Previously, patients who had cataracts removed had to wear thick glasses to see anything. Now a new lens is inserted into the eye, and the eye begins to see well. This procedure is widely used by doctors at the Maerchak Laser Eye Microsurgery Clinic. If you need advice from an ophthalmologist regarding lens replacement, please contact us and we will answer all your questions.
Toric IOLs - what are they?
Intraocular lenses are artificial lenses that are implanted into the patient's eye to replace the cloudy natural lens.
The cloudy lens is removed from the eye using ultrasound and water. Toric IOLs combine the properties of cylindrical and aspheric lenses. This lens has a special shape: the back wall is aspherical, and the front wall has different radii. It is thanks to its shape that the toric artificial lens compensates for the defect in the optics of the eye and relieves the patient from both cataracts and astigmatism.
Selection of intraocular lens (IOL) for ultrasound phacoemulsification of cataracts
The doctor gives recommendations on the choice of IOL for cataracts, taking into account the patient’s refractive characteristics, his activity, financial capabilities, age and other factors. Ultrasound phacoemulsification of cataract surgery is performed after selecting the optimal IOL option.
At the Eye Surgery Center, ultrasonic removal (phacoemulsification) of cataracts involves the installation of soft IOLs. These systems can be placed into the lens capsule even through a small incision, after which they are straightened and take on their final shape.
IOLs can be:
- Monofocal are systems that have one focus. In other words, if a patient has a cataract with a combination of nearsightedness and farsightedness, a monofocal IOL will provide good distance vision. At the same time, you will need to select glasses for near vision.
- Multifocal IOLs are IOLs that have several foci and provide the patient with cataract surgery with good distance and near vision.
Both mono- and multifocal intraocular lenses, according to reviews from numerous patients, have their advantages and disadvantages, which the doctor informs the patient about.
Why is toric IOL implantation necessary?
Toric IOLs are needed in particularly complex cases of eye pathology:
- For the treatment of cataracts with astigmatism
- After a cornea transplant or in case of corneal pathologies, including in case of trauma
- Toric IOLs may be contraindicated in patients with advanced glaucoma (high intraocular pressure)
- Iritis (inflammation of the iris)
- Iridocyclitis (inflammation of the iris and ciliary body of the eye)
- And degenerative processes in the cornea of the eye.
Toric intraocular lenses
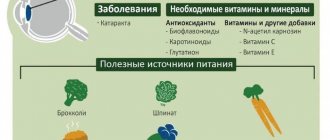
In ophthalmological practice, a combination of cataracts and astigmatism is often encountered. If “cataract” is widely known to modern people as clouding of the lens, then the more specialized term “astigmatism” needs clarification and means an anomaly in the development of the cornea or lens (non-spherical shape), in which the optics of the eye cannot focus the light flux at one point - i.e. . independent sharp and clear vision is impossible for geometric reasons. According to statistics, corneal astigmatism is more common than lens astigmatism, and due to the greater refractive power of the cornea, its non-sphericity creates more noticeable visual impairment than lens astigmatism.
As in general medicine, ophthalmology distinguishes between physiological disorders - transient, not significantly affecting the quality of life - and overt pathology, subject to medical intervention or, otherwise, significantly limiting self-realization and social functioning. Thus, astigmatism with a severity of less than 0.5 diopters is considered functional; such an anomaly often occurs at a young age and is compensated over time by the natural development of tissues and structures of the eye. However, more pronounced degrees of astigmatism (more than 2.0 diopters) require medical correction and do not go away on their own. A special problem is age-related astigmatism, in which it is often very difficult to choose adequate and effective glasses.
Cataracts in combination with astigmatism were previously considered as a complex pathology, amenable only to palliative correction: even after a microsurgical operation to replace the affected lens with an implant, the patient needed special glasses “with cylinders.” However, to date, the development of methodology and technology has made it possible to develop special, toric, lenses that can compensate even for combined types of astigmatism and cataracts. One of the promising models is the AcrySof Toric lens. Without going into very special details, we note that such IOLs are a “smart” optical solution, which, thanks to the high refractive index and ultra-precise calculation of the geometry, can largely (and sometimes completely) correct the “error of nature” and compensate for corneal astigmatism.
In the most common cases, toric lenses are indicated:
- for cataracts;
- with astigmatism to a degree of 0.75-3.0 diopters;
- with acquired astigmatism (injuries, consequences of infections, etc.);
- for diseases of the cornea of the eye;
- if it is necessary to re-correct unsuccessful operations or postoperative complications, as well as to correct the consequences of corneal injuries;
- with severe astigmatism after corneal transplantation (which, as a rule, makes it extremely difficult to select effective glasses or contact lenses).
The toric IOL does not require any special microsurgical technique. To replace a cataract-damaged lens with a toric implant, the widely practiced and long-established operation of phacoemulsification is performed. A microscopic entrance incision is made (no more than 2.5 mm), which does not require any postoperative sutures and is sealed naturally, due to natural protective and restorative processes. The total duration of microsurgical intervention does not exceed 10-15 minutes; Hospitalization is not required, the operation is performed “in one day.” Powerful drip anesthesia provides reliable pain relief without overloading the cardiovascular system - which eliminates a number of contraindications, primarily age-related. The rehabilitation period is short and imposes only minimal restrictions and requirements (mainly of a hygienic nature) on the usual lifestyle in the postoperative period.
At the same time, a toric intraocular lens not only takes on the optical functions of the removed lens affected by cataracts, but also makes the necessary optical corrections for comorbid (accompanying) corneal astigmatism.
However, optics is not forgiving of errors, and most of the methodological problems of implanting toric lenses are associated with this. The precision accuracy of such an artificial lens in each case requires a thorough and error-free diagnosis of the existing anomaly, as well as high qualifications of the operating ophthalmic surgeon. Thus, the correct location of the intraocular implant along the axes and planes is critically important, since only in this case it is possible to achieve satisfactory correction of astigmatism. Therefore, for diagnostic purposes, to clarify the picture of optical pathology, as well as to select the most adequate implant, high-precision computerized hardware systems are used.
In addition, when selecting a toric type IOL, specialists at the Moscow Ophthalmological Center take into account medical history and individual characteristics of the patient: age, characteristics of professional activity, severity of pathology, presence of underlying diseases, and many others. Each toric artificial lens is a one-piece, highly individual product of high technology and ophthalmic science, so in most cases a certain waiting period is inevitable before the actual operation. The result, however, makes all the difficulties and worries worth it. In our ophthalmology center it is possible to install a toric lens from the world leader in ophthalmology - the German company Carl Zeiss. This makes it possible to achieve high treatment results in patients with various forms of astigmatism.
How is toric IOL implantation performed?
Before the operation, the doctor conducts a complete examination of the patient’s vision to identify possible contraindications and eliminate the risk of complications. Next, the ophthalmologist selects the IOL according to the individual characteristics of the eye, so that the artificial lens is as comfortable and invisible as possible after installation.
The implantation procedure takes 10–20 minutes and is performed under local drip anesthesia. The ophthalmic surgeon removes the cloudy lens using ultrasound, vacuum and water, and then through a microscopic puncture of up to 2 mm places a folded IOL in the eye. The toric lens is distributed in place of the natural one, and the puncture is sealed with water - no seams.
2–3 hours after the operation the patient is allowed to go home. To eliminate discomfort, doctors apply a drop of anesthetic to the eye.
At the Eye Clinic of Dr. Belikova, IOLs of all types are used: multifocal, toric, phakic. We use only high-quality artificial lenses from world brands - ALCON (USA), HumanOptics and Carl Zeiss (Germany), Hoya 251 (Japan) and others.
Rehabilitation period
Upon completion of the cataract lens replacement procedure, the postoperative period may take 2-3 weeks. During rehabilitation, physical activity is contraindicated for the patient, and visual stress on the eye in which the lens was replaced should also be limited. It is recommended to regularly instill special drops into the eyes, prescribed by the doctor, and follow a number of simple recommendations.
The attending physician will schedule follow-up examinations. As a rule, the patient should undergo a follow-up examination on the second day after surgery, on the seventh day, after one month and after three months. The examination schedule may vary depending on the individual characteristics of the patient and the need to monitor his condition.
If no complications arise and all rehabilitation rules are followed, vision should improve noticeably within a month.
Should we wait until the patient becomes completely blind?
Patients often use this logic: as long as the eye sees something, there is no need to operate on the lens.
In fact, today, on the contrary, the lens is operated on as early as possible, when it is already clear that an irreversible process has begun. The reason - in addition to protection from risks caused by changes in metabolism in the eye, is that the softer the lens is at the time of surgery, the less invasive the method will be used, and the lower the risk of complications. The pooled worldwide risk of severe to serious complications from lensectomy is around 6%. In the case of late stages, it can reach 20–30%. In the early stages it is 1–2%. In the case of using modern access equipment, very precise selection of the lens-implant itself and more than 5 years of experience of the surgeon - less than 1%. What influences the risks so much, I will tell you in the next post, when we talk directly about the progress of the operation.
Another important point is that you yourself will never be able to determine on your own what condition your lens is in. There are a number of factors that force surgeons to recommend surgery at an earlier stage: weak ligamentous apparatus of the lens, short or, conversely, long eyes, eyes with a shallow anterior chamber, the condition of the corneal endothelium and other things that can only be assessed by a specialist who performs operations on this particular subject. type. Quite often, outpatient doctors act as advisors, but they are not always well versed in the surgical technique and the indications for lens replacement. By reassuring the patient with the words “you have an immature cataract, it’s too early to operate,” they do the patient a “disservice” - inaction leads to the optimal time being missed.
In general, cataract surgery in ophthalmology is like appendicitis surgery in general surgery. It is considered the most basic and most predictable in the standard case, the most creative in the non-standard case. If everything goes according to the scenario, even an inexperienced surgeon will get a good result. If something goes wrong (and this cannot always be predicted in advance), then only an experienced surgeon will be able to find a way out of the unusual situation. I have to very often, almost weekly, undergo reconstructive surgeries after unsuccessful surgeries in other clinics. Sometimes the volume of such surgery is enormous - operations lasting not 10-15 minutes (as with standard cataracts), but 1-2 hours of “creativity”.
An important point in cataract surgery is the choice of lens. And the main factor is taking into account the individual characteristics of a particular patient. Models of IOLs (intraocular lenses) differ in the material of manufacture, the shape and number of supporting elements, the structure of the optics (spherical, aspherical, astigmatic), and the method of attachment. Therefore, it is better to choose not an American or German one, “like your neighbor’s,” but the one that your surgeon considers most suitable for your eye.
And the most important. Lens replacement restores optical clarity and may improve the optics of the eye, but it will not create a new eye. If there are concomitant problems with the retina, optic nerve, cornea or brain, that is, there are other problems with vision loss, then these will ultimately determine how you see after surgery. That is, post-operative visual acuity will be as you visual analyzer as a whole.
Ultrasound phacoemulsification
At the Eye Surgery Center, a complete vision diagnosis is carried out and indications for ultrasound phacoemulsification of a clouded lens are determined. This operation has the following advantages:
- no need for stitches;
- efficiency;
- individual selection of IOLs;
- rapid recovery after phacoemulsification surgery.
The operation is performed by experienced specialists: high qualifications and many years of successful practice are a guarantee of a stable positive result for the patient. The set for Phacoemulsification surgery includes modern instruments that ensure minimal tissue trauma and high precision of the surgeon’s manipulations in the treatment of cataracts.
Cataracts are curable! You can make an appointment with an ophthalmologist by calling.
Cost of services
| Operation | rub. |
| Computer phacoemulsification with implantation of a flexible multifocal IOL Restor (USA) (prepayment for 1 eye 45,000) | 103 000 |
| Computer-assisted phacoemulsification with implantation of flexible multifocal IOL Lentis (USA) (prepayment for 1 eye 45,000) | 103 000 |
| Computer-assisted phacoemulsification with implantation of a multifocal toric IOL Lentis (USA) (prepayment for 1 eye 70,000) | 128 000 |
| Computer phacoemulsification with implantation of a flexible multifocal IOL Rayner M-flex (England) (prepayment for 1 eye 33,000) | 91 000 |
| Computer-assisted phacoemulsification with implantation of a flexible toric IOL Rayner (England) (prepayment for 1 eye 20,000) | 78 000 |
| Computer phacoemulsification with implantation of a flexible toric IOL Rayner (England) (in complicated cases, on a single eye) (prepayment for 1 eye 20,000) | 88 000 |
| Computer phacoemulsification with implantation of a flexible toric IOL Acrysoft IQ Natural (USA) (prepayment for 1 eye 23,000) | 81 000 |
| Computer-assisted phacoemulsification with implantation of a flexible toric IOL Acrysoft IQ Natural (in complicated cases, on a single eye) (USA) (prepayment for 1 eye 23,000) | 91 000 |
| Computer-assisted phacoemulsification with implantation of a flexible multifocal toric IOL Rayner (England) (prepayment for 1 eye 50,000) | 108 000 |
| Computer phacoemulsification with implantation of a flexible multifocal IOL Zeiss Atlisa (Germany) (prepayment for 1 eye 45,000) | 103 000 |
| Computer phacoemulsification with implantation of a flexible trifocal IOL Zeiss Atlisa (Germany) (prepayment for 1 eye 60,000) | 118 000 |
| Computer phacoemulsification with implantation of a flexible multifocal toric IOL Zeiss Atlisa Toric (Germany) (prepayment for 1 eye 60,000) | 118 000 |
| Computer phacoemulsification with implantation of a flexible toric IOL Zeiss At Torbi (Germany) (prepayment for 1 eye 35,000) | 93 000 |
| Computer phacoemulsification with implantation of a flexible toric IOL Zeiss At Torbi (Germany) (in complicated cases in a single eye) (prepayment for 1 eye 35,000) | 103 000 |
| Computer phacoemulsification with implantation of a flexible trifocal IOL Panoptix Alcon (prepayment for 1 eye 60,000) | 118 000 |
| Computer phacoemulsification with implantation of a flexible toric IOL Panoptix Alcon (prepayment for 1 eye 75,000) | 133 000 |
| Computer phacoemulsification with implantation of a flexible IOL (made in the USA or England) ( on promotion , without discount) | 38 000 |
| Computer-aided phacoemulsification with implantation of a flexible Bi-Flex IOL (discounts do not apply) | 45 000 |
| Computer phacoemulsification with implantation of flexible IOL Rayner (England) aspheric | 58 000 |
| Computer-assisted phacoemulsification with implantation of a flexible Rayner IOL (England) (in complicated cases, on a single eye) | 68 000 |
| Computer-assisted phacoemulsification with implantation of flexible IOL Acrysoft Natural (USA) | 62 000 |
| Computer-assisted phacoemulsification with implantation of a flexible IOL Acrysoft Natural (USA) (in complicated cases, on a single eye) | 72 000 |
| Computer-assisted phacoemulsification with implantation of flexible IOL Acrysoft IQ Natural (USA) | 73 000 |
| Computer phacoemulsification with implantation of flexible IOL Acrysoft IQ Natural (USA) (in complicated cases, on a single eye), Alcon 3-piece IOL | 83 000 |
| Computer-assisted phacoemulsification with implantation of a flexible Tecnis IOL (USA) | 75 000 |
| Computer-assisted phacoemulsification with implantation of a flexible Tecnis IOL (USA) (in complicated cases, on a single eye) | 85 000 |
| Computer-assisted phacoemulsification with implantation of a flexible Zeiss IOL (Germany) | 79 000 |
| Computer-assisted phacoemulsification with implantation of a flexible Zeiss IOL (Germany) (in complicated cases, on a single eye) | 89 000 |
Fill out an application on the website, we will contact you as soon as possible and answer all your questions.
Make an appointment
When is the lens removed?
There are three types of indications for lens replacement: optical, refractive and medical.
Optical readings are when the aging and compaction of the “onion” in layers has reached its logical end and the lens darkens. When cataracts begin to reduce vision qualitatively or quantitatively. Feelings as if smoked glass had been inserted into the eye or as if you were looking at the world through glass splattered with semolina. Even initial cataracts, which cause decreased vision, require removal.
The old term “immature” is not a reason to wait for ripening. A diagnosis of cataract is a reason to replace the lens.
When a person no longer sees objects and only light perception remains, this is the last stage of mature cataracts. It is better not to bring it to this point, in particular because changes in the lens cause numerous disruptions in the normal functioning of the eye. In mature and overripe forms, the lens capsule and ligamentous apparatus suffer; removal requires a large amount of ultrasonic energy, which, in turn, destroys the cornea and its delicate endothelial layer. In general, if you delay replacing the lens, you should be prepared for the fact that the operation will be longer and more traumatic, with a long recovery period.
Refractive readings are changes in the optics of the eye. By replacing the lens and correct calculations of the optical power of the implanted artificial lens, we can change the refraction of the eye to the desired value - save the patient from a large “minus” or “plus”, correct astigmatism, and get rid of age-related farsightedness. In this case, cataracts do not develop, and the optics of the eye remain stable forever.
This method is most often used for patients over 40-45 years of age, when the first symptoms of presbyopia appear.
Medical indications are when your own lens is the cause of concomitant changes in the eye, for example, when there is a subluxation after an injury and there is a risk of its dislocation, when it causes the formation of glaucoma (a dangerous increase in intraocular pressure and death of the optic nerve), etc. That is, again, to simplify, sooner or later the lens will still need to be changed, but due to the risk of pathologies, sometimes it needs to be changed a little earlier than it has exhausted its resource.