Marcus-Gunn syndrome is a disease of the visual apparatus, which is manifested by blepharoptosis of the upper eyelid in combination with its uncontrolled lifting. In this material we will talk in detail about this disease and find out what symptoms it has and whether it can be treated.
Marcus-Gunn syndrome is a fairly rare disease, most often it is congenital. The incidence does not depend on gender, since both men and women are equally susceptible to this disease.
Causes
According to statistics, pathology occurs in only 5% of the population. It is usually observed in children and occurs with equal frequency in both sexes. Gunn syndrome often develops accidentally. Very rarely, the causes of the disease lie in a genetic predisposition, and it is inherited according to an autosomal dominant pattern of inheritance.
The main causes of the disease are underdevelopment of the elevator muscles responsible for raising the eyelid and a defect in the nerve that controls these muscles. Most often, the disease develops during the period of intrauterine development of the fetus due to a genetic failure or birth trauma.
The acquired form of the pathological process occurs due to the following reasons:
- inflammation of the brain;
- weakening of the elevator muscles as a result of aging of the body;
- chronic cerebrovascular insufficiency;
- damage to the 7th cranial nerve;
- multiple sclerosis;
- change in connections between the 3,5,7 pairs of cranial nerves.
Surgical interventions during which the facial nerve is damaged are less likely to provoke the development of pathology; tooth extraction associated with a gum incision, Botox injections or other cosmetic procedures performed invasively.
Pathogenesis
Different etiologies of apallic syndrome cause different morphological patterns of cortical damage. There are no specific disorders inherent in the disease. If the cortex is insufficiently saturated with oxygen, necrosis occurs. Traumatic injuries disrupt the anatomical and functional connections between neurons. Degenerative changes cause progressive atrophy and decreased functionality of the cortex.
If a person is in a coma, not only consciousness is absent, but also vegetative functions. The transition from coma to normal life begins with the restoration of subcortical structures, the reticular formation. During this period, the cortex is still inactive, and until neural connections are formed, the patient will be in a state of apallic syndrome.
Symptoms
The following symptoms are characteristic of apallic syndrome:
- outwardly the patient is conscious, but is not aware of himself, does not recognize objects and people, does not respond to stimuli;
- pain sensitivity, ability to chew and swallow are preserved, but at a slower pace;
- the body maintains breathing, heartbeat and blood pressure due to the preserved function of the hypothalamus;
- the function of the pelvic organs is not controlled by the patient;
- The alternation of sleep and wakefulness is maintained, but the daily cycle is irregular.
While awake, the patient opens his eyes, reacts to painful stimuli, but does not show other signs of consciousness, emotions, or purposeful activity. The patient may develop excessive tension in the sympathetic nervous system, manifested by increased blood pressure, rapid pulse, and pain in the heart. The symptom of restless legs manifests itself in the form of cramps, numbness, crawling, and tingling in the lower extremities.
The face does not express emotions, there is no facial expression, the eyes are not capable of tracking, they move chaotically. Painful stimulation is accompanied by dilated pupils, increased blood pressure, and increased heart rate. The patient is characterized by spastic compression of the hands and feet, bent position of the legs, and tonic short-term convulsions.
In a state of sleep, the patient experiences an increase in the tone of the parasympathetic system - blood pressure decreases, the pulse becomes less frequent, the face turns red, and sweating increases.
In case of injuries, metabolic disorders, poisoning, hypoxia, apallic syndrome develops in a short time. Degenerative processes are characterized by a gradual loss of brain function. The first sign of restoration of consciousness is the appearance of gaze tracking of moving objects. With the acute development of the disease, consciousness can be restored completely.
Symptoms
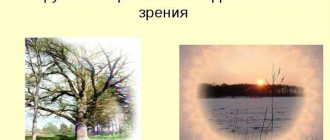
If the disease is congenital, then Marcus Gunn syndrome is detected in early childhood. The child may notice drooping of the upper eyelid. However, when opening the mouth, moving the lower jaw to the side or down, or clenching the teeth, the affected eye opens. This process occurs reflexively and the person does not control it. In infants, this symptom can be noticed while the baby is suckling. Drooping of the eyelid or ptosis can be subtle or very noticeable, as well as the degree to which the affected eyelid is dependent on mouth movements.
In children, symptoms include lacrimation, swelling of the eyelid and general weakness. With age, clinical signs disappear due to the development of skills by sick people that help mask symptoms. Mostly, the pathology affects one eye, but there are also cases of bilateral damage.
According to the severity of Gunn's syndrome, there are:
- Full. The pupil is completely covered by the eyelid and is not visible.
- Incomplete. The pupil is 2/3 closed.
- Partial. The eyelid slightly covers the pupil.
International Neurological Journal 6 (36) 2010
The syndrome was described in 1883 by London ophthalmologist Marcus Gunn in a 15-year-old girl and bears his name [7].
Synkinetic Marcus Gunn syndrome involves ptosis of the upper eyelid, which is combined with involuntary raising of the ptotic eyelid with movements of the lower jaw. Synkinesia appears when opening the mouth, moving the lower jaw in the direction opposite to ptosis (in isolated cases - in the same direction), pushing the jaw forward, clenching the teeth, and moving the lips. The severity of ptosis and synkinesis varies widely. Marcus Gunn syndrome in 50–60% of cases is combined with strabismus, as well as amblyopia, which is most often caused by strabismus and only in some cases by ptosis [5, 7].
A combination of palpebromandibular synkinesis of Hun with Waardenburg and Hirschsprung syndromes has been described [8].
Marcus Gunn syndrome is usually unilateral, in rare cases it occurs on both sides [4, 7].
Marcus Gunn syndrome is considered a rare anomaly. According to foreign authors [5], it occurs in 5% of people with congenital blepharoptosis. According to domestic ophthalmologists [3], a practicing doctor encounters this pathology 1–3 times a year. It is observed equally often in men and women.
Pathological synkinesis is most often detected in early infancy; When feeding from a bottle or breastfeeding, the mother notices unusual rhythmic movements of the upper eyelid.
We observed three patients with Marcus Gunn syndrome. In all cases there was a classic variant: congenital synkinesia, unilateral symptoms described above, but in none of them the diagnosis was made before contacting the State Institution “IPAG AMNU”.
Here is our observation.
Child T., 3 months. 11 days, boy. Complaints about drooping of the upper eyelid of the right eye. According to the mother, at birth the right eye was closed and swelling of the eyelids was noted. When the swelling subsided and the eye began to open, the mother noticed that there was a rhythmic up and down movement of the right upper eyelid while breastfeeding.
The child was examined by a neurologist. At the age of 1 month. 1 week spent a week in the neurological department of the city clinical hospital, where an NSG was performed, which did not reveal any pathology, as well as X-ray and MRI of the chest organs. Discharged with a diagnosis of myasthenia gravis. Timoma?" Hormonal therapy is recommended - prednisolone.
A child from the first pregnancy, at the end of which swelling of the right ankle joint was noted. During labor, labor was weak, there was a long anhydrous period of 10 hours, and there was a short umbilical cord. Birth weight - 3750 g, length - 56 cm, head circumference - 35 cm, Apgar score - 7-8 points. He screamed right away. Discharged on the third day.
An objective examination in our clinic showed that the child’s general condition was satisfactory. Development corresponds to age: follows the object, holds the head, the support reaction is positive, there are stepping movements.
On the right there is partial ptosis. When breastfeeding, the right upper eyelid rises and falls rhythmically. On the left is a weakly positive Graefe sign. Sucks actively. Muscle tone is satisfactory. Reflexes on the upper and lower extremities are of moderate vivacity without asymmetry. Babinski's sign on both sides. Robinson, Moreau, Perez, Bauer's symptoms are positive. There were no signs of myasthenia gravis.
He was examined by an ophthalmologist and diagnosed with “congenital ptosis of the upper eyelid of the right eye.”
Due to suspected thymoma, the child was in the surgical department of our institute for 10 days. An ultrasound scan and repeated radiography of the chest organs were performed, which revealed slight positive dynamics; Ultrasound shows thymic hyperplasia.
The child was discharged with a diagnosis of thymic hyperplasia. Timoma? Marcus Gunn syndrome." A course of hormonal therapy is recommended. Thus, the child had a typical picture of Marcus Gunn synkinesis, which was not recognized during the initial examination by either a neurologist or an ophthalmologist.
The second child, a 1.5-year-old girl, lived in Moscow, came to Kyiv to visit relatives, was examined at our clinic, and was diagnosed with Marcus Gunn syndrome. Subsequently, she periodically consulted at our institute, the last examination was at the age of 10: ptosis and synkinesis are not clearly expressed, they represent a mild cosmetic defect, to which the child is fully adapted.
The third child was diagnosed at 3 months. during a preventive examination in our clinic.
Hun syndrome is most often congenital, but can be acquired. Its development has been described against the background of progressive cerebral vascular insufficiency, as well as after mental trauma [2].
Gunn syndrome is almost always sporadic, but familial cases with an irregular autosomal dominant pattern of inheritance have been reported [6].
The etiology and pathogenesis of palpebromandibular synkinesis of Marcus Gunn are the subject of debate. Some authors explain synkinesis by pathological connections between cranial nerves (III, V, VII pairs) [1, 9]. Others believe that the pathological focus is localized supranuclear. It is believed that the basis of Marcus Hun syndrome is the restoration of phylogenetic ancient branchial-oral synkinesis, since the muscles of the eyelid develop from the muscles that move the gill operculum. In fish, the respiratory and feeding mechanisms are combined - along with the opening of the mouth, the gill covers rise.
Many researchers consider pathological synkinesis as a result of the predominance of subcortical structures, and the morphological basis of pathological synkinesis is a congenital or acquired defect of the pyramidal system [2], the hidden insufficiency of which can manifest itself under the influence of external factors.
The prognosis for Marcus Gunn syndrome is favorable. Older people often state that palpebromandibular synkinesis decreases over time. However, this has not been confirmed by objective research data. It is likely that older people pay less attention to synkinesis or have learned to mask them [5]. However, with severe ptosis and synkinesias, when they are combined with strabismus and amblyopia, surgical treatment is indicated.
Thus, Marcus Gunn syndrome is a clearly defined clinically pathological synkinesis that occurs more often than is diagnosed. It is useful, first of all, for neurologists and ophthalmologists to remember this in order to avoid diagnostic errors, as well as to give qualified recommendations to parents. Currently, effective methods for surgical correction of this pathology have been developed.
Diagnostics
To establish a diagnosis, the doctor examines the patient and asks him (if the pathology is acquired and the patient is an adult) or his parents (in the case of a congenital pathology in a child) about the heredity factor. Then the mobility of the eyelid and its dependence on the activity of the jaw are assessed, the width of the palpebral fissure and the location of the mobility of the eyelid are determined.
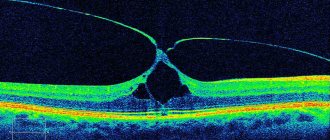
Visual acuity (visometry) is checked. Vision does not deteriorate with Gunn syndrome. Biomicroscopy is performed using a slit lamp to assess the condition of the cornea, conjunctiva, and eyelids. Using biomicroscopy, swelling and redness of the conjunctiva are detected.
If the origin of the disease is traumatic, an x-ray examination is prescribed. If the disease has developed due to damage to the central nervous system, consultation with a neurologist and an MRI are necessary. Radiography is used in the acquired form of the disease to identify the root cause of the disease. MRI helps to identify the relationship between nerves that have become pathological.
Read in a separate article: Conjunctival cyst of the eye: retention, dermoid, treatment and drops
Complications
Complications of apallic syndrome are associated with loss of consciousness and prolonged immobile position of the patient:
- forced position of the limbs due to prolonged spasm leads to joint contracture;
- lack of physical activity and constant stay in bed leads to the formation of bedsores, stagnation of blood in the pulmonary circulation, causing pneumonia;
- the spread of infection along the urinary tract can cause pyelonephritis; infection in the blood leads to sepsis with possible death.
Complete loss of brain function leads to the death of the patient. Life expectancy can be increased with the help of comprehensive care, therapy, and adequate nutrition for the patient.
Treatment of Marcus Gunn syndrome
The main treatment for Marcus Gunn syndrome is surgery, which is performed under general anesthesia. It is not recommended for children under 5 years of age or with mild illness. However, when the visual axis is completely covered by the eyelid, surgical intervention is mandatory.
Surgery is recommended in the presence of severe ptosis, which interferes with normal life, and also if the disease is accompanied by strabismus and amblyopia. In uncomplicated pathology, surgery is prescribed after the teenager reaches 15 years of age to eliminate a cosmetic defect.
Operations are divided into several groups:
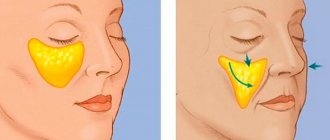
- According to Blaškowicz. The levator fold is formed.
- Hess. Performed in case of dysfunction of the levator and superior rectus muscles. The eyelid is tightened using sutures that extend slightly above the eyebrows through the frontal muscles.
- Operation Mote. Blepharoptosis is corrected by enhancing the functioning of the levator muscle if the levator is paralyzed.
- Tarzomyectomy. This is the removal of part of the eyelid of the affected eye and its further strengthening with a special graft. Tarzomyoectomy is recommended if minimal clinical symptoms are present and the functional ability of the levator muscles of the upper eyelid is preserved.
The operation does not completely eliminate Hun's syndrome. But treatment significantly reduces the risk of developing complications of ophthalmological pathology, such as strabismus, decreased vision clarity, amblyopia.
Non-surgical treatment
If the eyelid gap is 3 centimeters or less, the patient is taught to regulate the lowering of the eyelid using the masticatory muscles. Initially, for this purpose, the eyelid is fixed with a plaster, which the person wears all day, and removes during sleep. Conservative therapy is carried out for a false form of the disease or when neurogenic factors become the main causes of development. Physiotherapeutic procedures are carried out, such as: paraffin therapy, UHF, galvanization.
Self-massage and gymnastics are prescribed to enhance muscle activity in the upper part of the face.
To perform gymnastics, it is recommended to do the following:
- roll your eyes in a circle for a minute;
- move your gaze to your nose, straining your eyes for 15 seconds, and then relaxing them (perform 6 times);
- close your eyelids and forcefully hold them in this position for 5 seconds. Then open your eyes as wide as possible. Repeat the exercise 6 times;
- Use your fingers to pull the skin in the temple area so that your eyes open wide and blink frequently for at least 30 seconds.
Drugs
Drug treatment involves the use of medications after surgery. It is not possible to get rid of Hun syndrome with their help and is unlikely to ever become so.
These pharmacological agents are always prescribed personally by the doctor immediately after the operation. In such cases, antiseptics, antibiotics and eye ointments are prescribed. The first is most often a zinc solution with a concentration of 0.25 percent, mixed with a two percent solution of boric acid. Used for washing. As for the second, the use of drops of a 0.25 percent solution of chloramphenicol or 0.3 percent ofloxacin is recommended. The ointments most often used are one percent ethromecin and tetracycline.
Prognosis and prevention
The prognosis for Gunn syndrome is quite favorable if the disease is detected and treated in time.
No special measures have been developed to prevent the disease. Preventive measures include ensuring safety at work (eye protection with a mask or goggles). All people with Marcus Gunn syndrome should undergo preventive examinations by an ophthalmologist twice a year.
Hun syndrome causes not only aesthetic discomfort, but can provoke the development of strabismus and “lazy eye” syndrome. Therefore, ophthalmological pathology must be treated for further normal human life.
Author of the article: Bakhareva Elena Sergeevna, specialist for the website glazalik.ru Share your experience and opinion in the comments.
Diagnostic measures
To accurately establish the diagnosis, the doctor performs a variety of procedures.
First of all, the ophthalmologist talks with the patient to exclude or confirm the hereditary factor of the disease. Then a visual examination of the patient is carried out, during which the doctor evaluates the mobility of the eye and eyebrows, the placement of the movable eyelid, and the width of the eye opening. Then visual acuity is examined and biomicroscopy is performed using a slit lamp, which allows you to evaluate the structure of the eye. Thus, the doctor checks the condition of the upper and lower eyelids, the conjunctival cavity and the cornea.
If the pathology appears as a result of injury, then an x-ray is taken. Magnetic resonance imaging is needed if the disease arises as a result of damage to the central nervous system. In addition, it is necessary to consult a neurologist.