you to capture a picture of the fundus of the eye, down to the smallest vessels, using a special camera. By assessing the images, the diagnostician clarifies the diagnosis and determines the amount of treatment required.
- OCT, or optical coherence tomography , is a computer scan in which the patient is asked to stare at a flashing dot. The method allows us to identify pathologies in the very center of the retina - the macula, where light rays that enter the eye are normally focused. OCT helps to assess the volume of exudative deposits.
- Ultrasound of the eyeball is an ultrasound diagnostic that uses high-frequency waves. They convey to the screen an accurate picture of what the eye looks like from the inside. This helps determine how the pathological changes are located and how widespread.
- Head CT is a computed tomography scan in which the entire person is placed in a special scanner called a tomograph. As a result of the scan, the diagnostician receives detailed layer-by-layer images of organs and tissues located in the patient’s head.
- Pathological examination , combining biopsy and histology, helps determine the composition and structure of the affected tissue. In this method, samples are removed from the affected organ and then examined under a microscope.
If the patient has already had a complete retinal detachment, it is necessary to perform not only a CT scan, but also color Doppler ultrasound with magnetic resonance imaging. This will help eliminate the possibility of malignant tumors.
Treatment
How to treat exudative retinitis? Therapy is effective only in the initial stages of the disease.
It sets the following goals:
Carry out successful obliteration, that is, soldering, of deformed capillaries of the eye.- Stop the destruction of intraocular blood vessels.
- Prevent the occurrence of new exudative lesions.
- Prevent retinal detachment and the development of secondary complications.
In the treatment of patients with Coats retinitis, medications, cryopexy and laser coagulation of the retina, as well as extrascleral filling are used. If the disease has reached the terminal stage, it can no longer be treated. Then they resort to enucleation - the complete removal of the eye destroyed by the disease.
Drug therapy
With the help of medications, the patient is prepared for surgery. In this case, drugs of the following groups are used:
- Angioprotectors are agents that improve microcirculation of the eye, stabilize metabolism inside the capillary walls, and also reduce their permeability. In addition, such drugs thin the blood.
- Antiplatelet agents are medications that prevent platelets and red blood cells from sticking together and clogging blood vessels. Such drugs improve blood flow and prevent the formation of blood clots.
Emoxipin belongs to the category of angioprotectors. Among other things, it protects the retina from bright light and accelerates the resorption of fluid that enters the eye through abnormal vessels.
This drug has the following pharmacological analogues:
- Trental;
- Troxerutin;
- Divaskan;
- Calcium dobesilate.
While awaiting surgery, patients take antiplatelet drugs such as Aspirin, Ticlopidine and Clopidogrel.
Laser coagulation of the retina
Until the middle of the developed stage, if no more than two-thirds of the fundus of the eye is affected, doctors resort to laser coagulation of the retina. At the same time, abnormal vessels are sealed, and thereby stop hemorrhages. The course of treatment consists of 2-6 series of procedures at intervals of 3-4 months.
IMPORTANT! Vision stabilizes in 70% of patients with Coats disease who undergo laser surgery.
Retinal cryopexy
If the retina has already begun to peel off, then cryopexy is used until the middle of the third stage of the disease. In this method, doctors freeze damaged areas of the fundus of the eye using a thin external probe. The area of the retina, which is located directly under the device, is soldered to the inner shell of the eye. This is how all the gaps are blocked one by one. Cryopexy allows you to restore the tightness and integrity of the retina, stop or slow down its detachment.
Extrascleral filling
Extrascleral filling is used from the second half of the advanced stage of Coats disease to the middle of the advanced stage.
This complex operation is carried out as follows:
- The outer layer of the eye is cut, the sclera is pressed tightly against the retina.
- Sponge silicone fillings are placed on defective areas of the sclera. They are made in advance, according to individual patterns.
- If necessary, excess fluid is removed from the eye.
- Sutures are placed along the conjunctival incision.
In 95% of cases, surgery helps stop the development of pathology.
Notes
- Disease ontology database (English) - 2021.
- Monarch Disease Ontology release 2018-06-29sonu - 2018-06-29 - 2018.
- Shields CL, Uysal Y., Benevides R., Eagle RC, Malloy B., Shields JA
Retinoblastoma in an eye with features of Coats' disease // J Pediatr Ophthalmol Strabismus (English) Russian. : journal. - 2006. - Vol. 43, no. 5. - P. 313-315. - PMID 17022167. - ↑ 123456
EdwardDP, Mafee MF, Garcia-Valenzuela E, Weiss RA. Coats' disease and persistent hyperplastic primary vitreous: role of MR imaging and CT. Radiol Clin North Am 1998; 36(6): 1119–1131. - WoodsAC, Duke JR. Coats's disease. I. Review of the literature, diagnostic criteria, clinical findings, and plasma lipid studies. Br J Ophthalmol 1963; 47: 385–412.
- ChangMM, McLean IW, Merritt JC. Coats' disease: a study of 62 histologically confirmed cases. J Pediatr Ophthalmol Strabismus 1984; 21(5): 163–168.
- Shields JA, Shields CL. Review: Coats disease—the 2001 LuEsther T. Mertz lecture. Retina 2002; 22(1): 80-91.
- BerrocalT, de Orbe A, Prieto C, et al. US and color Doppler imaging of ocular and orbital disease in the pediatric age group. RadioGraphics 1996; 16(2): 251–272.
- GlasierCM, Brodsky MC, Leithiser RE Jr, Williamson SL, Seibert JJ. High resolution ultrasound with Doppler: a diagnostic adjunct in orbital and ocular lesions in children. Pediatr Radiol 1992; 22(3): 174–178.
- EisenbergL, Castillo M, Kwock L, Mukherji SK, Wallace DK. Proton MR spectroscopy in Coats disease. AJNR Am J Neuroradiol 1997; 18(4): 727–729.
- Chung EM, Specht CS, Schroeder JW. Pediatric Orbital Tumors and Turmorlike Lesions: Neuroepthelial Lesions of the Ocular Globe and Optic Nerve. Radiographics. 2007 Jul-Aug;27(4):1159-86.
- Kremer I, Nissenkorn I, Ben-Sira I. Cytologic and biochemical examination of the subretinal fluid in diagnosis of Coats' disease. Acta Ophthalmol (Copenh) 1989; 67(3): 342–346.
- FernandesBF, Odashiro AN, Maloney S, Zajdenweber ME, Lopes AG, Burnier MN Jr. Clinical-histopathological correlation in a case of Coats' disease. Diagno Pathol 2006; 1:24.
- synd/2146
on Who Named It? - G. Coats. Forms of retinal disease with massive exudation. Royal London Ophthalmic Hospital Reports 1908, 17, 3: 440-525.
Prognosis and possible complications
With early diagnosis and proper treatment, the disease has a conditionally favorable prognosis: vision can be preserved, although the disease returns in 40% of patients with remission.
An unfavorable prognosis is given in the following cases:
- advanced stages of the disease;
- negative reaction of the body to surgery;
- relapse of Coats disease.
The disease is especially dangerous for young children. Without timely treatment, 96% of patients develop complicated cataracts, 70% develop neovascular glaucoma, and 23% develop eye atrophy.
Prevention
It is known that about 40% of those who have had retinitis have relapses, so methods of preventing the disease must be taken into account. Retinitis of any type causes deterioration in visual acuity. After a person recovers, he cannot fully regain his vision because it is quite difficult due to the severity of the disease.
Prevention of retinitis involves timely treatment, which is necessary in order to maintain good vision. Prevention also includes protecting the retina. If it is not subjected to mechanical trauma, the risk of developing retinitis again will be minimal.
For prevention, it is possible to use eye drops that will help the eyes recover after the disease. You can ask your doctor for this medicine.
It must be remembered that retinitis is a rather dangerous disease that can deprive a person of his vision.