general description
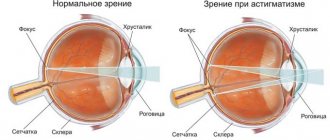
Sympathetic ophthalmia (SO) is a lesion of the choroid (uveal tract) of the healthy eye following penetrating damage to the other eye.
As a consequence of eye injuries, OM develops relatively infrequently, in approximately every fiftieth case, but in most cases it results in loss of vision. The cause of damage to a healthy eye in OM is the close neuro-reflex connections between these paired organs. This state of affairs implies that if one eye is susceptible to any disease, then in due time pathological changes will affect the other, until then healthy eye. OM is considered as a manifestation of autoallergy, which is confirmed by the presence in the blood of patients of circulating antibodies to the elements of the choroid. Certain importance is attached to disorders of nervous trophism.
Risk factors for OM are:
- penetrating injuries of the cornea, sclera, ciliary body, complicated by uveitis;
- intraocular surgical interventions;
- perforation of a purulent corneal ulcer;
- eye injuries complicated by endophthalmitis.
OM usually begins no earlier than two weeks after the injury and is characterized by a steadily progressive course, with periods of exacerbations followed by remission. Sometimes the disease can last for years. Blindness occurs in approximately sixty patients out of a hundred. Prevention of OM involves enucleation of the injured eyeball.
Causes
The reasons for the development of this pathological condition include traumatic iridocyclitis on the opposite side, which arose against the background of mechanical damage or surgical intervention. Sympathetic ophthalmia can also occur after severe contusions or destruction of tumor tissue, but this happens much less frequently.
At the heart of this problem are immune mechanisms: damage to the eye leads to disruption of the hemo-ophthalmic barrier of the body and the production of antibodies that affect the other eye. Thus, the inflammatory process leads to gross disturbances in the functioning of the optic tract. This occurs more often in people with low resistance to negative environmental factors.
Symptoms of sympathetic ophthalmia
Symptoms of OM are often indistinguishable from the symptoms of other ophthalmological diseases, but the main difference is that a healthy eye becomes ill against the background of another, already diseased eye. It should be remembered that in every third case CO occurs in an erased form. Symptoms of disease activity:
- blepharospasm (involuntary squinting of the eyes, difficult to overcome by volitional effort);
- constriction of the pupil;
- severe lacrimation;
- decreased visual acuity;
- photophobia;
- the appearance of spots on the cornea of the eye;
- scleral injection.
It is unusual to have all the symptoms at once; usually there are no more than two. The erased form is not clinically manifested and is detected only by biomicroscopy.
Symptoms
There are 3 types of sympathetic ophthalmia:
- Serous (serous iridocyclitis develops). It occurs easily and in the vast majority of cases does not affect visual acuity.
- Mixed (may be accompanied by optic neuritis against the background of severe plastic iridocyclitis or symblepharon). This type of inflammatory process is more common than others. Often ends in complete loss of visual ability.
- Neuritic (the blind spot increases, sensitivity to colors sharply weakens, photophobia develops). The pathology is rare and, as a rule, is diagnosed as an independent disease. At the onset of neurotic sympathetic ophthalmia, there are no characteristic symptoms.
Photophobia is characteristic of the neuritic form of the disease
Common symptoms for them are:
- uncontrolled lacrimation;
- inadequate reaction to light;
- narrowing or change in the shape of the pupil;
- the appearance of flashes, “floaters” or bright spots before the eyes;
- blurred vision;
- pain on palpation;
- hyperemia.
During inflammation, the outflow of exudate is disrupted, which can provoke increased pressure inside the eye (glaucoma) or the vitreous body (secondary hypertension).
Find out how dangerous pinguecula is and whether it can be treated here.
In the mixed form, iridocyclitis is often observed
A remedy that will help defeat the infection and relieve swelling from the organs of vision and hearing - instructions for Sofradex eye drops are presented at the link.
Treatment of sympathetic ophthalmia
You should know that in cases of eye injuries and ophthalmic operations, you should always keep in mind the possibility of developing OM. Therefore, if any of the listed symptoms appear, you should immediately consult a doctor. Whether the intact eye can be saved depends on the timeliness of treatment.
The main type of treatment is medication. Corticosteroid hormones are used as a powerful anti-inflammatory agent: they are prescribed subconjunctivally and parabulbarly, parenterally, orally, electropharetically. In persistent cases, cytostatics and antibacterial drugs are prescribed. A radical way to prevent OM is enucleation of the injured eye in case of blindness within up to two weeks after the injury.
Treatment
The appearance of symptoms of the disease requires immediate contact with an ophthalmologist. Any delay in diagnosis and treatment of sympathetic ophthalmia risks irreversible vision loss. To confirm the diagnosis, the doctor performs testing:
- Collection of complaints and medical history. Mandatory emphasis on the presence of injuries and operations (regardless of the statute of limitations).
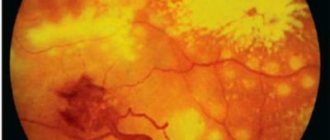
- Ophthalmoscopy (examination of the fundus of the eye).
- Checking visual acuity using the tables of Sivtsev and Golovin.
- Tonometry (for the presence of glaucoma).
- Fluorescein angiography (study of the capillaries that supply the eye).
- Ultrasound of the eyes.
- CT scan of the organs of vision.
After confirming the diagnosis of sympathetic ophthalmia, drug treatment is started, including:
- Corticosteroids (Methylprednisolone, Prednisolone, Metypred). Depending on the form and severity of the disease, they are prescribed orally (with a gradual reduction in dosage), “mini-pulse” therapy, “pulse” therapy (in high doses).
- Immunosuppressants (Cyclosporine).
- Antibacterial therapy with broad-spectrum antibiotics.
The drugs are prescribed subconjunctivally, parabulbarly or orally. Treatment lasts for a long time (about 3 months). If hormonal therapy is ineffective, cytostatics can be used.
With the development of secondary cataracts, surgical intervention is indicated (phacoemulsification of cataracts with implantation of an artificial lens). If the iris is damaged during the development of pathology, laser membranetomy is performed.
If, after the completed course of treatment, symptomatic ophthalmia continues to progress, then the question of removing the injured eye is raised.
Indications, contraindications and advantages of laser vision correction techniques. You can read about this on our website in the article at the link.
Types and classifications
Sympathetic ophthalmia has the following forms of development:
- Serous. Characterized by the occurrence of serous iridocyclitis. Most often, therapy in this case gives a good prognosis and the progression of the disease stops. Occurs with average frequency.
- Neuritic. It is diagnosed quite rarely and is an independent pathology. The onset of progression is often imperceptible and asymptomatic; after some time, mild neuritis appears. Dullness and swelling of the tissues and redness occur. It is usually cured with complete restoration of visual functions only in half of the cases.
- Mixed. It occurs more frequently than those listed and combines the characteristics of both forms. In most cases of therapy, the prognosis is favorable and most often ends in complete recovery of the patient.
Serous form of sympathetic ophthalmia
Recommendations
- A cautionary tale from the past, to K. Barry Sharpless, in MIT Tech Talk; published March 19, 1992; received May 10, 2016
- ^ a b
Gürdal, C;
Erdener, U; Irkeç, M; Orhan, M. (September 2002). "Incidence of sympathetic ophthalmia after penetrating ocular injury and choice of treatment." Ocular immunology and inflammation
.
10
(3): 223–7. Doi:10.1076/ocii.10.3.223.15600. PMID 12789598. - ^ a b
Migliori, Maine (October 2002).
"Enucleation versus evisceration." Current Opinion in Ophthalmology
.
13
(5): 298–302. Doi:10.1097/00055735-200210000-00002. PMID 12218460. - ^ a b
Albert, DM;
Diaz-Rohena, R. (July–August 1989). "A Historical Review of Sympathetic Ophthalmia and Its Epidemiology". Review of Ophthalmology
.
34
(1): 1–14. Doi:10.1016/0039-6257(89)90125-2. PMID 2678549. - ^ a b
Caden, R. (January 1977).
"[Historical Notes of Louis Braille and the Development of the Point (author's translation)]". Klinische Monatsblätter für Augenheilkunde
.
170
(1):154–8. PMID 321864. - Ravin, James G. (2002). "James Thurber and the Problems of Sympathetic Ophthalmia". Archives of Ophthalmology
.
120
(5): 628. doi:10.1001/archopht.120.5.628. PMID 12003613. - Chu, D.S.; Foster, C. S. (Summer 2002). "Sympathetic ophthalmia." International ophthalmological clinics
.
42
(3): 179–85. Doi:10.1097/00004397-200207000-00019. PMID 12131594. - Damico, F.M.; Kiss, S; Young, L.H. (July–September 2005). "Sympathetic ophthalmia." Seminars on ophthalmology
.
20
(3): 191–7. Doi:10.1080/08820530500232100. PMID 16282154. - Friedlaender, M.H.; O'Connor G.R. (2001). Medical Immunology
(10th ed.). Lange Medical Books/McGraw-Hill. ISBN 978-0-8385-6300-7. - Zechariah, Massachusetts; Lamarche, J; Laurin, M. (August 1984). "Sympathetic uveitis 66 years after injury." Canadian Journal of Ophthalmology
.
19
(5): 240–3. PMID 6478310.
Story
Although descriptions of sympathetic ophthalmia can be found in ancient Greek texts, modern understanding of SO comes from the works of Scotland. William Mackenzie who characterized and named the disease sympathetic ophthalmitis. In Mackenzie's time, oral Mercury and leeches applied to the conjunctiva were the treatment of choice for SO.[4]
It is believed that Louis Braille, who damaged one eye as a child, lost sight in the other eye due to S.O.[5] James Thurber Adult blindness was also diagnosed as sympathetic ophthalmia caused by the loss of an eye when he was six years old.[ 6]
Prevention
Since the cause of ophthalmia is injury to one of the eyes, all methods of prevention depend on its condition. To begin with, it should be noted that any intervention in the structure of the organ of vision, including surgery, must occur under the supervision of a specialist. If you have injured your eye, suffered a blunt injury, or noticed unusual discharge or deposits in any part of it, you should immediately consult a doctor.
Although prevention of OS comes down to removing the damaged eye, it is worth carefully considering other options for restoring vision.
If the injured organ still retains some of its basic functions, a good doctor will certainly fight for its health, while monitoring the other eye, excluding or confirming the development of ophthalmia. If vision is completely lost, the specialist must take all necessary measures to protect the other eye as soon as possible. You must understand that the attending physician must be completely trustworthy in his actions, and if this is not the case, then it is better to consult another specialist.
Note that after removal of an eye, there is a conditional period during which any of the symptoms may appear in the other eye. The period usually lasts up to two months, and you need to be very attentive to any details and subtle changes in visual function. The manifestation of symptoms is a reason to seek qualified help again, and the patient must be under the watchful supervision of a specialist throughout the entire period of rehabilitation. After two months, there were no documented cases of secondary recurrence of symptoms.
General prevention of eye diseases is the first priority. You need to understand that any little things like prolonged visual stress, poor-quality removal of eyelashes from the shell, and even advanced forms of eye colds can greatly affect the health of the eye and cause serious consequences. Injuries, which in most cases become the cause of sympathetic ophthalmia, must be treated by a specialist and nothing else. Keep yourself in shape, don't get sick and take care of your eyes!
Sympathetic reflex dystrophy
Experts' opinions:
Demidkin Pavel Mikhailovich
Treatment of joints
all expert opinions
Video on the topic:
all videos on the topic
What is sympathetic reflex dystrophy
The syndrome is characterized by combinatorial pain in the distal arms and legs due to disturbances in trophism, movements and functions of the autonomic system. Neuropathic pain syndrome develops as a result of damage to nerves or soft tissues and is characterized by the manifestation of symptoms from several systems at once.
Kinds
Sympathetic reflex dystrophy syndrome extends to the entire limb or to a specific area. More often the entire arm or leg is affected, less often the patella, wrist, thigh, etc. In almost half of patients, the pain syndrome covers the side of the body opposite to the source of the lesion.
The disease is divided into three stages:
- the first stage lasts up to six months. The limb swells, hurts, feels hot when you touch it,
- during the second stage, the skin of the limb shines and becomes cold,
- at the third stage, contractures form.
Causes
The syndrome develops gradually after the following conditions:
- various types of injuries (fractures or sprains of muscles and ligaments, burns of the limb, after which chronic pain develops),
- diseases of the central nervous system. This group includes sclerosis, stroke, traumatic brain injury,
- diseases of internal organs. For example, myocardial infarction.
The etiology of reflex sympathetic dystrophy remains uncertain in some cases.
The mechanism of development is associated with chronic persistent pain. The sensitivity of peripheral nerves connecting to sympathetic transmitters increases. Mediators are substances that transmit nerve impulses. The activity of the sympathetic nervous system, which is responsible for trophism, regulation of vascular tone, and sweating, increases. As a result, sympathetic tone increases and vasospasm develops.
Symptoms and signs
The clinical picture of sympathetic reflex dystrophy manifests itself from several sides at once within a few weeks after the provoking factor.
The patient complains of a sharp and burning pain, which spreads not only near the injured area, but also innervates the affected nerve roots. Because of this, a false sensation of paresis is created. The mobility of the limb appears to be limited.
Disturbances of sensations are noted. The threshold of sensitivity decreases, therefore the susceptibility of the senses increases. Dysesthesia, a condition in which pain intensifies when lightly touching the skin of the upper and lower extremities, also worsens.
Excruciating pain worsens at any moment - with anxiety, excitement, bright light and cold, so the patient covers and protects the injured area. He tries to protect himself from irritants such as cold/heat, sound and light, and tactile touches. Against this background, mental disorders develop - the patient withdraws into himself, becomes irritable and aggressive.
Symptoms of movement disorders:
- osteoporosis develops. Bones become brittle.
Signs of trophic disorders:
- muscles atrophy
- contracture of the flexor fingers develops on the upper or lower extremities,
- skin color changes - local pallor, bluishness or redness is observed,
- the condition of the skin changes. The cover becomes thinner and glossier.
Symptoms of autonomic system disorders:
- swelling of the skin,
- sweating increases.
Which doctor treats sympathetic reflex dystrophy?
The disease is diagnosed and treated by a neurologist. If necessary, other specialists are involved in the treatment process to eliminate the cause of the pathology.
Diagnostics
MRI images of the distal extremities show changes in the musculoskeletal system, for example, patchy wasting, signs of osteoporosis. Blood test results show a slight increase in white blood cells.
Treatment methods
To stop the pathological process of the affected limb, first stop the acute signs of the disease, and then begin to restore motor activity.
Your doctor will prescribe medications to relieve pain, such as nonsteroidal anti-inflammatory drugs and analgesics. If they do not have a positive effect, take corticosteroids for a short period of time. For acute pain, the sympathetic nerves are blocked by injecting an anesthetic into the nerve that supplies the limb. To relieve symptoms of trophic and vegetative changes, calcium antagonists and alpha-blockers are prescribed. Neuroleptics and antiepileptic drugs combat neurological symptoms. Often, to relieve swelling, venotonics are prescribed to normalize the outflow of blood through the veins.
During treatment, cold and warm bandages are applied alternately to the limbs, while gymnastics are performed and the arms and legs are worked out.
results
The first two stages of sympathetic reflex dystrophy syndrome are completely reversible. The third stage cannot be treated completely; it can only be stopped temporarily.
Rehabilitation and lifestyle restoration
During the period of remission, they resort to physiotherapy. Magnetotherapy, neurostimulation of the spinal cord, as well as acupuncture affect nervous tissue, stimulate its renewal and normalize motor activity. Physiotherapy sessions are long.
Lifestyle with sympathetic reflex dystrophy
The range of movement is limited, so patients ask for help in performing basic tasks - fastening the lock around the neck, putting on shoes, etc.
Return to list
SYMPATHETIC OPHTHALMIA (sympathetic inflammation) is a disease of the second eye that occurs as a result of chronic traumatic iridocyclitis of the first eye.
Etiology: penetrating injury to the other eye, complicated by sluggish iridocyclitis, less commonly, surgical intervention on the eyeball or perforated corneal ulcer.
Pathogenesis:
The main role in inflammation of the second eye is attributed to autoimmune reactions and the action of tissue antigens of the damaged eye.
Symptoms occur at different times - from 12-14 days to several months and even years after injury to the first eye. The erased form of the disease has the character of serous iridocyclitis and is detected only by biomicroscopy in the form of edema of the corneal endothelium and isolated precipitates on its posterior surface.
With severe serous or serous-fibrinous iridocyclitis, lacrimation, photophobia, blepharospasm, mixed injection of the eyeball, whitish or pigmented precipitates on the posterior surface of the cornea, swelling and hyperemia of the iris, single pigment deposits on the anterior capsule of the lens, synechia, and vitreous opacities appear. The process is often combined with neuroretinitis (hyperemia of the optic disc, blurred boundaries, dilated veins), sometimes with focal chorioretinitis. Changes in the refractive media and the retina cause decreased vision.
Treatment
.
Locally - mydriatic agents in the form of drops, ointments, powder. Corticosteroids—installations of 1% hydrocortisone emulsion 4-5 times a day, placing 0.5% hydrocortisone ointment behind the eyelids 3-4 times a day, subconjunctival injections of 0.2-0.3 ml of 0.5-1% cortisone emulsion (hydrocortisone) or 0.4% dexamethasone solution. In the stage of subsiding of the process, resorption therapy—electrophoresis with papain, fibrinolysin and aloe. Leeches on the temple. Antibiotics and sulfonamides; penicillin 150,000-200,000 units 2-4 times a day, per course 6,000,000-7,000,000 units, streptomycin 250,000-500,000 units 1-2 times
a day, per course 5,000,000-8,000,000 IU, tetracycline with nystatin 100,000 IU 4 times a day for 5-10 days, chloramphenicol 0.5 g 3-4 times a day for 5-7 days, erythromycin 0.5 g 4 times for 5 —7 days, sulfapyridazine 0.5 g (on the first day 2-4 tablets, on subsequent days 1-2 tablets) and other drugs. Orally - prednisolone or dexamethasone according to the scheme. While taking prednisolone, a salt-free diet with an increase in the amount of protein is recommended, and a solution of potassium acetate is administered orally. Butadiene 0.15 g 4 times a day for 2-3 weeks, diphenhydramine 0.03 g and calcium gluconate 0.5 g 3 times a day (1 month) are also indicated.
Forecast
serious and depends on timely treatment. It is more favorable for neuroretinitis and serous uveitis.
Prevention
: timely and correct treatment of penetrating wounds of the eye, its enucleation in the first 14 days after injury in case of extensive damage, as well as iridocyclitis, hypotension, pain on palpation and decreased vision to light perception.
Pathophysiology
Sympathetic ophthalmia is now considered an autoimmune inflammatory reaction to ocular antigens, in particular delayed hypersensitivity to melanin-containing structures from the outer segments of the photoreceptor layer of the retina. The immune system, which is not normally exposed to the whites of the eye, is introduced into the contents of the eye after injury.[1] After exposure, it perceives these antigens as foreign and begins to attack them. This process may begin days or years after the inciting traumatic event.