Dacryocystitis is an inflammation that spreads to the lacrimal sac. The pathology is more typical for babies in the first year of life, although it occurs in older children and adults. In women, the disease is diagnosed 6-7 times more often than in men.
When inflammation develops, the lacrimal sac, like the tear itself, cannot function normally. Due to impaired outflow, the fluid stagnates, infection occurs and pathology develops.
To avoid the development of an anomaly, it is important to know the reasons for its occurrence. It should also be remembered that only timely consultation with a doctor with such a pathology will help to avoid complications.
What you need to know about dacryocystitis
With dacryocystitis, an inflammatory process of an infectious nature develops in the lacrimal gland. This disease can be congenital or acquired, and have an acute or chronic course. More often, such inflammation is associated with blockage or narrowing of the nasolacrimal duct. In this case, the outflow of tear fluid is disrupted, which contributes to the unhindered proliferation of various painful microflora with subsequent inflammation of the mucous membrane of the “tear reservoir”.
Most often, dacryocystitis occurs on the left. This is due to the fact that the left nasolacrimal canal and lacrimal fossa are located at a smaller angle. The organs of the lacrimal drainage system are prone to inflammation due to the peculiarities of their location: their mucous membrane borders on the mucous membrane of the nose and conjunctiva of the eye.
Since the organs adjacent to the lacrimal apparatus (nose, eye) are rich in various microflora, any stagnation in the outflow of tears simply causes dacryocystitis.
Who most often experiences inflammation of the lacrimal sacs? The peak of this disease is typical for infancy and people 60-70 years old. In addition, it is known about some anatomical features that contribute to the disease dacryocystitis. It has been proven, for example, that people with a round (brachycephalic) skull shape and a flat nose are more likely to suffer from dacryocystitis. Such people have a number of structural features of the nasolacrimal duct and fossa that contribute to the appearance of inflammation in them.
If in newborns the appearance of dacryocystitis is not associated with any gender, then dacryocystitis in adults more often occurs in women.
Pathogenesis
The triggering mechanism for dacryocystitis is stenosis (narrowing) of the nasolacrimal duct, as a result of which the outflow of fluid decreases or becomes impossible. Next, tears accumulate in the bag, stagnate and attach pathogenic microflora, which provokes an inflammatory process.
In newborns, the pathology has a similar development mechanism and occurs against the background of a congenital anomaly of the nasolacrimal apparatus. Normally, the plug from the lacrimal sac comes off with the baby's first breath. During intrauterine development, the canal is closed with a film that protects it from the penetration of amniotic fluid.
This does not happen if the plug is too dense. As a result, the tear does not exit into the nasal cavity, but accumulates in the bag. Infection is possible both from the outside and during the passage of the fetus through the mother’s birth canal.
Symptoms of dacryocystitis
When can you suspect dacryocystitis in a person? Most often, a patient with acute dacryocystitis will experience manifestations in the form of:
- constant lacrimation;
- swelling of the ocular conjunctiva;
- pain in the orbit of the eye (often radiating to the teeth or nose);
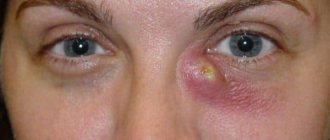
- swelling in the area of the inner corner of the eye (lacrimal sac);
- the appearance of discharge (mucus or mucus with pus) when pressing on the area of the lacrimal fossa.
Often, during the acute course of this disease, the lacrimal sac becomes very inflamed and red, and the palpebral fissure closes completely. In this case, the temperature may rise and general malaise may appear (poor appetite, weakness, headache, etc.)
Sometimes dacryocystitis provokes the appearance of conjunctivitis.
The appearance of the eye with dacryocystitis changes in the subsequent days of the disease. A dense, painful swelling in the corner of the eye softens after a few days, and the redness disappears. Usually, after this, an abscess (suppuration) is formed, which opens up on its own. The accumulated pus comes out and the inflammation disappears. However, sometimes the process of inflammation of the lacrimal sac ends with the formation of a fistula, through which the purulent contents of the nasolacrimal canal drain.
In chronic cases, dacryocystitis can manifest itself as:
- persistent and profuse lacrimation;
- severe swelling of the orbit of the eye (more pronounced in the morning);
- the appearance of a tumor in the area of the lacrimal sac;
- the appearance of contents (purulent or mucous) when pressing on the lacrimal openings;
- redness and swelling in the area of the inner eyelid;
- manifestations (not always) of visual impairment (especially peripheral) due to inflammation of the cornea.
Dacryocystitis often takes on a recurrent course and then the disease occurs frequently, several times a year.
When to see a doctor
Dacryocystitis in adults, whose treatment in the early stages is often delayed due to mild symptoms, can lead to the spread of infection to surrounding tissues.
Therefore, you should seek medical help if:
- painful swelling between the inner corner of the eye and the nose;
- regular lacrimation;
- purulent and serous discharge from the corner of the eye when pressed;
- elevated body temperature and general symptoms of intoxication.
Dacryocystitis is treated by an ophthalmologist. Depending on the symptoms and complexity of the disease, additional consultation may be required: a maxillofacial surgeon, neurosurgeon, traumatologist, otolaryngologist, dentist, neurologist.
Dacryocystitis in children
Dacryocystitis is very common in children, being congenital or acquired. Most often, dacryocystitis in children is located on one side, and only in 3% of cases the process can be bilateral.
The symptoms of acute dacryocystitis in children differ little from the manifestations of this disease in adults. The disease in children occurs with the same symptoms of redness and swelling of the eyelid with enlargement and soreness of the lacrimal sac.
However, in children with dacryocystitis, the swelling of the eyelids is often very severe, involving the upper and lower eyelids. Sometimes the baby cannot even open his eyes due to severe inflammation. Children often experience a fever and a deterioration in their general health (fever, chills, refusal to eat, tearfulness).
Often in children, inflammation of the lacrimal sac spreads in the form of swelling to the eye orbit, cheek or nose.
After a few days, the inflammatory focus in the lacrimal sac turns yellow and softens. This indicates the formation of an abscess, which often opens on its own.
Dacryocystitis in newborns often occurs with minimal symptoms. In this case, the temperature in babies often remains normal, and an abscess does not develop.
Often, blockage of the nasolacrimal duct and inflammation of the lacrimal sac in an infant looks like a sour eye. The eye becomes especially sour after a night's sleep. Also, with this disease, the baby’s eyes become cloudy.
When you press lightly on the lacrimal sac, mucus or pus often comes out.
And although dacryocystitis in newborns is not contagious, this diagnosis requires mandatory consultation with an ophthalmologist.
Causes
Dacryocystitis usually appears if, for some reason, tear stagnation occurs, which promotes the proliferation of microflora in the “tear reservoirs” (canals or sac). At the same time, microbes (staphylococcus, streptococcus, meningococcus, chlamydia, etc.) begin to multiply in the eye sac.
Inflammation of the lacrimal sac can occur for many reasons. Thus, in newborns, dacryocystitis can occur due to certain congenital disorders:
- narrowing or complete occlusion of the nasolacrimal duct;
- gelatinous plug that did not resolve in time;
- the presence of a membrane inside the nasolacrimal duct.
Also in children, dacryocystitis can be acquired for the following reasons:
- dust or foreign matter entering the nasolacrimal canal;
- inflammation of the eyes or nose (inflammation of the sinuses, purulent conjunctivitis, etc.);
- eye injuries.
In adults, inflammation of the lacrimal sac can occur in the following cases:
- swelling in diseases of the nasopharynx (rhinitis, sinusitis, polyposis, etc.);
- eye diseases (purulent or viral);
- injuries to the eyes, nose or nasolacrimal duct (injuries to the eyelids, fractures of the nose, damage to the nasolacrimal duct);
- getting foreign objects into the eyes (dust, dirt, sand).
The lacrimal sac becomes inflamed especially often if the patient’s body is weakened due to:
- allergic manifestations in the eye or nose area (rhinitis, conjunctivitis);
- metabolic disorders (diabetes mellitus, etc.);
- weakened immunity (after long-term illness or stress);
- sudden temperature changes;
- occupational hazards (dust, chemical compounds, etc.)
Classification
There are two forms of dacryocystitis:
| Form | Characteristics |
| Spicy | It manifests itself as an independent disease or exacerbation of a chronic form of inflammation of the lacrimal sac. Accompanied by severe symptoms and purulent discharge. |
| Chronic | Develops against the background of infectious pathologies in neighboring anatomical structures (sinuses, nose). Against this background, a narrowing of the nasolacrimal duct occurs, followed by infection and the development of inflammation. Has a wavy current. |
Dacryocystitis of newborns is separately distinguished. It develops with congenital anomalies of the nasolacrimal apparatus and occurs in approximately 7% of babies.
Note! The presence of such an anomaly does not guarantee the development of pathology, but only increases the risk of its occurrence when the baby’s body is exposed to unfavorable factors.
Depending on the cause of inflammation of the lacrimal sac, the following forms of the disease are distinguished:
- post-traumatic dacryocystitis (after mechanical damage to the facial skull);
- viral;
- bacterial;
- parasitic;
- mycotic (fungal);
- chlamydial (caused by chlamydia).
Diagnostics
Typically, the diagnosis of dacryocystitis is not difficult. However, sometimes it is necessary to distinguish dacryocystitis from another inflammatory eye disease - conjunctivitis. With conjunctivitis, the eyes also turn red, and symptoms are associated with swelling, burning or itching, and slight discharge from the eyes.
Dacryocystitis occurs without general redness of the eye, but with severe lacrimation.
The main distinguishing symptom of dacryocystitis is the release of pus or mucus when pressing on the area of the lacrimal sac.
Often, the Vesta color test or tubular test is used to detect dacryocystitis. In this case, collargol is instilled into the eye, and a tampon is inserted into the nasal entrance. By the release of the dye from the lacrimal ducts, one can judge the degree of patency of the lacrimal canal. If 10 minutes after the injection of Collargol there are no traces of dye on the tampon, it means that the lacrimal ducts are impassable.
Also, when diagnosing dacryocystitis, the following methods are used:
- diagnostic probing of the lacrimal canals;
- eye biomicroscopy;
- fluorescein instillation test;
- contrast radiography of the lacrimal ducts;
- bacteriological culture to clarify the nature of the microflora.
In infants and newborns, dacryocystitis is usually diagnosed according to a simplified scheme, including examination by an ophthalmologist and bacteriological culture of the contents of the lacrimal sac.
Treatment
Very often, doctors offer inpatient treatment for dacryocystitis to adults and children. Treatment methods before and after softening of the infiltrate are different.
Before the infiltrate matures, therapeutic methods are often used in the form of:
- Physiotherapy to accelerate the maturation of the abscess (UHF therapy, dry heat in the lacrimal sac area).
- Vitamin therapy.
- Opening a mature abscess.
After opening the infiltrate, therapeutic measures include:
- Draining the wound with rinsing with antiseptic solutions (furatsilin solution, hydrogen peroxide or dioxidine).
- Using broad-spectrum antibiotics orally or by injection for 7-10 days (usually penicillins or aminoglycosides), often in combination with sulfonamide drugs.
- Local use of antibiotics in the form of ointments (tetracycline, erythromycin, etc.) and instillation of antibacterial drops (miramistin, gentamicin, sodium sulfacyl, cypromed, etc.)
- In pediatric practice, eye drops with antibiotics (Tobrex, Vigamox, Vitabact, Albucid) are used for treatment.
- In case of severe intoxication (more often in children), detoxification solutions are used intravenously (in the form of calcium chloride, glucose, gemodez with ascorbic acid, hexamethylenetetramine).
- Surgical treatment of dacryocystitis is possible after relief of acute inflammation (dacryocystorhinostomy). In this case, the cavity of the lacrimal sac is drained surgically. This method is used mainly in adult patients who suffer from repeated inflammation of the lacrimal sac with constant relapses. Occasionally, the method is also used in pediatric practice (for chronic forms of dacryocystitis), requiring “jewelry” technology from surgeons to preserve full vision for the child. The operation is not performed in acute forms of the disease or in cases of exacerbation with purulent discharge from the lacrimal sac. Rehabilitation after surgery lasts about a month and includes local use of rinsing and instillation with antiseptic solutions.
- Use of modern methods of laser and endoscopic dacryocystorhinostomy as surgical treatment. This low-traumatic surgical technique allows you to do without a visible postoperative scar. According to indications, a similar method of surgical treatment is used for children or newborns. In this case, instead of a scalpel, a laser mounted in an endoscope is used.
Compared with traditional surgery, the laser endoscopic method allows you to do without hospital treatment, general anesthesia and postoperative bleeding. However, this type of intervention is more expensive and is not indicated for all patients.
With dacryocystitis, patients are prohibited from using many activities related to contact with the cornea (using contact lenses, applying bandages, ultrasound methods, tonometry, etc.). Such methods can lead to the formation of purulent ulcers of the cornea.
Treatment of dacryocystitis in newborns
With dacryocystitis in newborns, they generally try to do without hospitalization. Most often, inflammation of the lacrimal sac occurs in a milder form and is associated with the physiological characteristics of the body. Typically, treatment of dacryocystitis in infants is carried out using the following methods:
Massage for dacryocystitis
Massage the lacrimal sac for 2-3 weeks. This therapeutic method is effective in the first months of a child’s life in 90% of cases. In this case, the index fingers are used for massage. Anyone can learn massage. First, the mother needs to wash and disinfect her hands, and cut her nails short, removing the varnish from them.
The massage technique for dacryocystitis in newborns consists of:
- Light tapping movements with the index finger in the area of the lacrimal sacs (it is better to do it simultaneously in both eyes).
- Run your finger with light pressure from the corner of the eye to the bridge of the nose (10-15 times). It is important to move from top to bottom to clear the tubules of their contents. You cannot change the direction of movement. Often, secretions may come out of the corners of the eyes, which indicates the effectiveness of the massage. It is better to remove droplets of secretion with sterile cotton swabs soaked in a solution of furatsilin or a decoction of medicinal herbs (chamomile, calendula).
- The session ends with light vibration of the lacrimal glands area.
- Massage is usually done 3-4 times a day, often before feeding. At the end of the session, doctors often recommend dripping a solution of furatsilin (1:5000) or miramistin (0.01%) into the baby’s eyes. If massage for dacryocystitis is not enough, doctors prescribe other methods of treatment (washing and probing of the tubules).
Massage should not be performed at the slightest suspicion of purulent inflammation. Otherwise, this may result in the spread of infection and the development of a dangerous complication - phlegmon.
Washing
Rinsing and parallel probing (or bougienage) of the nasolacrimal canal. Performed if other methods are ineffective. Probing and bougienage are performed through the lacrimal openings of the nasolacrimal canal and are a gentle substitute for surgical treatment. Manipulations are usually performed under local anesthesia and last several minutes. At the same time, the shape of the probe in the form of a cone expands the channel and cleans it. Such manipulations are painless for children, but may be unpleasant for them. The procedure is completed by inserting a long probe and using antiseptic solutions. After probing, the Vesta color test is used to determine the degree of patency of the canal. Repeated probing or bougienage is often required at intervals of several days.
Be sure to visit a doctor for outpatient treatment of dacryocystitis at least 2 times a week. After 2 weeks of treatment, the doctor will determine the effectiveness of the conservative treatment.
Operation
Surgical treatment is rarely used in newborns. If surgery is unavoidable, preference is given to minimally invasive methods (laser method). Traditional surgery is performed under general anesthesia. Before surgery, mandatory antibiotic therapy is carried out to prevent postoperative complications.
A rare but very dangerous complication of surgery in newborns is a brain abscess due to infection from the eye sac with venous blood into the brain.
Eye massage for dacryocystitis
Mechanical impact is used mainly in children, as it allows you to separate the embryonic plug and speed up its release. Massage should be done daily. In the area where the lacrimal sac is located, moderate jerking movements are performed from top to bottom. 2-3 pushes are done at one time. It is recommended to perform approximately 10 such movements for each procedure.
The duration of using massage for the treatment of dacryocystitis is 1-2 weeks. If there is no result, resort to other methods of therapy.
Complications of dacryocystitis
Dacryocystitis usually occurs without serious complications. However, in some cases, the disease can contribute to the development of complications in the form of:
- tear duct stones;
- orbital phlegmon;
- lacrimal sac abscess;
- brain abscess;
- sepsis.
With advanced systemic diseases in weakened patients, dacryocystitis can give rise to the emergence of serious pathologies in the body. And complications such as brain abscess or sepsis can lead to death.
Although dacryocystitis is a well-studied and treatable ailment, it is absolutely impossible to neglect this disease. Particular attention should be paid to inflammation of the lacrimal sac in children or weakened people. Dacryocystitis can not only become chronic and significantly worsen the patient’s quality of life, but also cause various serious health complications. Take care of your eyes!
Sources used:
- Avetisov S. E., Egorov E. A., Moshetova L. K., Neroev V. V., Takhchidi H. P. Ophthalmology: national manual // M.: GEOTAR-Media. — 2008.
- Brzhesky V.V., Somov E.E. Corneal-conjunctival xerosis (diagnosis, clinic, treatment) / 2nd ed., revised. and additional // St. Petersburg: Lefty. Saint Petersburg. — 2003.
- Diseases of the lacrimal organs: Monograph / Cherkunov B. F. - Samara: State Enterprise "Perspective", 2001.
- Kursk State Medical University