Indications Contraindications Crosslinking stages Price Our advantages
Corneal crosslinking is an effective, low-traumatic technique used to treat a number of pathologies of the cornea, in this case, keratoconus, as well as other diseases. This method was developed by prof. T. Seiler in the late 90s. last century and was used to treat patients with keratoconus and postoperative keratoectasia (a complication of laser vision correction). Nowadays, the corneal cross-linking technique is also gaining widespread use in the treatment of various dystrophic lesions of the cornea.
Mechanism of action and indications
The corneal crosslinking method is based on the ability of the stromal collagen fibers of the cornea to undergo certain changes under the influence of certain physical or chemical factors. It was found that the combined effect of ultraviolet rays on the cornea in the presence of riboflavin (vitamin B2) causes a photopolymerization reaction of collagen fibers, which leads to their compaction and increases the biomechanical properties of the cornea.
In addition, riboflavin and ultraviolet rays have an anti-edematous and antibacterial effect. Thanks to these effects, in this period corneal crosslinking is triumphantly used as an effective method for treating keratoconus, as well as various dystrophic pathologies of the cornea (keratopathies, corneal ulcers, Fuchs' dystrophy with pain syndrome, keratomalacia).
Advantages of the crosslinking method and technique
Crosslinking has significant advantages over traditional operations on the cornea, thanks to which it has gained well-deserved popularity:
- The method is safe and highly effective;
- Suitable for patients with extremely low corneal thickness and opacity;
- The effect significantly increases the strength of the cornea and improves its structure;
- It is possible to combine with other methods of correcting the shape of the cornea;
- The result is long-term, while corneal transplantation may be needed after a long time or may never be needed;
- The technique is simple to perform, minimally invasive and affordable.
Crosslinking of corneal collagen is carried out under local anesthesia, which is achieved by instilling special drops into the conjunctival sac. The operation occurs with or without removal of the surface layer of the epithelium of the cornea - transepithelial. When the procedure is performed transepithelially, the surface of the cornea is not injured. This method is more comfortable for patients.
Classic corneal crosslinking includes several stages:
- Removing the top layer of the cornea mechanically - with a spatula on a circle with a diameter of 9 mm, lasts no more than a quarter of an hour, is necessary to facilitate the penetration of the photosensitizer (vitamin B2) into the underlying layers of the membrane;
- Soaking the cornea with riboflavin (30 minutes before the start of irradiation), examining the shell in a slit lamp, during which the surgeon determines the degree of its moisture with a riboflavin solution;
- Exposure of the cornea to ultraviolet light for 30 minutes;
- Instillation of eye drops with antibiotics and anti-inflammatory components;
- Placement of soft lenses in the eye for protection for the entire rehabilitation period (until the cells of the surface layer are restored).
During the action of ultraviolet light on the treated cornea, a chemical reaction occurs between the collagen fibers, which seem to stick together, giving the shell strength. The light source is located at a distance of about a centimeter from the treatment area, focusing the light at the top of the corneal cone. The dose of ultraviolet radiation that the patient's eye receives during treatment is comparable to that at solar noon.
The corneal crosslinking operation lasts approximately an hour and a half and is performed on an outpatient basis. After its completion, you can leave the clinic, having received all the necessary recommendations from the ophthalmologist. It is advisable to think in advance who will help you get home, and you will have to temporarily give up driving a car.
Although the transepithelial cross-linking technique is among those used in some clinics, there is still debate about its features. It is clear that low trauma and a lower risk of complications are very attractive with the transepithelial approach, but the effectiveness of this technique is also lower compared to irradiation of the cornea, which is devoid of epithelial cover. In addition, insufficient exposure may further contribute to the progression of keratoconus.
Ophthalmologists around the world are actively researching ways to make the transepithelial approach more effective. To improve the penetration of riboflavin into the intact cornea, various drugs are used (benzalkonium chloride, EDTA), which reduce the bond strength between the epithelial cells of the cornea. There is evidence of the possibility of using iontophoresis, which promotes deeper saturation of tissues with riboflavin.
Many ophthalmologists consider a more promising method of cross-linking for keratoconus to be a technique that involves preliminary exposure of the cornea to a femtolaser. The laser beam forms a ring-shaped channel in the cornea, into which a riboflavin solution will then be injected. This method does not require removal of the epithelial layer, does not cause pain, is safer and is better tolerated by patients.
Video: crosslinking of the cornea - video of the operation
Stages of the procedure
Before the operation begins, the patient is given eye drops containing an anesthetic. After the onset of anesthesia, the doctor applies an eyelid speculum and, using an eye spatula, carefully removes the top layer of the corneal epithelium (this is necessary to improve the penetration of the vitamin B2 solution into the thickness of the cornea). Within 15–20 minutes, a riboflavin solution is instilled into the eye, at the same time the doctor examines the cornea using a slit lamp and evaluates how evenly the vitamin B2 solution penetrates the corneal tissue.
Upon reaching the required degree of saturation with the riboflavin solution, the corneal tissue is treated with low-intensity ultraviolet rays for 30 minutes, which avoids damage to the deeper structures of the eyeball. Under the influence of ultraviolet light, collagen fibers located in the cornea are welded together and form a strong frame that is resistant to stretching.
At the end of the procedure, antibacterial eye drops are instilled into the eye to prevent inflammation, after which the operated surface of the cornea is protected with a special therapeutic soft contact lens. Throughout the entire healing period of the cornea (an average of 3 - 5 days), the patient must wear a treatment lens and instill anti-inflammatory drops.
Features of surgical technique and complications
This intervention is outpatient, that is, at the end of the procedure, the patient can leave the clinic after receiving appropriate recommendations and setting a date for a follow-up visit to the doctor. Typically, corneal crosslinking is performed in a sterile operating room under local anesthesia.
Technically, there are 2 options for performing crosslinking:
- With removal of the epithelial layer. Under local anesthesia in the form of eye drops, the epithelium is excised. Before the procedure, ultrasound pachymetry is performed to determine the minimum thickness of the de-epithelialized cornea. This is necessary so that the thickness of the cornea is at least 400 microns. 0.1% riboflavin is applied to the surface of the cornea every 3 minutes for 30 minutes. The saturation of the cornea with riboflavin is monitored using a slit lamp. It is a sufficient concentration of riboflavin that ensures the formation of free radicals and protection of the underlying layers of the eye from UV rays. Then UV radiation is carried out for 30 minutes using a special optical system. During the procedure, a solution of riboflavin and a local anesthetic are applied to the cornea every 2-3 minutes. After the procedure, antibiotic prophylaxis is necessary, and a special contact lens is installed until complete re-epithelialization.
- Without removing the epithelial layer (transepithelial cross-linking). This intervention is less painful and more comfortable for the patient. To weaken interepithelial bonds and better penetration of riboflavin, special substances are used. One of them is benzalkonium chloride. It is a surfactant that weakens intercellular connections, facilitating sufficient penetration of riboflavin to the underlying layers of the cornea. Otherwise, the essence of the procedure remains unchanged.
One of the big questions that still worries many specialists in this field is whether transepithelial cross-linking allows one to obtain results comparable to a more invasive technique (excision of the epithelium). A lot of scientific research is being conducted in this direction, which currently has very contradictory results. In European countries, the use of a special type of riboflavin (RicrolinTE) has been introduced, which also promotes deeper penetration of riboflavin.
The undeniable advantages of cross-linking without removing the epithelial layer are a reduced risk of infectious complications and a reduced likelihood of corneal opacification. This method also promotes faster recovery after surgery and less discomfort.
Possible complications of corneal crosslinking:
- Temporary stromal edema (up to 70% of patients), temporary blurred vision or permanent blurred vision (up to 10% of patients).
- Cicatricial changes in the cornea and sterile infiltrates.
- Infectious keratitis: bacterial or herpetic.
Contraindications
The corneal cross-linking procedure is not performed on persons under 18 years of age. Contraindications are also small (less than 400 microns) thickness of the cornea in any dimension, inflammatory eye diseases in the acute phase, decompensation of internal diseases (this mainly applies to pathologies of the cardiovascular or respiratory systems), and mental illness. If it is necessary to perform cross-linking on both eyeballs, the minimum interval between operations is 3 months.
Indications for cross-linking:
The main goal of the procedure is to inhibit the development of pathological changes in the cornea, therefore the main diseases for which cross-linking is recommended are:
- Keratoconus
- Marginal pellucidal corneal degeneration
- Therrien's marginal degeneration
- Ectasia after refractive surgery such as LASIK, PRK or radial keratotomy
Complications of crosslinking
In most cases, the prognosis for cross-linking is favorable. At the same time, like any invasive intervention, the procedure can have a number of complications. Possible complications include:
- temporary visual impairment (recovery of visual acuity is observed within 1 to 4 months after the procedure);
- reversible decrease in corneal transparency that does not affect visual acuity;
- slow (up to 1 month) restoration of the corneal epithelium;
- redness and irritation of the eyes, in rare cases - the development of keratitis;
- activation of herpetic infection with the development of herpetic lesions of the cornea.
Progress of the operation
The cornea crosslinking operation has two types: traditional and transepithelial. Let's look at how the procedure works using the traditional technique.
Progress of the operation:
- The patient sits in a chair. Body position: reclining with head thrown back.
- A local drip of anesthesia is performed (an anesthetic is instilled into the eye, this is quite enough).
- For better viewing and fixation, an eyelid speculum is installed.
- When the anesthetic takes effect, the thinnest top layer of the cornea is mechanically peeled off. This stage is very important, as it allows drugs to penetrate into the deep layers of the cornea. The duration of the stage is about 15 minutes.
- Next, riboflavin is administered over half an hour. It is important that the drug is absorbed evenly.
- The next stage is a control inspection. Necessary to determine how well riboflavin is distributed.
- Next, exposure to ultraviolet light is carried out for half an hour.
- After the main stages of the procedure, drops with antibiotics and anti-inflammatory components are instilled into the eye.
- A soft protective lens is placed in the eye, which the patient will wear throughout the recovery period.
The entire procedure is performed on an outpatient basis and lasts about one and a half hours.
If crosslinking is performed using the transepithelial technique, then the top layer of the cornea is not removed, and all other steps remain the same.
In scientific circles there is still a division of specialists into two camps. Some are adherents of the traditional method, others use the transepithelial method.
The advantage of the transepithelial crosslinking method is that it is less traumatic and has a shorter recovery period. But the traditional method is more effective, as proven by many years of research.
Advantages of corneal crosslinking in MGC
A favorable outcome of any medical procedure is determined by a combination of several main factors, which include accurate diagnosis, selection of the most effective treatment method, high qualifications of the attending physician, and high-quality management of the postoperative period. Each patient of the Moscow Eye Clinic is guaranteed to receive all these benefits.
Thanks to the clinic being equipped with the best examples of diagnostic equipment from global manufacturers, a diagnostic examination allows you to detect any eye pathologies, takes a compact period of time and is carried out in comfortable conditions. On the day of the examination, the patient receives the results of the examination with a transcript of the detected abnormalities and the doctor’s recommendations.
The clinic employs some of the best specialists in the capital. The treatment of corneal pathologies at the Moscow City Clinical Hospital is carried out by Professor, Doctor of Medical Sciences. Alexey Yurievich Slonimsky is one of the most authoritative domestic specialists in the treatment of patients with various corneal pathologies (cataract, corneal dystrophy, keratitis), a recognized leader in the field of end-to-end corneal transplantation for keratoconus. The corneal crosslinking procedure is performed by an ophthalmologist, Ph.D. Kishkin Yuri Ivanovich.
Our clinic is open seven days a week, from 9 a.m. to 9 p.m., seven days a week. For the convenience of patients, there is a day hospital, where each patient can receive the necessary support.
Recovery after crosslinking
In the first days, the person operated on may feel pain and discomfort in the eye; bright light and other irritants will cause negative sensations. During the recovery period, it is better to avoid exposure to bright light, being in a dusty room, watching TV, working at the computer, and even reading. When regeneration is complete, you can safely return to your usual activities.
If cross-linking occurred transepithelially, without damaging the cornea, recovery will occur much faster. There will be no need for strict restrictions, and the patient will return to work sooner.
Recovery after treatment will require compliance with some rules:
- Careful daily eye hygiene;
- Use of antibacterial drops - before removing lenses 4 times a day;
- Instillation of anti-inflammatory drugs into the eyes for two months according to the regimen prescribed by the ophthalmologist;
- It is recommended to remove lenses no earlier than three days after cross-linking.
Full recovery after crosslinking takes 1-2 months, sometimes six months, but corneal regeneration is usually completed by day 5, and by the end of the first month the patient will notice improved vision. To monitor the effectiveness of treatment, the ophthalmologist will examine your eyes regularly: daily until the soft lenses are removed, then after 1, 3, 6 months and a year.
Crosslinking is considered a safe treatment method. However, complications are possible and are usually short-term. Adverse consequences may include:
- Cloudiness of the cornea - does not reduce visual acuity, resolves in the first months after the procedure;
- Slow regeneration of the epithelial layer, lasting for a month;
- Short-term visual impairment;
- Irritation of the mucous membrane lasting up to two weeks;
- Recurrence of herpes;
- Keratomalacia is very rare.
The listed complications are more likely with cross-linking with removal of the surface epithelial layer, therefore, after such an operation, patients should especially carefully follow the doctor’s recommendations and undergo regular examinations during the first year after treatment.
Crosslinking cost
The cost of the corneal crosslinking procedure at the Moscow Eye Clinic is 30,000 rubles. for one eye. Prices for other medical services at MGK can be found here.
All questions you are interested in can be asked to specialists by calling the MGK hotline 8(800)777-38-81 (toll-free from mobile phones and regions of the Russian Federation) and the number in Moscow 8(499)322-36-36 or online using the appropriate form on website.
Indications for the procedure
The main indication for this procedure is keratoconus. With this ophthalmological pathology, the cornea of the eye thins, becomes denser and, under the influence of intraocular pressure, bulges - changes its shape from spherical to conical. Such changes entail deterioration of vision. A patient with keratoconus may see surrounding objects in a blurred, distorted form, and his visual acuity is reduced.
Cross-linking, by helping to strengthen the mechanical strength of the cornea, can stop the progressive development of keratoconus and make the cornea more resistant to the effects of intraocular pressure. Other indications for surgery may include the following diseases and pathological conditions:
- Iatrogenic keratectasia is a long-term complication of vision correction surgery (anterior keratotomy);
- secondary keratoconus - corneal dystrophy caused by trauma, inflammatory diseases and other reasons;
- corneal ulcers;
- Corneal keratomalacia is a lesion of the eye tissue caused by a lack of vitamins.
Personalized (local) UV crosslinking in the treatment of keratoconus and corneal ectasia
S.I. Anisimov, S.Yu. Anisimova Glaznoy LLC, Moscow
Relevance of the problem • The number of diagnosed keratoconus and other, including iatrogenic, corneal ectasia is increasing. • The number of iatrogenic keratoectasias increases after laser correction of ametropia and in the long term after anterior radial keratotomy. The main pathogenetic prerequisites for keratoconus and other corneal ectasia • Biomechanical changes - uneven changes in the strength characteristics of corneal tissue. • Morphological changes - local deviations from the normal curvature and thickness of the corneal layers. • The occurrence of an imbalance in the biomechanical parameters of the cornea, leading to a discrepancy between the strength of the cornea and the mechanical stresses generated in it by IOP.
At the same time, new diagnostic possibilities for keratoconus have now emerged.
1. Precision measurement of IOP is possible, taking into account the influence of corneal rigidity by determining corneal compensated IOP (Pcc). 2. Changes in the curvature and thickness of the cornea are recorded quite accurately using modern topographers with the possibility of optical pachymetry; in particular, Orbscan II (Bausch+Lomb) is well suited for this.
Using a computer, it is possible to calculate mechanical stresses using the Laplace equation, taking into account the parameters of the pachymetric and topographic map. This makes it possible to construct a map of the distribution of mechanical stresses over the entire area of the cornea. For this new type of topographic map, we proposed the term “keratotensotopogram.” In Fig. 1 on the calculated keratotensotopogram (map below), the red arrow indicates areas of reduced corneal rigidity. They are located concentrically in the paracentral region of the cornea.
There is another way to identify areas of reduced stiffness in the cornea. To implement this, the topogram is taken twice. The first time in normal condition, and the second time - after a vacuum-compression load of 80 mm Hg. After subtracting the data from these two topograms (in the differential topogram mode), zones of reduced rigidity appear, which are localized in the same area that is also detected in the calculation method. In Fig. 2 are represented in blue by the zones that responded with protrusion and, therefore, weakened (marked by arrows). It is noteworthy that these areas are located where corneal segments are usually implanted. That is, it can be assumed that the mechanism of action of the corneal segments with this distribution of corneal stiffness in keratoconus is mainly based on an increase in the strength of these paracentral regions. It should also be noted that often observed in keratoconus, after keratotomies or in other cases of corneal deformation, for example, with pterygium or after antiglaucomatous operations with pronounced filtration pads, Flasher pigment deposits appear precisely in areas corresponding to areas of increased mechanical stress. For keratoconus, after hypermetropic LASIK, concentrically in the form of rings, after keratotomies in the center of the cornea. Perhaps this phenomenon is an indicator of those areas of the cornea in which remodulation processes are activated in response to increasing tensile loads.
Based on a study of keratotensotopograms in corneal ectasia, we hypothesized that the refractive effect of crosslinking in these conditions could be enhanced by targeting only areas in which stiffness is reduced. The concept of such an impact is reflected in Fig. 3. By changing the shape of the irradiation zones when exposed to UV radiation, it is possible to flatten or increase the curvature of the cornea in the central zone.
To implement this concept, a special device was developed that allows the cornea to be irradiated with different patterns depending on which area of the cornea needs to be irradiated based on preliminary calculations (type and design of the device in Fig. 4). The diaphragm to form the pattern was cut out using a special cutting printer, then placed in a machine that projected the pattern onto the cornea. The cornea was soaked with riboflavin after de-epithelialization of the cornea within the upcoming local irradiation zone for 30 minutes, 1 drop of 0.1% riboflavin every 2 minutes. In this case, the radiation power and exposure time corresponded to the usual protocol: 3 mW/cm2 for 30 minutes with additional irrigation of the cornea with a riboflavin solution every 5 minutes.
In Fig. 5 and 6 are examples of obtaining myopic and hypermetropic correction effects.
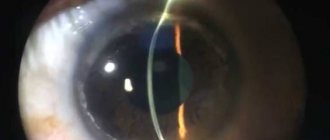
Another positive effect of local crosslinking is that areas that have not been irradiated are less susceptible to aggressive ultraviolet radiation. In Fig. Figure 7 shows that the central zone of the cornea, which was shaded, is not affected by haze, in contrast to traditional cross-linking (image on the right in Fig. 7), the corneal syndrome goes away faster and the rehabilitation period of patients after the procedure is accelerated.
Rice. 8 demonstrates faster vision recovery after local crosslinking compared to the traditional method.
Finally, an important condition for obtaining a good visual result is the use of local cross-linking in the initial stages of keratoconus, before the possibility of obtaining an elastic response of the cornea to the procedure is lost. This dependence is shown in Fig. 9.
conclusions
• Local crosslinking is effective in the treatment of keratoectasias. • Local cross-linking is more effective in the early stages of keratoconus. • Local crosslinking has a pronounced controlled refractive effect. • Local cross-linking helps reduce the inflammatory response to the procedure.