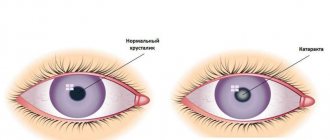
Cataract is a pathology of the visual organ in which visual acuity is lost. Translated from Greek, this word means “splash of a waterfall.” The patient sees surrounding objects as if through a veil of water, regardless of their distance. Inside the eye is the lens, which is an optical lens. Rays pass through it and are subsequently displayed on the retina. This is how visual images of objects are created on which a person concentrates his gaze.
With the development of cataracts, the protein components in the structure of the lens are destroyed, it becomes cloudy, and loses its physiological ability to normally perceive what is happening around it. The flow of light is disrupted, visible objects are distorted. This disease belongs to the category of rapidly progressing. Within a few years, the patient may completely lose vision. Often cataracts occur in both eyes at the same time; surgery becomes the only way to help the patient regain full vision.
Stages of diabetic cataract
The stages of deterioration of the eye do not differ from other forms of cataract:
- initial;
- immature;
- mature;
- overripe.
The initial stage is characterized by one or several lesions on the periphery. At this stage, the patient is practically not worried about anything. The disease is detected accidentally during a preventive examination. Immature cataracts are characterized by the fusion of pathological foci and the movement of opacities to the iris. The chamber is swollen, blurred vision appears. When examining the eye, healthy tissue remains under the damaged fibers. A mature cataract progresses rapidly, the protein becomes cloudy over the entire area of the chamber. The patient does not see objects, only the areola and the light source. Overmature cataracts are characterized by tissue decay and fiber destruction. It is very difficult to restore vision; blindness occurs.
Causes and symptoms of senile cataracts
Cataracts usually develop in older people after age 50. The second name of the pathology is senile disease (the word “senilis” translated from Latin means “senile”). Among the prerequisites for the development of the disease at this age are:
- diabetes;
- myopia;
- infectious diseases;
- prolonged exposure to ultraviolet radiation;
- glaucoma;
- exposure to toxic fumes.
All these factors can act one at a time or several at the same time. They lead to loss of transparency of the lens. The main reason for the development of age-related cataracts is the natural aging process in the body. They are accompanied by the following irreversible processes:
- the formation and accumulation of free radicals that destroy cell membranes;
- an increase in the level of insoluble proteins and, conversely, a decrease in soluble proteins;
- decrease in the concentration of substances such as amino acids, ATP, enzymes;
- changes in the composition of intraocular fluid.
Often patients do not pay attention to a slight deterioration in vision. They consider this a common age-related manifestation, unaware of the course of the latent phase of the disease. The following signs should be the reason for consulting a doctor:
- general deterioration of vision;
- discomfort in the eye area;
- “floaters” before the eyes, bright circles and flashes;
- clouding of the pupil, which is visible from the side with the naked eye;
- blurred outlines of objects;
- development of “night blindness”;
- double vision, blurred lines;
- transition from farsightedness to nearsightedness;
- excessive sensitivity to light, which was not there before.
It is important to establish the stage of development of the disease in order to select the appropriate treatment regimen.
Symptoms of diabetic cataracts
Specialists at the laser vision correction center highlight the main signs of diabetic cataracts:
- the appearance of flickering before the eyes;
- foreign body sensation;
- reduced image clarity;
- increased photosensitivity;
- reduction of image brightness;
- distortion of the perception of the object, double vision;
- rapid fatigue of the organ of vision.
If these symptoms occur, the patient should take care of his eyes and contact an ophthalmology clinic.
SIGN UP FOR A CONSULTATION
Extracapsular extraction
This is the most common and effective method of cataract removal. The operation involves removing the optical lens without the use of expensive equipment. Indications for extracapsular extraction include corneal dystrophy and weak ligamentous apparatus. This operation helps with excessively narrow pupils, partial rupture of ligaments and diagnosed secondary cataracts, the development of which was caused by the disintegration of the optical lens.
The entire lens is removed through an incision in the membrane of the eyeball. This is the main disadvantage of the operation, since the patient needs stitches. In the future, symptoms of astigmatism are often observed. The patient complains that he cannot clearly see objects that are close to his eyes.
The rehabilitation process is long, in some cases it can take up to 6 months. Recovery should be carried out under the supervision of the attending physician, strictly following the indications recommended by him. Extracapsular extraction helps restore vision even at the stage of overripe cataracts. It is prescribed for secondary ophthalmological pathologies or for a hard lens. The posterior capsule can be preserved, which prevents the vitreous from prolapse into the anterior chamber.
Diagnosis and treatment of diabetic cataracts
Making an appointment at the Tarus clinic involves using all available methods for diagnosing the disorder:
1. The ophthalmologist interviews the patient about complaints. 2. Measures the fundus. 3. Sets the field of view. 4. Evaluates microcirculation. 5. Examines the eyes with an ophthalmoscope.
Based on the results of the examination, the doctor draws up an individual treatment plan for the patient. Drug treatment is carried out to improve microcirculation, eliminate dry eye, reduce swelling and reduce pain. A radical method of solving the problem is cataract surgery. The phacoemulsification method has proven itself well. It consists of crushing the damaged tissue and removing it out through the device.
Stages of surgery to remove overripe cataracts
Surgery is almost always performed on an outpatient basis. 3-4 days before surgery, the patient is prescribed a course of drug therapy for prophylactic purposes to reduce the risk of complications.
Before the procedure, the patient is given painkiller drops. The operation takes place in several stages:
- An incision in the cornea to create access to the lens. The procedure is performed with a special instrument that allows the surgeon to act as accurately as possible.
- Formation of a hole in the anterior capsule of the lens.
- Removal of a clouded lens. This is the most critical stage.
- Implantation of an intraocular lens.
- Applying a bandage.
There are no overlaps during the operation. If there are no complications after surgery, the patient can be discharged home on the same day.
Preparing for surgery
Before cataract surgery is scheduled, the doctor assesses the patient's general condition. Due to the specifics of the disease, it is necessary to take into account the indications and contraindications for the intervention. Laser phacoemulsification is performed after a stable decrease in sugar levels has been achieved. The regeneration of structures during the disease, even after microintervention, is impaired; fluctuations in glucose can worsen the condition even further.
Method of treatment
Treatment of overripe cataracts with medications and physical therapy is not effective. Vision can only be restored through surgery, which also carries risks.
To determine treatment, doctors carefully evaluate the risks. Surgery is performed when it does not threaten the patient's life.
Ultrasound is used to remove the lens. A device is inserted through an incision in the cornea, which turns the lens masses into an emulsion, which is removed using special instruments. An intraocular lens is placed in place of the lens.
The advantage of visiting the Tarus clinic
The state eye clinic often does not have the ability to provide quality care due to limited funding. The Tarus Center in Odessa has the most modern equipment. Thanks to this, examination and treatment of the patient, even in complex cases, takes a limited amount of time. The clinic’s licenses and certificates confirm the high level of care provided. The clinic’s doctors have the right to train abroad, which significantly improves the quality of their work.
SIGN UP FOR COMPREHENSIVE VISION DIAGNOSTICS
Cataract
Encyclopedia of Health / Encyclopedia of Diseases
Cataracts can be overcome, even if they are inevitable.
OPTICAL FOCUSES
A cataract is any clouding of the lens of the eye, even one that does not reduce visual acuity at the moment. It can occur at any age.
congenital cataracts , caused by disturbances in the intrauterine development of the fetus. Or complicated - usually develops in middle-aged or young people against the background of systemic diseases of the body or under the influence of harmful environmental factors, for example, increased doses of radiation. Traumatic cataract is usually a consequence of injury or contusion of the eye. But the most common is senile (age-related), which sooner or later affects more than half of the world's population.
ON THE CLEAR EYE
And yet, more often than not, we do not know why cataracts developed. It is known that changes in the structure of the lens occur against the background of a shift in general metabolic processes. Damaging factors also include ultraviolet radiation - southerners have cataracts more often than northerners, so in sunny weather everyone is recommended to wear glasses, and not just dark ones, but with special filters that protect against ultraviolet radiation. After all, the lens is a lens inside the eye, without blood vessels or nerve endings and covered with a capsule.
Over the years, the lens begins to thicken, change its color, and then lose transparency.
There is an opinion that catarrh is an inevitable consequence of the aging of the body.
If doctors knew the true causes of the disease, perhaps they could prevent it and offer conservative treatment - for example, drops. But such methods are still unknown to ophthalmologists around the world. There are antioxidant drops, popularly called “vitamin” drops, which supposedly delay the development of the disease. “Supposedly” - because no one knows exactly according to what laws cataracts develop. Sometimes in people who take these drops and lead a healthy lifestyle, the disease still progresses quickly, while in others, relying on chance, it hardly moves at all. So for now, the surest way to recover is to replace the diseased lens with an artificial one.
CAUGHT RED-ANDED
There is a myth that it is impossible to “catch” cataracts at an early stage without sophisticated equipment. In fact, a simple slit lamp and average medical experience are enough. In some forms of the disease, you can even suspect something is wrong.
If the cataract is “central”, with clouding in the center of the lens, the person immediately notices a deterioration in vision.
First of all, its sharpness changes under different lighting conditions. Some people begin to see better in the twilight than in bright light. This is especially dangerous for drivers: in clear weather everything is dimly visible, and when blinded by oncoming traffic, there is a complete veil of fog before your eyes. Another initial sign: a person was reading with “plus” glasses, but suddenly he began to see better up close, but worse at distance. It would seem, where does myopia come from? Due to changes in the structure of the lens and its refractive ability. The shape of the lens remains the same, but its core becomes denser, and it turns out something like a lens within a lens.
“OVER-MATURATE” OPERATION
Very often, eye surgeons are faced with advanced stages of the disease. And, sadly, sometimes through the fault of doctors who still tell patients: “Cataracts must mature. Wait." So, at first glance, it is easier to operate. And the patient, suffering for several years, waits. Vision gradually deteriorates, and a person comes to the doctor when the eye no longer sees anything - it only senses light. In addition, when a cataract matures, the lens sometimes not only becomes cloudy and hardens, but also begins to swell and increase in size: the surrounding tissues suffer, and intraocular pressure increases. The situation is getting dangerous. Often, due to loss of time, other, more serious diseases develop, such as glaucoma.
| WHOM SHOULD YOU TRUST FOR CATARACTS? When choosing a clinic for surgery, be on the safe side: 1. Make inquiries from ophthalmologists at several clinics. They observe patients after surgery and know how well their colleagues work. 2. Talk to your surgeon. A rude, heartless doctor is rarely a good specialist. 3. Don't be scared of private clinics. Today they are not only not inferior to the state ones in terms of the level of qualifications of specialists, equipment and service, but often surpass them. 5. The patient has the right to participate in the choice of model. Traditional "plastic" lenses with a rigid design are very reliable, but require a larger incision (about 5 mm). The soft, elastic lenses of the latest models raise the cost of surgery by $150–200 or more. 6. Abroad, phacoemulsification will cost more, but even there the patient will not receive anything beyond what they can offer in Russia. Moreover, in the West, a specialist who has performed about 500 operations is considered experienced. Leading Russian ophthalmic surgeons perform thousands of phacoemulsifications. |
You should not wait for the cataract to mature: this worsens both the course of the operation and its prognosis. If your doctor encourages you to delay treatment, it makes sense to consult another specialist.
The only “justification” for a wait-and-see approach is the use of old techniques, which actually make it technically easier to remove mature cataracts. A large incision is made in the cornea (about 12 mm), the lens capsule is opened, the affected tissue is washed with saline, an artificial lens is inserted and the cornea is sutured. In this case, astigmatism inevitably occurs - an irregular shape of the cornea: where it is stretched more, the refraction is greater, and where it is weaker, less. Try bending a plastic spectacle lens in boiling water and then inserting it into the frame - the same thing happens when suturing the cornea. And the anesthesia required by this technology is not always pleasant and safe.
This method is called extracapsular cataract extraction and has been used since the late 60s of the last century. Unfortunately, this technology is still used en masse and is paid for through the compulsory health insurance system. There are not always enough specialists and equipment to implement modern treatment methods. But if you seriously care about your health, it is better to pay money and cure the disease at an early stage in a modern clinic.
FIGHT FOR MICRONS
Phacoemulsification is one of the new ways to remove cataracts. The lens, measuring 9–10 mm in diameter, is removed through a 3 mm incision in the eye. To do this, a small amplitude oscillation is created at the end of the needle (approximately 40 thousand per second): the nucleus of the lens is destroyed and is sucked out through the same needle.
But how can a new lens be implanted through a 3 mm hole, which with attachments reaches 12–13 mm? Using a special instrument (injector), the lens is inserted into the eye cavity in a folded state, and there it straightens. Technologists are struggling to create an artificial lens that can be implanted through an even smaller incision, and are looking for ways to relieve the side effects of microvibration of an ultrasonic needle. The fight is for microns. It has already become technically possible to operate through a 2 mm incision. Since it is valved, its profile is similar to a step, the incision closes itself. No stitches are required to seal the eye.
CALM, ONLY CALM! The operation is quite easy. Instead of the traditional “heavy” anesthesia - retrobulbar injection (in simple terms - an injection “behind the eye”), local anesthesia with drops is used. There is no pain, but tactile sensitivity remains: you feel that you are being touched. The operation lasts approximately 10–15 minutes, then the patient gets up, changes clothes, drinks tea and calmly goes home.
In standard cases, after phacoemulsification, the bandage is removed the next day, and within a month the patient himself instills drops into the operated eye and is seen by the doctor from time to time. Since vision is completely restored, you can start working with virtually no restrictions. No bed rest! Previously, after surgery, it was forbidden to bend over (this was due to the implantation of certain models of artificial lenses), and to use a gas stove - now all these prohibitions have been lifted.
With a good diagnosis and a standard situation, when the problem is only clouding of the lens, the failure rate is about 4–5%. Moreover, this is often expressed in slightly worse visual acuity than expected, and not in blindness.
Doctors often perform surgery when vision is 80–90% - when the patient’s profession requires 100%, as, for example, for a surgeon.
Risk factors are high intraocular and blood pressure, concomitant diseases, say, diabetes. If there is a serious failure, it is sometimes difficult to repeat the operation, but this is a feature of eye surgery. So choose your clinic and surgeon very carefully.
What happens to the lens as you age?
If you have read previous posts, you are already very familiar with the cornea. This is the first most powerful refractive lens of the eye; it is formed at approximately 16–18 years of age and changes slightly throughout life. Next we have the second “group of lenses” - lenses (lens - natural lens in English terminology). And behind it, through the vitreous body, there is a sensor, that is, the retina.
The lens is responsible for the refraction of light (about +20 diopters at rest and about +30 diopters when stressed) and focusing the eye. When we look at a book, the muscles tense and shape it so that the focus falls on the letters. When we look at a plane in the sky, the muscles relax and the lens forms almost parallel rays. The muscles are not located in the lens itself, but in the area of the so-called ciliary body; the lens ligaments are attached to them, which, in turn, allows for accommodation, that is, this precise adjustment to the desired focal length by changing the shape of the lens. If you take out the lens at all, you will see with glasses somewhere between +10 and +15 diopters.
With age, the lens gradually becomes dense and cloudy. In a young person, the lens usually contains only 60–65% tissue water. In old age, the amount of fluid decreases. Although the lens “floats” in liquid, it itself is relatively dry. On the other hand, in the lens itself, due to its structure and the absence of blood vessels, there are no tumor or inflammatory processes. The lens does not hurt because it has no nerve endings.
Often, as cataracts develop, they cause a weakening of presbyopia and the ability to read without glasses, that is, two age-related pathologies suddenly correct each other. But this is an imaginary improvement in vision, the image quality is poor - this is a significant symptom of the development of cataracts.
At about 60–70 years of age, the lens completely loses its ability to accommodate, that is, it becomes hard, large and inelastic. The lens also turns yellow with age.
Yes, it must be said that cataracts are not necessarily an age-related phenomenon. There are congenital cataracts (if during pregnancy a woman suffers from certain infectious, systemic or genetic diseases).
There are complicated types of cataracts that appear with concomitant diseases of the eyes or the body as a whole, for example, diabetes, arthritis, etc. Taking certain medications can also cause cataracts.
And, of course, any injury to the eye can cause cataracts, even if there was no direct contact with the lens. It is now known that cataracts are caused by strong infrared radiation, as well as various radiation factors, and not immediately, but years later. This, in particular, calls into question the use of powerful lidars of unmanned vehicles operating in the infrared spectrum - while their effect on the eyes has not been studied in the future for several years. It is also known that ultrahigh frequency current also leads to the development of cataracts. Cataracts can also be caused by poisoning, in particular (very typical) with nitro paint. In animals, cataracts have been learned to be produced predictably with naphthalene and specific diets.
But let's return to ordinary age-related cataracts. A very characteristic symptom of the beginning of the process is that the patient thinks that his glasses are “dirty”, and there is a constant desire to wipe them. If you suddenly notice this in an elderly relative, it means it’s definitely time to change the lens.
Sometimes patients misinterpret the symptoms that appear. Very often, cataracts mature by thickening the lens - along the sclerotic path. In this case, the patient with cataracts, who was reading with glasses, suddenly begins to notice with surprise that he can now see poorly with them and it becomes possible, albeit in the “fog,” to read the text without glasses. The patient feels joy and thinks that he can see better. Alas, this is a bad symptom! He says you need to schedule a visit to the ophthalmologist.
Often cataracts cause myopia, which has been stable for years, to suddenly begin to worsen. Sometimes to enormous values - -20 diopters or more. In general, frequent changes of glasses are an early sign of cataracts.
The second option for cataract maturation is no better - hydropic, when the lens begins to increase in volume, becomes waterlogged, swells and leads to an increase in intraocular pressure and rapid loss of vision.
There are also a number of symptoms: at dusk it becomes better to see than during the day, rainbows and double vision are disturbing, astigmatism appears or increases. In general, cataracts are very diverse in their manifestations; it is impossible to make a diagnosis on your own; this requires a visit to an ophthalmologist.
Phacolytic iridocyclitis
Iridocyclitis is an inflammatory process of the iris and ciliary body. This consequence can be caused by cataracts at the stage of overripeness.
This consequence of cataracts is manifested by the following symptoms:
- headache,
- eye pain,
- the appearance of a red or bluish network of vessels in the limbus (the area at the border of the cornea and sclera),
- impaired pupil mobility,
- a change in the color of the iris to greenish due to the penetration of red blood cells and their destruction.
The consequences of iridocyclitis can be adhesions between the iris and the lens.
Treatment consists of prescribing anti-inflammatory drugs
preparations, drops to dilate the pupil (this helps reduce swelling and other inflammatory phenomena). After the acute stage of the disease subsides, the issue of removing the lens is decided.
How is treatment and IOL selection performed?
Cataract surgery is performed on an outpatient basis in a comfortable environment for the patient using local drip anesthesia. This means that there will be no painful sensations, and after the procedure is completed, the patient returns home. Modern high-precision equipment and the use of the latest techniques make it possible to remove the clouded lens without waiting for the cataract to fully mature.
The method of phacoemulsification , used to remove cataracts, is based on the impact of ultrasound or laser on the lens tissue to soften it. In a softened state, the lens is removed from the eye through a micropuncture that does not require sutures. Through the same hole, an intraocular lens is inserted into the eye. New generation artificial lenses are made from biocompatible materials with memory. This allows the lens to take the desired shape inside the eye and securely lock into the desired position.
Modern IOLs allow additional vision correction at different focal lengths. Depending on the characteristics of the patient’s visual system, the most suitable artificial lens is selected, which will help get rid of glasses. To accurately select an artificial lens, a detailed examination of the organs of vision is required to calculate the required optical power of the IOL. Depending on the indications, aspheric, multifocal, toric or trifocal intraocular lenses can be used.
Obscurational amblyopia
Obscuration amblyopia is a common consequence of congenital cataracts in children.
Most often, congenital cataracts are accompanied by the presence of small opacities of the lens, which do not progress and do not affect the refraction of this structure. However, when the lens becomes completely clouded, irritation of the retina by light rays stops. Due to the lack of visual information entering the brain, the retina is “switched off” from the visual act.
In other words, the healthy retina stops functioning. This is a serious consequence of congenital cataracts, which can lead to disability in childhood.
Treatment of ocular amblyopia is surgical. It must be carried out before changes to the retina become irreversible. Timely removal of the lens and installation of an intraocular lens can restore vision and avoid blindness.