Corneal endothelial dystrophy, or Fuchs', is an inherited disease that affects the inner layer of the cornea (endothelium). It performs the function of a pump, constantly pumping out from the thickness of the cornea the liquid of the anterior chamber (aqueous humor), which enters there under the influence of normal intraocular pressure. If there is an excess amount of fluid in the cornea, its transparency decreases. The cornea then becomes like frosted glass.
As the disease progresses, patients gradually lose endothelial cells that are unable to divide. The remaining cells are spread out on the vacated area. Until a certain time, the condition of the organ of vision is compensated by the increased work of the cells that remain. Then the pumping system becomes less efficient, and the cornea becomes swollen and cloudy. Ultimately, visual acuity decreases.
The disease is more common in women than in men. It appears between the ages of 30 and 40, affects both eyes and gradually progresses.
Fuchs syndrome
This is a type of disease called anterior uveitis. It usually develops in people after thirty years of age. Elderly patients are also at risk. However, a similar anomaly can also appear in a child. In young patients, it is easy to treat and does not cause complications.
In 4% of all cases, Fuchs' dystrophy occurs in patients diagnosed with uveitis. But even in the presence of the disease, the syndrome is sometimes difficult to identify, since its course is not accompanied by pronounced symptoms.
It is most difficult to detect the disease in brown-eyed people, since it is almost impossible to see that the shade of the iris has changed. But this is one of the main signs of pathology.
| It is still unknown exactly what causes the development of corneal dystrophy. But the majority of ophthalmologists are inclined to believe that the appearance of the syndrome is a consequence of inflammatory processes occurring in the body. |
Signs (symptoms) of Fuchs' dystrophy
In the early stages of Fuchs' dystrophy, there is usually increased intolerance to bright light and glare. As the disease progresses, vision deteriorates in the morning and recovers somewhat in the evening. This is due to the fact that when the eyes are closed during sleep, moisture from the surface of the cornea does not evaporate, accumulating inside. During the day, open eyelids “turn on” the mechanism for removing intraocular moisture from the cornea, and a temporary normalization of the condition occurs. The progressive death of more and more endothelial cells leads to a gradual decrease in vision.
The main signs of endothelial dystrophy are considered to be the following:
- Deterioration of vision after sleep, blurry vision.
- Fluctuations in visual acuity.
- Glare (glare) when looking at a bright light source.
- Poor tolerance to intense light.
- Discomfort and feeling of sand in the eyes.
Fuchs endothelial dystrophy is characterized by bilateral damage. The disease is more common in women after 30-40 years of age. In case of serious deterioration of vision, when the ability to self-care is lost, the question of a corneal transplant arises.
Causes of Fuchs syndrome
It has not yet been possible to establish the exact etiology of the disease. In rare situations, a genetic predisposition can be traced. Also, the activation of the disease can be caused by inflammatory processes of various origins occurring in the orbit of the orbit. This assumption is confirmed by the fact that the pathology causes vision problems.
Also, the development of Fuchs syndrome is often diagnosed in patients with neurodystrophic pathologies in the anterior region of the choroid. Risk factors include impaired sympathetic innervation of the cervical spine and diseases of the vasomotor center.
The cause of the disease in children is prenatal or postnatal iritis. In practice, ophthalmologists have encountered the disease in patients suffering from iridocyclitis of tuberculous origin. Return to contents
Symptoms
Endothelial-epithelial dystrophy of the cornea affects the iris and ciliary body. The disease is accompanied by the following symptoms:
- Since the composition of intraocular moisture changes, after some time clouding of the lens is observed;
- As the iris thins, it becomes lighter. The patient's eye color changes;
- After some time, the damaged eye becomes much darker than the healthy one. A similar phenomenon is observed after the iris becomes thinner and the lacunae expand. The pigment sheet of the iris begins to appear through them;
- In some cases, the development of secondary glaucoma is diagnosed;
- Dystrophy develops in the processes of the ciliary body. The result of the destructive process is the sedimentation of the protein and the release of the eyeball in the anterior chamber.
| In some cases, the symptoms stop for a while and the person believes that he has recovered. In fact, if left untreated, the symptoms will return after a while. |
General information
The causes of this phenomenon can be congenital and acquired. The various forms can be asymptomatic or cause severe visual impairment, they can appear at different ages, but still have similar characteristics:
- most forms of the disease have a bilateral course;
- progress slowly;
- do not affect other organs;
- As a rule, inherited in an autosomal dominant manner, they are found in many representatives of the same family.
What is corneal dystrophy in terms of anatomy and physiology? This is the accumulation of abnormal structures in its layers, which make the cornea cloudy and do not allow it to perform its functions - refract light and direct it deep into the eyeball to the lens.
Layer-by-layer structure of the cornea
Corneal dystrophies are characterized by the accumulation of pathological changes in cells that can occur in each of its five layers:
- epithelial (outer protective layer);
- anterior limiting membrane (Bowman's membrane is the strongest and physically does not allow hostile agents to penetrate deep into the cornea);
- stroma (the main layer, which is the thickest and consists of water and collagen fibers, which gives it strength, elasticity and transparency);
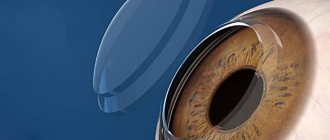
- posterior limiting membrane (Descemet's membrane, which, despite its small thickness, also acts as a protective layer);
- endothelial (the innermost layer, consisting of specialized cells that pump excess water out of the cornea).
Symptoms of dystrophy are common in many forms and include recurrent erosion, discomfort or severe pain, abnormal sensitivity to light (photophobia), foreign body sensation (such as dirt or eyelashes) in the eyes, and blurred vision. These symptoms are caused by dystrophic changes. That is, a violation of cellular metabolism, which leads to structural damage, as a result of which the function of the organ changes.
The mechanisms of trophism (nutrition) are divided into cellular and extracellular. The latter depend on the circulation of blood and lymph, the body's neurohormonal regulation system, and intracellular ones are based on disturbances in the transfer of molecules across the membrane and damage to the enzymatic system of the cell. One way or another, dystrophies almost always have a genetic cause.
An international classification of corneal dystrophies has been developed, which takes into account the chromosomal loci of various corneal dystrophies, as well as the responsible genes and their mutations. Traditionally, dystrophies are classified based on their clinical manifestations and the specific damaged layer.
Possible complications
Fuchs syndrome is a type of chronic uveitis. If you ignore the pathology and delay a visit to the doctor, it can develop into cataracts or glaucoma. The reason lies in the uncontrolled use of medications from the group of corticosteroids.
In most cases, the majority of patients inevitably face the development of glaucoma. When complicated by Fuchs syndrome, the pathology can lead to complete loss of vision. Cataract is accompanied by all the symptoms inherent in this anomaly. It can also lead to hyphema (bleeding into the anterior chamber of the eye).
Corneal dystrophy: severity of eye damage and possible consequences
The cornea is a completely transparent structure. It is important for the optical function of the eye. This is a strong center of refraction of light rays. It must have the correct ellipsoidal shape (11-12 mm horizontally and 1 mm at a time). The element is the first focusing optical center. It serves as a specific barrier that protects the inside of the eyeball. The layer of tear film is also important. It provides constant hydration and glide
Without this, the optical center will not be able to function, which is what they pay attention to
Failure to regenerate the endothelium can lead to corneal decompensation. This threatens the penetration of fluid into the anterior chamber. Stenosis may appear. The most important optical functions of the cornea are disrupted. Turbidity or unevenness of the surface makes it impossible to correctly perceive light rays. These changes are associated with the presence of a very strong decrease in visual acuity. Pain in such cases is caused by rupture of epithelial vesicles. This leads to exposure of the sensory endings of the cornea. Symptoms are more severe in the morning. The reason for this is reduced evaporation of fluid from the cornea during sleep. This can cause serious problems.
Surgery for corneal problems
A common form of dystrophy that occupies the corneal stroma. The disease is idiopathic. It has an uncertain or unknown background. This is primary corneal amyloidosis. With this change, amyloid deposits penetrate through the keratocytes. The onset of symptoms occurs at the turn of the first and second decades of life. Corneal pathology manifests itself in the form of periodic epithelial erosions.
Disorders and consequences of damage to the cornea can affect all its layers. In most cases, the treatment used will restore normal function. Sometimes this is not possible. In this situation, the only solution is corneal transplantation. The condition for performing the operation will be not only a specific pathology
The general condition of the patient is also important. This applies to some chronic diseases that can worsen the prognosis
For transplantation, a donor cornea is required. Transplants (material taken from the second eye) are rare. As with all organ and tissue transplant procedures, there are special rules. They identify a list of medical diagnoses that may serve as an indication for a transplant.
Diagnosis of corneal endothelial dystrophy
To identify the disease, contact and non-contact examination methods are used. Ultrasound pachymetry helps measure the thickness of the cornea using a special machine. It is not used if the integrity of the membrane is violated and in the presence of inflammation of purulent origin. Optical pachymetry is also used, the essence of the procedure is to measure the thickness of the cornea using a slit lamp.
Popular diagnostic methods include endothelial microscopy. In an image taken using special equipment, the doctor measures the number of endothelial cells.
In a healthy person, the thickness of the cornea ranges from 490 to 560 micrometers. The indicator may change throughout the day, but if it exceeds the mark of six hundred micrometers, this signals the development of pathological processes. Representatives of the stronger sex have a slightly smaller cornea (545 microns) than women (555 microns).
It is believed that the result of an ultrasound examination is more accurate than the optical method of measuring shell thickness. In the first case, the patient is in a supine position, an anesthetic substance is injected into the eye and a special attachment is attached to it. The result of the study is displayed on the computer.
During the procedure using an ophthalmic microscope, the patient takes a sitting position, and a unique device is attached to the forehead and chin. The doctor analyzes the condition of the eye, moving the stream of light to the right place. At the same time, he rotates the handle of the slit lamp, measures the thickness of the cornea and records the data on a special scale.
One of the simplest diagnostic methods is endothelial microscopy. It not only allows you to measure the thickness of the cornea, but also count the number of cells. The technique gives a visual representation of the state of the endothelium. The equipment automatically determines the number of cells per square millimeter of tissue. A normal indicator is considered to be a density of up to a thousand cells per square millimeter; if it decreases, then clouding of the cornea is observed.
Ribbon dystrophy (degeneration) of the cornea
Band-shaped corneal dystrophy (degeneration) is a slowly growing superficial clouding in blind or low-vision eyes.
Ribbon-shaped corneal dystrophy develops several years after severe iridocyclitis, choroiditis in eyes blinded due to glaucoma or severe trauma. Opacities occur against the background of altered sensitivity of the cornea, decreased mobility of the eyeball and decreased metabolic processes in the eye. With increasing atrophy of the muscular system, involuntary movements of the eyeball (nystagmus) appear. The opacities are located superficially in the area of Bowman's membrane and anterior epithelium. The corneal stroma and posterior layers remain transparent. The changes begin at the periphery of the cornea at the inner and outer edges and, slowly increasing, move to the center within the open palpebral fissure in the form of a horizontal ribbon. From above, where the cornea is covered by the eyelid, it always remains transparent. The opacities are distributed unevenly; there may be islands of the transparent surface of the cornea, but over time they also close. Band-shaped degeneration is characterized by the deposition of calcareous salts, so the surface of the cornea becomes dry and rough. When such changes are long overdue, thin plates of keratinized epithelium, impregnated with salts, can be torn off on their own. The raised salt outgrowths injure the mucous membrane of the eyelid, so they must be removed.
Gross opacities and salt deposits in the cornea are formed against the background of pronounced general trophic changes in the blind eye, which can lead to subatrophy of the eyeball. There are cases where calcareous deposits formed not only in the cornea, but also along the vascular tract of the eye. Ossification of the choroid occurs.
Such eyes are subject to removal followed by cosmetic prosthetics. In eyes with residual vision, a superficial keratectomy (cutting off the cloudy layers) is performed within the optical zone of the cornea (4-5 mm). The exposed surface is covered with epithelium growing from the intact upper part of the cornea, and can remain transparent for several years if the patient regularly instills drops that support corneal trophism and applies ointments that prevent keratinization of the epithelium.
Ribbon-shaped corneal dystrophy in children, combined with fibrinous-plastic iridocyclitis and cataracts, is characteristic of Still's disease (Still's syndrome). In addition to the triad of eye symptoms, polyarthritis, enlargement of the liver, spleen, and lymph glands are noted. After a course of anti-inflammatory treatment for iridocyclitis, cataract extraction is performed. When opacities in the cornea begin to cover the central zone, a decision is made to perform a keratectomy. Treatment of the underlying disease is carried out by a therapist.
Treatment
Most methods of conservative therapy used for corneal degeneration slow down destructive processes and make the patient feel better. Among medications, doctors recommend eye drops and ointments that block tissue destruction. These include medications such as Taufon, Emoxipin, etc. Additionally, vitamins are prescribed and physiotherapy is prescribed.
A saline solution will help reduce the manifestation of negative symptoms; it attracts moisture and rids the cornea of excess fluid. Contact lenses can help reduce pain.
Surgery will help completely restore visual acuity, but since in most cases it causes serious complications, doctors prescribe it only if the ability to see has become less than ten percent. The operation is performed using a laser, the affected part of the cornea is removed.
| If the damage has penetrated deep into the outer shell of the eye, penetrating keratoplasty (complete transplantation of the shell and installation of donor tissue) or layer-by-layer keratoplasty (replacement of affected areas of the cornea) is used. However, surgery does not eliminate the risk of relapse. In this case, repeated intervention is performed. |
Return to contents
Treatment methods
Depending on the concomitant eye diseases, the optimal method of surgical correction is chosen, for example, implantation of an artificial lens.
Hereditary corneal dystrophy
The hereditary form of dystrophy is corrected with the help of vitamin preparations and instillation of vitamin-containing medicinal solutions. Sometimes a drug to improve soft tissue trophism can help. If vision is severely reduced, a corneal transplant or keratoplasty is performed.
However, the hereditary form of dystrophy cannot be completely cured, and even in the case of corneal transplantation, re-development of the pathology is possible. After a few years, patients again show signs of thinning of the stratum corneum. Repeated transplantation can significantly improve the condition of the visual organ; as a rule, patients manage to restore vision.
Edema dystrophy
At the initial stage of pathology progression, the installation of glycerin and glucose, vitamin therapy and correction of soft tissue trophism help. Swelling of the epithelial layers of the cornea is treated with antibiotics, antibacterial ointments and drugs to accelerate tissue regeneration. In some cases, laser stimulation of the cornea gives positive results. In case of severe swelling and thickening of the cornea, penetrating subtotal keratoplasty is performed.
Band-shaped dystrophy
If vision is completely lost, the diseased organ is completely removed and an artificial eye is implanted. Typically, the ribbon-like form of corneal degeneration is formed due to injury or the development of glaucoma. If vision is partially preserved, the clouded layers of the cornea are cut off (keratectomy). Subsequently, the patient is prescribed drugs to activate epithelial restoration and tissue regeneration.
Endothelial epithelial corneal dystrophy
Unfortunately, no cure for this pathology has been found. Surgery can only slow down the rapid development of dystrophy and delay the onset of blindness. Additional measures to the main surgical treatment are physical procedures - helium-neon laser stimulation and magnetic therapy.
Donor tissue transplantation is used to replace cloudy layers of the cornea. However, all types of surgical correction have side effects—various types of complications. Therefore, in modern ophthalmology, cryokeratoplasty is used, a more gentle method of correcting the corneal layer.
Crosslinking
This minimally invasive treatment method involves photopolymerization of the corneal connective protein collagen. It is used for any form of dystrophic change in the epithelium. The operation does not require hospital conditions. The diseased eye is anesthetized using drip anesthesia, then the corneal layer is saturated with riboflavin and irradiated with ultraviolet light. The eye is closed with a contact lens and sent home. At home, the patient is required to keep the lenses clean and adhere to the treatment regimen determined by the ophthalmologist.
Prognosis and prevention
There are no specific measures to prevent the development of the pathology, since the exact reasons that provoke the appearance of the anomaly are still unknown. If dystrophy is detected, it is necessary to visit an ophthalmologist at least twice a year, who carries out a number of diagnostic measures (visometry, tonometry, gonioscopy, etc.). This will prevent the development of complications such as cataracts and glaucoma.
It’s also worth reviewing your diet, taking a vitamin-mineral complex, and putting your sleep and rest patterns in order. Most often, doctors give a favorable prognosis for the treatment of Fuchs syndrome. For a long time, the pathology occurs without pronounced symptoms and does not in any way affect the usual way of life.
However, if treatment is delayed, cataracts or glaucoma may join dystrophy. In this case, there is a high risk of complete loss of vision and disability.