Surgical treatment of glaucoma is most often performed in case of ineffectiveness of conservative therapy, as well as against the background of progressive vision loss and deterioration of the optic nerve. If the operation is not performed in time, you can lose your vision.
Specialists in the field of glaucoma treatment know that there are cases when it is impossible to help patients without surgery. In modern practice, a large number of different techniques and types of operations are used to treat glaucoma. The main indication for surgery in patients with glaucoma is the lack of the desired effect from conservative techniques and the persistence of a high level of intraocular pressure (more than 22 mm Hg). In addition, it is necessary to perform surgical intervention in case of significant daily fluctuations in pressure inside the eye (more than 5 mm Hg), a progressive decrease in visual function and oppression of the optic nerve. If you refuse surgery in the presence of these symptoms, the patient will sooner or later completely lose his vision.
During the surgical treatment of glaucoma, the doctor mainly tries to stabilize the level of intraocular pressure, creating new pathways for the outflow of aqueous humor or stabilizing existing ones. At the same time, it is important to create optimal conditions for the functioning of optic nerve cells and eliminate the consequences of prolonged compression of its fibers by improving blood supply and cellular metabolism in this area. To determine the success of glaucoma surgery, you need to measure the level of intraocular pressure one year after it is performed. With good results, intraocular hypertension should be absent, and intraocular pressure should be firmly maintained at normal values.
Indications for surgery for glaucoma of the eye
| Indications for surgery using laser technologies | Indications for abdominal surgery |
|
|
Contraindications
There are a number of diseases of organs and systems for which surgical intervention is not recommended. It can aggravate the course of the disease and cause the development of other pathologies. The main contraindications include:
- ocular herpes;
- low immunity;
- retinal detachment;
- progressive myopathy.
It is necessary to plan surgical intervention with caution in the presence of malignant neoplasms in the body. Infectious or viral diseases also carry additional risks. It is necessary that the patient fully recover, which will be confirmed by laboratory tests. If there are no contraindications, the doctor sets a date for the procedure and gives recommendations on how to prepare for it.
How to prepare for glaucoma surgery?
In order to eliminate contraindications and perform surgery to treat glaucoma successfully, the attending physician prescribes a comprehensive diagnostic test for the patient, which includes the following:
| Techniques | What is it for? |
| Daily tonometry | Determination of intraocular pressure during the day. |
| B-scanning with a sufficient level of transparency of optical media | Ultrasound examination to identify affected ocular structures |
| Gonioscopy | Study of the structure of the angle of the anterior ocular chamber and the trabecular meshwork to determine surgical tactics. |
| Direct ophthalmoscopy | Determination of the integrity of the retina and optic nerve head. |
| Biomicroscopy | Determination of the condition of the cornea, identification of its dystrophic changes. |
| Electronic tonography | Auxiliary measurement of intraocular pressure and determination of the circulation of aqueous humor in the eye. |
| OCT | It is performed when there is insufficient transparency of the cornea or vitreous body, which makes it difficult to use other diagnostic techniques. |
| Laboratory tests of blood and urine | To determine the general condition of the patient. |
In order to exclude the presence of inflammatory and infectious processes, before surgery you need to visit the following specialists:
- ENT;
- dentist;
- therapist.
When is surgery required?
The answer to the question “to do or not to have surgery” can only be obtained after a thorough diagnosis of the disease. Examination using equipment allows you to determine the type and stage of pathology and possible complications. Increased intraocular pressure is not always a direct indication for the installation of a drainage shunt or other types of intervention in the ocular apparatus.
At the initial stage, it is recommended to treat this disease with different types of drops. Over time, they help reduce pressure, stop the process of falling visual acuity and narrowing of fields. If medication methods do not help and no positive dynamics are observed, drainage installation is prescribed.
Surgery is indicated in the following cases:
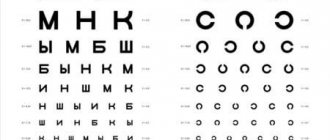
- blindness, in which a person sees only a blurred outline;
- blood pressure remains high even with regular and long-term use of drugs;
- the patient’s inability or desire to apply eye drops regularly;
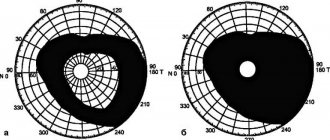
- fields of vision narrow, and the person sees only a small picture (this symptom indicates the destruction of the nerve);
- pain syndrome is present;
- deterioration of vision with normal intraocular pressure.
Attention! The modern pharmacological market offers a large number of drops that bring blood pressure back to normal. Some of them have contraindications and serious side effects that worsen the prognosis for glaucoma. Self-medication is unacceptable; pharmacological drugs can only be used with the permission of the attending physician.
Types of surgeries for the treatment of glaucoma
The price of surgery for the treatment of glaucoma depends on the method of its implementation. Modern surgical ophthalmology has a wide range of techniques to treat this disease. In accordance with the objectives of the conduct, they are divided into four groups:
| Group | Indications for use | Methods used |
| Operations aimed at providing optimal conditions for the circulation of intraocular fluid | Primary/secondary angle-closure glaucoma. |
|
| Operations aimed at creating new pathways for the outflow of intraocular fluid from the anterior chamber - fistulizing operations |
| Trabeculectomy - requires an incision of the conjunctiva, partial separation of the fibrous plate in order to create a path for the outflow of EVs into the subconjunctival space, where it can be absorbed into the vessels. |
| Non-penetrating fistulizing surgeries that do not require opening the anterior chamber |
| Non-perforating deep sclerectomy involves excision of the outer wall and ensuring the outflow of EVs into the subconjunctival space or capillaries of the ciliary body. The operation can be penetrating or non-penetrating. |
| Cyclodestructive operations |
| Cyclocryodestruction and cyclocryocoagulation, which are aimed at damage and atrophy of parts of the ciliary muscle in order to reduce the production of intraocular fluid. |
Laser iridectomy (iridotomy)
The essence of the method is to create a small duct in the peripheral zone of the iris, due to which the angle of the anterior chamber of the eye opens and the pressure in the posterior and anterior ocular chambers is equalized.
The main indications for laser iridectomy are:
- narrow- and closed-angle forms of glaucoma (both primary and secondary) with a functional block of the pupil;
- the need to prevent acute glaucomatous attacks with positive stress tests;
- irregular (flat) shape of the surface of the iris;
- iridovitreal block.
Like other ophthalmic laser procedures, laser iridotomy does not require hospitalization and is performed on an outpatient basis, under local anesthesia (Inocaine, Alcaine drops or their analogues). A special focusing device (goniolens) is placed on the cornea, which concentrates the laser beam at the required point of the iris. The aiming point can be located in any area, but usually the target is thinned areas or natural irregularities (lacunae, depressions) of the iris.
Often the duct created by the laser beam is closed again by the growing pigment tissue. In such situations, as well as in some other situations (for example, when a so-called pigment leaf remains after a microsurgical intervention), a second laser pulse is prescribed - this is enough to restore the state of the drainage system planned and achieved in the first procedure.
The accumulated clinical experience confirms the very high effectiveness of laser iridectomy: normalization of intraocular pressure can be achieved in more than 95% of cases. Rare therapeutic failures (or incomplete success) are usually due to the presence of gross organic changes in the ocular drainage structures, and thus, the timeliness of laser iridotomy and its implementation in the early stages, before the formation and proliferation of scar tissue, becomes extremely important.
The technique is also indicated and effective for prevention purposes - for example, with true narrow-angle glaucoma, the main manifestation of which is repeated acute attacks. Here one should take into account the fairly high statistical probability of an acute attack of glaucoma in the second eye, if such attacks previously developed in one eye: the risk reaches 20%, and preventive laser iridotomy is very advisable.
Laser techniques for treating glaucoma
Laser treatment of glaucoma has become widespread in ophthalmology. Techniques of this type make it possible to eliminate incisions and allow the outflow of explosives to be restored naturally. They involve the use of modern laser systems and are minimally invasive, which determines the patient’s rapid recovery after the procedure and minimal risk of complications.
Laser operations do not require opening the eyeball, and this is their huge advantage, since they minimally injure its tissues and structures. Unfortunately, their use is possible only in the early stages of the disease, since they are not able to significantly reduce the pressure of the intraocular fluid. If the disease continues to progress, repeated laser correction is not possible.
The cost of laser surgery to treat glaucoma is affordable, making it widespread. The methods used are varied, which allows for individual selection. Using a laser, the following is carried out:
- trabeculoplasty;
- iridectomy;
- descemetogoniopuncture;
- cyclocoagulation;
- combined interventions.
Rehabilitation in the early recovery period
In the first 10 days after surgery, you need to take into account important points in everyday life:
- Do not touch your eyes with your fingers or rub them, or use drops for instillation that were not prescribed by a doctor. Avoid contact of the operated eye with tap water.
- Sleeping on your stomach or on the side where the eye was operated on impairs the circulation of moisture in the eye. Therefore, it is recommended to rest on your back or the side opposite to the operated eye.
- There are no strict dietary restrictions. After surgery, you can eat if you wish. You should avoid hard and hot foods. You need to stick to a diet that does not lead to constipation. Alcohol, pickled and salty dishes are excluded from the menu.
- After surgery, it is not recommended to make sudden movements, lift heavy weights, bend down, or engage in traumatic sports. Moderate physical activity will not harm you - gentle cycling, walking. It is better to avoid visiting bathhouses and saunas. The patient should be prudent and avoid any situations that may lead to an increase in intraocular pressure.
After the operation, the ophthalmic surgeon gives recommendations to the patient. For 1.5 weeks, when going outside, the patient must wear a protective bandage over the operated eye. It can be removed at home on the third day after surgery. After surgical procedures, some patients develop a fear of light. In this case, it is recommended to wear sunglasses.
After discharge, the ophthalmic surgeon will tell you how often you need to be examined. A timely visit to an ophthalmologist will help identify complications and also adjust treatment after surgery.
Surgical techniques for treating glaucoma
Surgical treatment of glaucoma is deservedly considered effective. Just like laser, it is aimed at preserving existing vision (by reducing the pressure of the intraocular fluid). The effectiveness of the operation depends on the stage at which the patient sought treatment: it is more effective in the early stages, when there is no irreversible damage to the optic nerve. According to recent studies, the development of operated glaucoma is more favorable than non-operated glaucoma.
Since surgical techniques require opening the eyeball, the risk of injury to eye tissue is higher, and recovery after surgery to treat glaucoma is longer than after using laser techniques. The main surgical techniques are:
- operations using drainage implants;
- trabeculectomy;
- deep sclerectomy.
Before surgery
Preparation for antiglaucomatous operations is based on the same principles as the preoperative period of any intervention with opening of the eyeball.
The preoperative examination includes, in addition to ophthalmological examination, therapeutic control, the purpose of which is to exclude contraindications, underlying infections and foci of inflammation. Blood parameters are monitored without fail - the level of leukocytes, erythrocytes, ROE, platelets. Sanitation of the oral cavity is carried out.
Immediately before surgery, medication support may be required: antihypertensive drugs, as well as sleeping pills and sedatives. It is important to ensure proper rest and relieve the patient’s psycho-emotional stress on the eve of surgery.
If an ophthalmological examination reveals the presence of inflammatory diseases of the conjunctiva or eyelids, instillation of broad-spectrum antibiotics is prescribed.
Postoperative period
The recovery time after surgery depends on how it was performed. As already mentioned, laser techniques are more gentle, and therefore the recovery period is shorter. In any case, after surgery it is necessary:
- stay in bed for one or two days;
- follow your doctor’s recommendations regarding the use of anti-inflammatory and antibacterial drops;
- wear bandages;
- limit fluid intake to one liter per day;
- take measures to prevent constipation;
- eliminate the consumption of alcoholic beverages, strong coffee and tea;
- Avoid prolonged exposure to poor lighting conditions.
Advantages of glaucoma treatment at the Sfera clinic
Specialists at Professor Eskina’s clinic have been studying, diagnosing and treating visual impairments in adults and children for more than twenty years. Therefore, by contacting us, you are in the safe hands of experienced ophthalmologists who have been certified and work in accordance with international standards.
We have a wide range of diagnostic equipment and modern laser systems for glaucoma treatment. The selection of the surgical technique is carried out individually, based on the patient’s indications. You can find out the cost of surgery for the treatment of glaucoma in the corresponding section of our official website or by calling us by phone.