Does your skin often become red and inflamed? Does it react sharply to temperature changes? Are there visible vessels on it? Has your skin become sensitive to cosmetics? Do you feel dry and notice flaking? Perhaps it is rosacea, or rosacea.
People with fair hair and skin are more likely to develop rosacea.
It will not be possible to get rid of it forever, because rosacea is a chronic disease (there are periods of remission and exacerbations). At the same time, following the doctor’s recommendations and adhering to preventive measures, you can significantly alleviate its manifestations and avoid complications. Cosmetologist and medical dermatovenerologist Yulia Baranova told a journalist of the information portal “Healthy People” in detail about the symptoms, diagnosis and treatment of rosacea. The specialist also shared practical advice on how to prevent complications and relapses of this disease.
Causes of eye rosacea
The reasons for the development of ocular rosacea can be identified as follows:
- Alcohol abuse and smoking. These bad habits contribute to damage to the capillaries, disrupt their normal tone, and lead to stagnation. All these become favorable factors for the manifestation of the disease.
- Frequent visits to the solarium, spending long periods of time in the sun without using eye protection. Ultraviolet radiation triggers a number of pathological reactions that damage skin vessels and intercellular substance, provoking the development of eye rosacea.
- Sudden temperature changes.
- A connection has been established between the development of ocular rosacea and diseases of the digestive system.
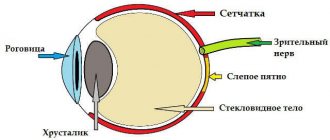
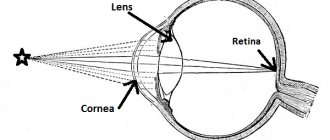
An indispensable condition for the occurrence of a pathological process in the organs of vision is the presence of rosacea on the skin of the face. The inflammatory process leads to translucent blood vessels through the epidermis and severe erythema. Venous outflow suffers, blood stagnation is constantly present, which is the basis for the development of eye rosacea.
Disturbances in the functioning of the meibomian glands cause instability of the tear film, excessive evaporation of tear fluid, and the formation of dry eye syndrome. All of these become key mechanisms in the development of the ocular form of rosacea.
Scientists tried to establish a connection between the disease and eyelash mite infection, however, they could not trace it. However, Demodex follicularum is quite common in patients with ocular rosacea.
Introduction
Rosacea is a chronic inflammatory skin disease with a complex pathogenesis.
The central part of the face is mainly affected.1,2 The disease has no gender preference. It occurs at any age; however, the typical onset is after age 303. The course of the disease usually manifests itself in remissions and exacerbations. In people with fair skin, the prevalence of the disease reaches 10%. However, the disease is not limited to fair skin; it can also be seen on dark and dark skin tones. Clinical manifestations of the disease include facial erythema (transient or persistent), telangiectasia, edema, papules and pustules. The patient may have one of these or a combination of them. Patients may have no symptoms or complain of burning, tingling, pain or itching.
Initially, the disease was divided into 4 main subtypes. These were:
- erythematotelangiectatic (subtype 1),
- papulopustular (subtype 2),
- phymatous (subtype 3)
- ophthalmic (subtype 4).
Granulomatous rosacea was considered a variant of rosacea rather than a subtype. However, not only can a subtype transform into another, but these subtypes can also arise simultaneously. Thus, in 2017, there has been a shift from subtypes to phenotypes in the diagnosis of rosacea, and diagnosing a patient with rosacea requires at least one diagnostic phenotype or two major phenotypes.
These phenotypes are summarized in Table 1.
| Diagnostic phenotypes | Large phenotypes | Small phenotypes |
| Persistent facial erythema | Transient facial erythema | Burning |
| Phymatous changes | Inflammatory papules and pustules | Tingling |
| Telangiectasia | Edema | |
| Eye changes | Dryness |
Diagnostic phenotypes
- Persistent erythema of the central part of the face, which is aggravated by provoking factors
- Phymatous changes (most often rhinophyma)
Large phenotypes
- Transient central facial erythema/redness
- Inflammatory papules and pustules
- Telangiectasia
- Ocular changes: blepharitis, keratitis, conjunctivitis, telangiectasia of the eyelid margins.
Small phenotypes
- Burning
- Tingling
- Edema
- Dryness
Because rosacea is a disease with a complex pathogenesis and multiple manifestations, its treatment poses a challenge for dermatologists. The following sections will review the main problems in the treatment of erythema, hyperemia, telangiectasia, inflammatory lesions and phymatous changes, and discuss possible solutions.
Redness, transient and persistent erythema
Transient or persistent facial erythema is the most common finding in patients with rosacea of all subtypes. It is a very common clinical problem that dermatologists encounter in daily practice.6 Symptoms of rosacea often begin with redness of the skin and lead to persistent erythema.
Facial erythema usually has a diffuse distribution and is located in the central part of the face. Although the inflammatory lesions may resolve over time, the erythema may persist. Increased innate immunity, neurovascular and neuroimmune dysregulation play a central role in the development and maintenance of facial erythema through vasodilation.
Currently available treatments for rosacea target inflammatory changes rather than erythema; these are: topical metronidazole, topical azeleic acid and systemic tetracyclines. Although topical metronidazole and topical azeleic acid should theoretically treat erythema on a molecular basis, current research suggests that they are generally not helpful in treating erythema, especially if it has become persistent.
The therapeutic challenge for dermatologists is that there are a limited number of effective topical agents that can be used in the treatment of diffuse facial erythema in patients with rosacea. Among them, topical steroids are very commonly used.
However, with the use of topical steroids, skin atrophy is inevitable, and exacerbations are observed after discontinuation of therapy. For these reasons, the use of topical corticosteroids should be avoided in patients with rosacea. Topical calcineurin inhibitors may help reduce facial erythema in some cases, but in most cases they actually worsen rosacea.
Lasers are increasingly used in the treatment of vascular lesions. The 595 nm pulsed dye laser (PDL) is a common treatment option for diffuse facial erythema. Treatment with PDL at purpuragenic doses usually produces sufficient cosmetic improvement in 2 treatment sessions.
In addition, it reduces burning, tingling, sensitivity, itching and dryness; This dramatically improves the patient’s quality of life. However, due to patient discomfort and facial bruising resulting from the procedure, PDL should not be used at purpuragenic doses. PDL is effective in reducing facial erythema and at subpurpurogenic doses, but more treatments have recently been required.
Recently, intense pulsed light (IPL), which is a flashlight emitting incoherent light with a wavelength of 400–1400 nm, was compared with PDL (at nonpurpuragenic doses) in the treatment of diffuse facial erythema. Not only was IPL found to be as effective at 560 nm filtration as PDL in treating facial erythema, but patients treated with IPL showed significant improvement than patients treated with PDL at 90 days of follow-up.
In addition, it did not cause any serious side effects.13 Thus, in patients with persistent diffuse facial erythema; Both PDL and IPL can be used for cosmetic enhancement.
Brimonidine tartrate 0.5% gel is a topical treatment approved for the treatment of transient and persistent facial erythema in patients with rosacea over 18 years of age. It is a potent vasoconstrictor that selectively binds to alpha-2 adrenergic receptors on the smooth vessels of muscle cells in the peripheral cutaneous vasculature.
Patients treated with topical brimonidine clinically experience a 60–70% reduction in erythema with minimal side effects. Moreover, its effect begins within 30 minutes.
However, the disadvantage of its use is that the effects of brimonidine gel are temporary; erythema reappears within 9–12 hours. Therefore, one dose per day may not be sufficient and twice daily use may be required. However, it is important to note that worsening of erythema may occur due to the use of brimonidine. This side effect can be overcome by using barrier creams correctly and avoiding excessive use of brimonidine.
Another new topical agent that has recently been approved for the treatment of facial erythema is oxymetazoline hydrochloride 1% cream.15 It is an alpha-1a adrenergic agonist that is used to treat moderate to severe persistent facial erythema in patients with rosacea. At higher concentrations, it also binds to alpha-2 adrenergic receptors.
Bauman et al followed patients with facial erythema using oxymetazoline cream for 29 days and concluded that topical oxymetazoline is a safe and effective treatment for moderate to severe facial erythema when applied once daily.
Tangetti et al demonstrated that oxymetazoline is effective in reducing facial erythema starting within the first hour of its initial application.19 Thus, oxymetazoline cream is an effective and easy-to-use topical alternative in the treatment of persistent facial erythema with its once-daily regimen. applications.
In addition to topical antihypertensive drugs, systemic antihypertensive drugs are used in the treatment of off-label facial erythema. Beta blockers may be used in the treatment of refractory facial erythema. Nadolol and propranolol, which are non-selective beta-adrenergic antagonists, are effective in reducing hot flashes.
However, their use was abandoned due to possible side effects: hypotension and bradycardia. Carvedilol, a non-selective beta-adrenergic agent and alpha-1 antagonist, is a better alternative in the treatment of refractory facial erythema. When used at a dose of 3.125–6.25 mg 2–3 times daily, carvedilol results in clinical improvement within 3 weeks without the side effects of nadolol and propranolol. Carvedilol differs from other non-selective beta-blockers in that its metabolites are powerful antioxidants.
This feature further increases its therapeutic effectiveness for facial erythema. On the other hand, the use of calcium channel blockers in the treatment of facial erythema is not recommended because they may aggravate rosacea.6 Clonidine is a centrally acting antihypertensive agent that acts through alpha-2 adrenergic receptor agonist activity.
Wilkin investigated the use of systemic clonidine hydrochloride for the treatment of hyperemia. Patients were given 0.05 mg clonidine hydrochloride twice daily for two weeks. Although clonidine did not cause a significant change in blood pressure, it also did not reduce flushing caused by red wine, chocolate, and hot weather. Cunliffe et al also examined the effect of clonidine on hot flushes. Similarly, patients were administered 0.05 mg of clonidine hydrochloride twice daily. Similar to Wilkin's findings, clonidine was found not to suppress hot flashes.
Intradermal injection of botulinum toxin type A (Botox) is a promising treatment for facial flushing and erythema. The release of acetylcholine leads to vasodilation of cutaneous vessels, which manifests itself in the form of facial flushing and erythema.
Botox inhibits the release of acetylcholine and provides symptomatic relief in patients with facial flushing and erythema. 23 Park et al reported two patients whose erythema was successfully treated with Botox injections. The first patient received a total dose of 50 units, and the second patient received a total dose of 65 units. Each patient received the full dose over two treatment sessions, and noticeable cosmetic results were achieved one week after the second treatment session in both cases.
Symptomatic relief persisted for 4 months in both cases, and patients returned to the clinic for a second course of treatment24. Bloom et al. conducted a study in 15 patients with facial erythema, each of whom received 15–45 units of intradermal Botox injection.
They concluded that intradermal injection of Botox is an effective and safe treatment for facial erythema in rosacea.25 Intradermal injection of Botox has been shown to help relieve facial erythema in several patients with rosacea; Further research with a larger sample size is needed to illustrate this treatment in detail.
Telangiectasia
Telangiectasias cause cosmetic discomfort to patients, and they often seek treatment. However, topical or systemic agents are ineffective in the treatment of telangiectasia. Currently, physical methods, that is, laser and light-based devices, are used to treat vascular manifestations of rosacea. To obtain cosmetically acceptable results, an average of one to four sessions is required.
The basis of these treatments is that hemoglobin absorbs the energy emitted by these devices, resulting in the disappearance of vascular lesions24. Neodymium doped yttrium aluminum garnet (Nd-YAG), 532 nm Potassium Titanyl Phosphate (KTP), 595 nm PDL, IPL and dual wavelength long pulse 775 nm alexandrite/1064 nm neodymium: yttrium aluminum (LPAN) are examples of these methods. 26, 27
The most common examples of these are PDL, Nd:YAG and IPL. A review article by Anzegruber et al. It was concluded that IPL is recommended at level A, and Nd:YAG laser (including KTP) and PDL are recommended at level B. Due to the larger spot size, IPL causes fewer side effects compared to PDL; therefore, its use is more advantageous compared to PDL. Additionally, PDL is more effective than Nd:YAG in treating vascular manifestations, but Nd:YAG is associated with less pain.
The effectiveness of Nd:YAG lasers in treating erythema, telangiectasia and skin texture in patients with rosacea can be increased by combining it with topical retinoic acid preparations. Independent evaluators found that topical retinoic acid increased the effectiveness of Nd:YAG laser treatment by 47%.
Radiofrequency (RF) devices cause focal damage to the dermis by producing heat and electrical current through electromagnetic radiation. This damage stimulates the formation of new collagen through a rapid healing process. Compared to laser treatment, RF is a newer treatment option for rosacea. A study by Kim et al compared the effectiveness of RF and PDL treatment for rosacea. Both methods were used for 3 sessions at a monthly interval.
RF and PDL produced similar results in the treatment of erythematotelangiectatic rosacea; there was no statistically significant difference. Thus, both RF and PDL are effective in the treatment of erythema and telangiectasia. On the other hand, RF was more effective than PDL in patients suffering from papulopustular telangiectasia. In a study of 21 patients with moderate to severe rosacea, PDL was combined with RF.
It was concluded that combination therapy is more effective than PDL alone in the treatment of erythema, hot flashes, and telangiectasia. Thus, in the treatment of refractory erythematous ectatic rosacea, PDL and RF may be considered for treatment alone or in combination.
Recently introduced combination treatments have been found to be more effective in treating patients with refractory rosacea than single treatments. The addition of PDL treatment to oral minocycline therapy has been found to reduce relapse rates in patients suffering from erythema and telangiectasia. The relapse rate with minocycline alone was 48%; however, the relapse rate of minocycline plus PDL was 37%.
Additionally, Nd:YAG laser treatment can be added to topical brimonidine therapy. Brimonidine itself is effective in treating erythema, although the effect is temporary. However, telangiectasias persist after treatment with brimonidine. Cosmetically, better treatment results were obtained when patients with erythematotelangiectatic rosacea were first treated with Nd:YAG laser and topical brimonidine therapy was added 1 month later.31
Papulopustular lesions
Inflammatory papules and pustules are the main phenotypes observed in patients with rosacea. For mild lesions, local treatment is sufficient. On the other hand, in moderate and severe cases, systemic and local treatments should be combined. A variety of topical medications are used to treat papulopustular rosacea (PPR): metronidazole, azaleic acid, ivermectin, pimecrolimus, retinoids, permethrin, benzoyl peroxide, erythromycin, and dapsone.
Nd:YAG laser, PDL and RF are also effective in treating papulopustular lesions. 26,29 Systemic treatments for papulopustular lesions are oral antibiotics, oral zinc sulfate, and oral ivermectin.
Metronidazole cream 0.75–1% is effective in treating PPD when used twice daily. 26 In a randomized controlled trial of 51 patients, the clearance rate of topical metronidazole was found to be 90%, which is similar to that of oral tetracyclines.
In a study by Dahl et al. the effectiveness of topical metronidazole 0.75% and 1% was compared and no difference was found between the two concentrations.
When applied topically, azaleic acid suppresses the production of reactive oxygen species and induces the production of proinflammatory cytokines.
Azaleic acid gel 15% applied twice daily for 15 weeks produced significantly better results for papules and pustules compared to metronidazole 0.75% cream. 12 weeks.35 Moreover, azaleic acid foam causes fewer side effects than azaleic acid gel when both are used at 15% concentration.36 Thus, metronidazole (0.75–1%) and azaleic acid (15%) are effective in the treatment of PPR when applied topically.
Ivermectin is an antiparasitic drug that reduces the density of demodex on the skin of patients with rosacea. Demodex mites are commonly found in human flora; however, their density increases in patients with rosacea. Ivermectin has anti-inflammatory effects against these mites.
Ivermectin cream 1% is a safe and tolerable alternative to first-line treatment for the treatment of PPD. It is more effective for the treatment of PPD than metronidazole cream 0.75%. However, its effectiveness has not been compared with topical azaleic acid 15%, which is also more effective than topical metronidazole 0.75%. Dall'Ogllio et al conducted a study that examined the effectiveness of 1% ivermectin cream in the treatment of PPD .
They used erythema-directed photography to evaluate the results. Thirty-two percent of cases achieved complete resolution with 8 weeks of topical ivermectin. In addition, a significant reduction in erythema was observed. Ivermectin is a safe and effective topical treatment alternative for patients with refractive error and is registered in Europe and the USA.
Pimecrolimus cream 1%, which is a calcineurin inhibitor, is also an effective alternative in the treatment of PPD. It is as effective as metronidazole 1% cream. However, it is also a drug that triggers rosacea.
Retinoids are also an alternative for treating inflammatory lesions of rosacea. However, keep in mind that the irritant side effects of retinoids may be more pronounced in rosacea patients with delicate skin. Of the retinoids, only tretinoin 0.025% and adapalene gel were tolerable and used successfully for the treatment of PPD.
Permethrin 5% cream, when applied topically twice daily for 2 months, is as effective as metronidazole in treating PPD. It is even more effective when combined with other anti-inflammatory agents.40 Topical permethrin 5% is effective in treating erythema and papules in patients with rosacea, but is not effective in treating telangiectasias and pustules. However, it is recommended as class A for the treatment of PPD.
Topical erythromycin gel 2% is as effective as metronidazole cream 0.75% in the treatment of PPD. 26 When combined with benzoyl peroxide, topical erythromycin produces better results than topical metronidazole. Thus, this combination is a good alternative for the treatment of rosacea.41 The combination of 5% benzoyl peroxide gel with clarithromycin gel is also recommended for the treatment of rosacea. 26 Dapsone 5% gel, when used for 12 weeks, is also as effective as metronidazole cream 0.75%, so it can be used to treat PPD.
Regarding systemic antibiotics, low-dose oral tetracyclines (eg, doxycycline 40 mg/day) are effective in treating PPD. Azithromycin and clarithromycin are also used in the treatment of PPD. Although one randomized clinical trial found azithromycin 500 mg per day to be as effective as doxycycline 100 mg per day, in general azithromycin and clarithromycin are considered less effective than doxycycline for the treatment of PPD.
Ampicillin can also be tried in refractory cases. However, it is not as effective as oral tetracyclines. 26 Although antibiotic resistance is a serious problem worldwide, daily use of doxycycline 40 mg/day does not result in antibiotic resistance even with long-term use.
Retinoids, topically or systemically, are used to treat rosacea for their anti-inflammatory properties at lower doses (eg, 0.3–0.5 mg/kg/day). Isotretinoin at a dose of 20 mg/day is effective in reducing erythema and inflammatory lesions. Oral isotretinoin not only provides rapid improvement, but also reduces relapse rates. Compared to topical retinoids, such as tretinoin cream 0.025%, systemic retinoids are more effective.
Zinc sulfate when taken orally at a dose of 100 mg/day is also effective in reducing the inflammatory lesions of rosacea. The only side effect reported was stomach upset in 12% of patients. Oral ivermectin (200 mcg/kg/day) is also an alternative treatment for PPD, although it is supported by level D evidence.
In patients with treatment-resistant rosacea, a combination of oral ivermectin and 5% permethrin cream may be considered, as this combination has been effective in reducing Demodex density in immunocompromised patients.
Phymatous changes
Phymatous changes occur due to hypertrophy of the sebaceous glands, proliferation of blood vessels and connective tissues. Most often, phymata occur on the nose, especially in the lower third of the nose, which is called rhinophyma. Other forms of phymata are gnathophyma (jaw/chin), metophyma (forehead), blepharophyma (eyelid) and otophyma (ear). Although all of these lesions are benign, they pose a challenge to patients due to their cosmetic and functional impairment.48 Systemic treatment options for phymatous lesions include low-dose doxycycline (40 mg/day) and low-dose isotretinoin (0.3 mg/kg / day). Both are supported by level A evidence. 26 Surgical techniques can also be used to treat phymatous changes and are in fact more effective. These techniques include excision, dermabrasion, electrocautery and laser ablation.48
Simple excision is a widely used method. However, since phymatous lesions have a large blood supply, removal of phymatous lesions may result in excessive bleeding, which is an undesirable complication. In addition, there is a risk of removing excess tissue. Dermabrasion can also be used to smooth the surface of the skin. However, like surgical removal, dermabrasion can also cause excessive bleeding.
Electrocoagulation is more effective in controlling bleeding compared to surgical removal. In addition, it is a faster method compared to simple excision. However, it hides the risk of necrosis of nasal cartilage due to excessive heat. In addition, atrophic scars and prolonged wound healing have also been reported when phymatous changes are treated with electrocautery.
The laser devices currently used to treat phymatous changes are the CO2 laser and the Erbium:YAG laser. Both of these lasers have a high affinity for water, which results in ablative changes because the skin has a high water composition.
Madan et al evaluated the effectiveness of CO2 laser in the treatment of rhinophyma. They demonstrated that during the three-month recovery period after a single treatment session, out of 124 patients, 115 were very satisfied with the results. In addition, the method had an acceptable side effect profile. CO2 laser is also good in hemostasis due to its coagulation properties.
Another combination therapy that can be used in the treatment of rosacea is Er:YAG and CO2 laser treatment.50 The CO2 laser is used for its coagulation properties when used together with the Er:YAG laser. Goon et al suggested that this combination therapy could achieve optimal cosmetic results with minimal scarring.
| Redness | Telangiectasia | PPR | Phymatosis | |||
| Current | Corticosteroids | Laser and light devices | Nd/YAG (1064 nm) | Current | Metronidazole cream (0.75-1%) | Oral doxycycline + low dose retinoid |
| Calcineurin inhibitors | KTP (532 nm) | Azeleic acid gel/foam (15%) | Excision | |||
| Brimonidine gel (0.5%) | PDL (595 nm) | Ivermectin cream (1%) | Dermabrasion | |||
| Oxymetazoline hydrochloride cream (1%) | LPAN (775 nm/ 1064 nm) | Pimecrolimus cream (1%) | Laser ablation | CO2 (10600 nm) | ||
| Ivermectin cream (1%) | RF | Retinoids (tretinoin 0.025% gel, adapalene gel) | Er.YAG (2940 nm) | |||
| Laser and light devices | PDL (595 nm) | Permethrin cream (5%) | ||||
| IPL (560 nm) | Benzoyl peroxide gel (5%) | |||||
| Systemic antihypertensive drugs | Carvedilol | Erythromycin gel (2%) | ||||
| Clonidine | Dapsone gel (2%) | |||||
| Intradermal Botox | Laser and light devices | Nd. YAG (1064 nm) | ||||
| PDL (595 nm) | ||||||
| RF | ||||||
| Oral antibiotics | ||||||
| Zinc sulfate | ||||||
| Oral ivermectin |
Conclusion
Rosacea is a common and lifelong condition that is distressing for patients. Although there are many treatments available for various manifestations of the disease, patients are usually not satisfied with the results. This is a challenge for dermatologists. There are many new treatments for erythema, telangiectasias, inflammatory lesions and phymatous changes that are resistant to conventional methods. Traditional and new treatments are summarized in Table 2. However, the relapsing nature of the disease reduces the likelihood of disease-free survival.
Symptoms of eye rosacea
Symptoms of ocular rosacea are most often mild, although it depends on how severely the eyes are affected. When the disease just begins to develop, the patient complains of pain in the eyes, increased lacrimation, and a burning sensation. There may be a feeling that there is a foreign body constantly present in the eye. Visual acuity may suffer already in the early stages of the disease.
The conjunctiva and white of the eye become bloodshot, swollen and red. During a visit to the ophthalmologist’s office, the doctor visualizes telangiectasias of the edges of the eye, persistent inflammation of the eyelid, and the presence of chalazions in the thickness of the eyelids.
For a long time, a person may try to treat conjunctivitis without success.
The ducts of the meibomian glands are sometimes blocked by yellow plugs. If you press your finger on the edge of the eyelid, a thick, opaque secretion will be released from the duct. Sometimes it looks like a paste.
As the cornea is damaged, the phenomena of keratitis and the growth of blood vessels into the stroma of the cornea itself are observed. At this time, vision decreases sharply, up to complete blindness. The vessels on the eye resemble twigs. This stage of the disease is characterized by the addition of cutting pain and severe photophobia. Ulcers and infiltrates may appear on the cornea.
Ignoring the symptoms of ophthalmic rosacea leads to the development of serious visual complications. The most dangerous of them are phlyctenular keratoconjunctivitis, corneal neovascularization, peripheral keratitis, conjunctival fibrosis, and ulcerative scleritis.
Causes of rosacea
The causes of the development of the disease have not yet been thoroughly studied, but a number of provoking factors are already known. Among them:
- hereditary predisposition,
- weak immune system,
- problems with the endocrine system and gastrointestinal tract.
Many scientists do not believe in the influence of genetics on this process. However, interesting studies were conducted in the United States and found that 40% of people with rosacea have relatives with this disease. And in the medical literature, cases of familial development of the disease have been recorded.
One of the most significant factors is mental state. Against the background of the disease, a depressed emotional state and depression occur.
Many scientists associate the development of rosacea with the activity of Demodex mites. In many cases this theory has been confirmed. But this is only one of the possible reasons. If mites are present, a diagnosis is made: “rosacea-like demodicosis.”
Various infections can also cause rosacea. Taking antibiotics reduces the rash. But so far it has not been possible to detect the viruses or bacteria that cause the disease.
Diagnosis of eye rosacea
Diagnosis of ocular rosacea begins with a standard examination of the patient. The doctor assesses the patient’s visual acuity, performs biomicroscopy and tonometry of the eye. It is imperative to interview the patient in detail to clarify whether there is a history of cutaneous rosacea.
As for additional examination methods, it is possible to conduct the Schirmer test and the Norn test. They allow you to determine the stability of the tear film and the quality of tear production.
During the examination, it is necessary to carry out a differential diagnosis with dry eye syndrome, allergic and toxic conjunctivitis.
Stages and special forms of rosacea
There are four stages of development of this unpleasant disease. The first stage is prerosacea. The skin of the cheeks and nose becomes covered with red spots that do not disappear for a long time. Sometimes a burning sensation is felt in the area of the spots. The second stage is vascular. The skin takes on a solid reddish color. Small blood vessels become visible on its surface. The third stage is inflammatory. Pustules appear - small pimples, sometimes with purulent contents. The fourth stage is late. Rhinophyma may appear - thickening of the skin in the nose area, accompanied by constant intense redness. Ocular rosacea is quite common. Here the characteristic signs are inflammation of the conjunctiva, eyelids, iris, cornea, and sclera. A combination of inflammatory changes is possible. There is redness and swelling. There is often a feeling of a foreign body in the eye and itching.
Treatment for eye rosacea
Most often, treating ocular rosacea is not difficult. Only when the disease is advanced may a long-term therapeutic course be required. To prevent this from happening, you should seek help from an ophthalmologist in the early stages of the disease. In addition to the main treatment, symptomatic therapy is carried out.
Gel with Metronidazole
Ocular rosacea, accompanied by demodicosis, requires the use of drugs based on Metronidazole. In ophthalmic rosacea, the parasite is found in the eyelash bed in 90% of cases. It is not difficult to identify it; it is enough to conduct a standard microscopic examination with the collection of eyelashes from both eyelids.
The following medications can be used to eradicate the parasite:
- Demalan ointment.
- Gel Stop Demodex.
- Gel Metrogyl.
The duration of treatment and the choice of medication should be determined by the doctor. If the drug was chosen correctly, then the inflammation process will fade away, and a control microscopic examination will not detect traces of the parasite in the eyelash bed.
Antibacterial drugs for topical use
If eye rosacea is accompanied by a bacterial infection, the patient is prescribed antibiotics. Bacteria that provoke skin inflammation in rosacea easily colonize the mucous membrane of the eye and conjunctiva. Therefore, bacterial conjunctivitis is a common companion to eye rosacea.
To get rid of inflammation, you will need to use the following medications:
- Eye drops: Ciprofloxacin, Ofloxacin, Tobramycin.
- Ointments: Erythromycin, Tetracycline.
These drugs have a wide spectrum of antibacterial activity and can cope with most microorganisms that affect the mucous membrane of the eye. When the therapy does not give the desired result, it becomes necessary to perform an antibiogram. This study allows us to identify which drugs the pathogenic flora is sensitive to. Then the patient is prescribed a second course of local antibacterial therapy.
Moisturizing the mucous membrane of the eye
Dryness of the mucous membrane of the eye is one of the common symptoms of rosacea. Insufficient hydration is caused by disturbances in the functioning of the meibomian glands, which overlap due to a number of factors (edema of the mucous membrane, parasitism of mites, hypertrophic changes in the skin of the eyelids). As a result, tear fluid quickly evaporates from the surface of the eye, causing dryness. To get rid of this phenomenon, you need to use special moisturizing drops. They need to be installed until rosacea can be completely eliminated.
Such drugs include:
- Oksial.
- Systane.
- Hilo chest of drawers.
Stimulation of metabolic processes
With rosacea, the natural metabolic processes that occur in the organs of vision are disrupted, as chronic inflammation is present. Any defects and injuries of the eyelid and conjunctiva take longer to regenerate, which negatively affects the patient’s well-being.
To normalize metabolic processes, you need to use drugs such as:
- Emoxipin.
- Solcoseryl.
- Taufon.
Relieving inflammation
If you do not get rid of inflammation, the person will experience severe discomfort. During an exacerbation of the disease, the use of hormonal drugs is permissible. However, only a doctor can prescribe them, having assessed all the benefits of the treatment. Preparations with a hormonal component are used for several days, but not for too long.
To eliminate the chronic inflammatory response, which is not associated with the risk of developing serious complications, you can use the following drugs:
- Indomethacin (Indocollir).
- Diclofenac (Diclo-F).
- ViziDol.
Disinfection of the skin around the eyes
Ointments and creams with an antibacterial component are used to treat the skin around the eyes. This could be Tetracycline or Erythromycin. They should be used from the very beginning of the therapeutic course. This is an excellent prevention of bacterial infection and other complications. In complex therapy, it is possible to use decoctions and compresses based on medicinal herbs.
Laser therapy for ocular rosacea is rarely prescribed. The laser can be used to eliminate cosmetic defects and remove the hypertrophied layer of eyelid skin. The decision about the need for laser therapy is made by the doctor.
What is rosacea?
Rosacea is a chronic skin disease that causes redness, pustules and other rashes, and if not treated properly, can cause eye damage.
People encounter this problem already in adulthood, usually from 30 to 50 years. Diagnosis is made by the appearance of the rash. It can be confused with acne. But the latter appears at a much earlier age and is distinguished by the presence of whiteheads.
Our clinic will provide you with qualified assistance in overcoming the consequences of this disease. It is especially recommended to undergo a course of phototherapy to eliminate telangiectasia, a vascular network that manifests itself at a certain stage in the course of rosacea. The Quantum photosystem truly works wonders.
Prevention and prognosis
If the patient follows all the ophthalmologist’s prescriptions, the prognosis for recovery is favorable. Although in some cases treatment lasts for several months.
To prevent the development of ophthalmic rosacea, exposure to negative factors on the eyes should be minimized. All people over 45 years old should be examined by an ophthalmologist every year. Basic recommendations boil down to maintaining a healthy lifestyle, giving up bad habits, and regular exercise. All diseases of the digestive system must be properly treated. If inflammation of the facial skin due to rosacea is stopped in time, the disease will not spread to the organs of vision.
Author of the article: Marina Vitalievna Degtyareva, ophthalmologist, ophthalmologist