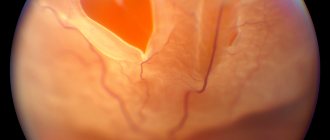
After 45 years, dystrophic changes begin to occur in a person’s eyes, causing disturbances in central and peripheral vision. One of the most common age-related problems is a macular hole of the retina, a defect in the central part of the retina (macula) that causes problems with visibility. This disease is especially common in older women suffering from myopia. In advanced cases, complete loss of vision is possible.
What it is?
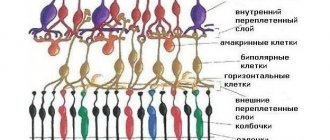
The retina (retina) is a thin tissue that continuously transforms the energy of light pulses and transmits it to the brain. It is thanks to this shell that the perception of the surrounding world is ensured. One of the most important parts of the retina is the macula - the macula, consisting of many optic nerves with dimensions of only a couple of millimeters. As light passes through the lens, information about the visible image is transmitted along nerve fibers to the brain. Despite the fact that the retina is tightly attached to the vitreous body, under the influence of a number of factors, a rupture of the membrane can occur, subsequently causing its detachment.
In ophthalmology, a macular hole is a rounded defect in the neurosensory part of the retina in the foveal zone, characterized by the appearance of a vertical traction component. Such a violation of the integrity of the tissue in the center of the retina leads to irreversible changes, including complete loss of vision.
Clinical picture of the pathology
The inside of the eyes is filled with a gel-like substance called vitreous humor. It occupies 75% of the volume of the organ of vision. Physically, it is located in the space between the lens and the retina. The vitreous body is tightly adjacent to the mesh tissue throughout its entire length.
However, the strongest area of their connection is the center of the retina or its macula. It consists of a huge number of receptors that recognize light and color, the so-called “cones” and “rods”. This part of the eye is responsible for human object vision.
Over the years, the vitreous body changes dystrophically and involutionally. It becomes more liquid and partially moves away from the retina.
But it continues to fit tightly to it in the macula. At the same time, the vitreous constantly acts on it mechanically. As a result, this leads to a tear in the retinal macula.
Causes
The causes of a macular hole in the retina are very diverse. Most often, the visual defect is age-related. As a person ages, the vitreous body softens and undergoes involutional changes. The space inside the eyeball, filled with vitreous humor, decreases in volume for a number of reasons. As a result, its jelly-like structure becomes more and more liquid, which leads to detachment of the vitreous body.
As a result, a constant force of mechanical tension acts on the macular area, which subsequently causes its separation and the formation of a macular hole. Gradually, the defect becomes larger and begins to pose a serious threat to vision. In addition to age-related changes, the causes of macular hole can be the following:
- eye injury;
- epiretinal fibrosis;
- vitreomacular traction syndrome;
- high myopia;
- chronic inflammatory process;
- retinal disinsertion.
The following factors can also cause retinal rupture:
- severe stressful situations;
- head injuries;
- active physical activity;
- a sharp bend or jump.
Most often, the nature of the origin of the pathological process remains unknown. In this case, the disease is idiopathic or spontaneous.
Often in this case, retinal rupture is accompanied by other eye pathologies.
After passing:
Operation of epiretinal gliosis:
Typically, the film can be completely removed during surgery. However, the retinal tension from removing the film will only be restored after several weeks or even months. In some cases, maintenance therapy with cortisone injections near the eyeball is justified. These manipulations are carried out on an outpatient basis with pain-relieving drops.
Macular retinal hole surgery
After the gas tamponade is removed, a follow-up visit at the eye clinic will determine whether the hole has disappeared. Only in extremely rare cases does this not happen. If the hole does not disappear, you will be advised to undergo another procedure with a new tamponade or, if necessary, silicone oil. The silicone oil will not remove from the eye on its own, so another follow-up surgery will be required. The disappearance of the macular hole through surgery occurs in more than 95% of patients.
Frequently asked questions from patients about macular hole surgery
- What visual acuity can I expect after surgery? If air, a gas bubble, or silicone oil is injected into the eye during surgery, vision will be blurry immediately after surgery. The long-term success of treatment depends on the extent of the disease and various factors. If epiretinal gliosis develops without previous retinal disease, you can expect significant improvement in vision after surgery. The operation can have a positive effect on vision; deterioration occurs in extremely rare cases. For macular retinal holes, the success of treatment depends on the stage and duration of the disease. If the macular hole has recently appeared, then you can confidently expect improved vision after surgery.
- Will I feel pain during and after surgery? The operation is painless. However, as with any surgery, few patients experience minor pain when moving their eyes, which is so minor that it usually does not require an appointment.
- What complications occur most often? The most common complication of this surgery is an increased chance of clouding of the lens (i.e., cataracts). Typically, cataract surgery is not required until several years after the previous surgery. In rare cases, a temporary fluctuation in internal eye pressure occurs. In extremely rare cases, surgery can lead to retinal detachment. The situation at an early stage can be corrected with the help of outpatient laser treatment; in later stages, surgery helps. A healthy eye is always full of beneficial bacteria. If individual bacteria enter the eye during surgery, they will be destroyed by the body's own defenses. Yet in less than one case in a thousand, bacteria entering the eye can lead to serious inflammation that must be treated in hospital or sometimes with surgery. In extremely rare cases, vision loss may also occur.
Surgeries for epiretinal gliosis and macular retinal hole are common procedures for eye clinics in Germany, performed multiple times every day. The development of medical surgical technology and improved instruments make it possible to perform very reliable operations in German clinics. The surgery helps most patients significantly improve their vision. This helps to avoid vision-related problems and often significantly improves the standard of living.
If you have any further questions about epiretinal gliosis or macular retinal hole, please contact us for answers. We are happy to take the time to give you answers or discuss specific problems and give you the best advice possible.
At-risk groups
Macular retinal hole is most often observed in the following categories of people:
- elderly men and women - most often the pathology occurs at the age of 50-75 years;
- females - according to statistics, retinal tears are diagnosed much more often in women;
- people with bad heredity - if close relatives had a similar problem, then the likelihood that it will arise is quite high;
- pregnant women - during the gestation period, the impact of negative factors increases, the risk of various diseases increases;
- patients with myopia - with this disease, the eyeball lengthens, which leads to stretching and thinning of the retina, the likelihood of rupture increases;
- patients with retinal dystrophy - even minor defects in the retina can subsequently provoke its rupture.
People suffering from diabetes and high blood pressure are also at risk.
Classification
Depending on the cause of origin, the following types of macular hole are distinguished:
- traumatic - occurs in 10% of all cases, characterized by the formation of a defect in the thinnest place of the retina as a result of a shock wave passing through the eyeball;
- myopic – the most severe form of the disease, which occurs against the background of severe myopia and requires long-term treatment and rehabilitation;
- postoperative - a rare form of the disease, occurring in 1% of cases as a result of disruption of the integrity of the retina during eye surgery;
- idiopathic - the exact cause is unknown, macular rupture occurs as a result of age-related changes that provoke thinning of the retina.
According to the type of rupture, the disease is:
- incomplete (lamellar) – the macular defect is superficial;
- complete (through) - all layers of the retina are damaged.
In ophthalmology, macular degeneration occurs in two forms:
- Dry. The initial stage of the pathological process, which is diagnosed in 90% of cases. With this form of the disease, a gradual deterioration of central vision occurs, and at the same time one may not even notice it. And since it is at this stage that treatment will be most simple and effective, it is extremely important to undergo regular preventive examinations with an ophthalmologist.
- Wet. This form of the disease occurs if the pathology was not detected at the initial stage of development. As macular degeneration progresses, the formation of new blood vessels of a pathological nature occurs. Due to their excessive fragility and fragility, small yellow accumulations (drusen) form in the retina and hemorrhage occurs. Wet dystrophy develops rapidly, so treatment should be carried out as quickly as possible.
An incomplete macular hole of the retina most often occurs in one eye, but damage to both organs of vision can also occur.
What types of retinal tears exist?
The problem is divided into several types, since retinal rupture is serious or not depends on the source of the disease:
- Holey. To a greater extent, it develops in places with the most severe tissue depletion. This can cause retinal detachment.
- Valve. Usually occurs as a result of failure of proper interaction of the retina with the middle membrane of the eye. In this case, the retina breaks along the jagged lines.
- Macular. This type is the most dangerous of the above, since detachment occurs in the central area.
Important! Failure to provide timely medical care increases the chances of vision loss.
Symptoms
The peculiarity of the clinical picture of a macular hole in the retina is that a person may not even be aware of the presence of such problems for a long time. One of the first signs of this pathology is a decrease in visual acuity. Since the macula is responsible for the visibility of objects, degenerative processes in this area of the retina become noticeable only when driving, reading or writing. In this case, the letters become blurry, and difficulties arise with the visibility of small details.
As the disease progresses and the size of the tear increases, another important symptom appears - distortion of the visible image. In this case, a person experiences difficulties when reading and sees straight lines as curved. With a through hole of the macula, a gray spot appears in the central field of vision. Sometimes these symptoms become noticeable only when the person closes the good eye. You should consult a doctor as soon as possible if the following signs appear:
- flashing “flies” before the eyes;
- a veil before the eyes;
- sharp flashes of light, most often occurring in the dark;
- narrowing of the field of view, loss of part of it;
- impaired color perception;
- diplopia;
- impaired refractive function of the eyes;
- distortion of the outlines and shapes of objects;
- periodic appearance of a gray spot before the eyes.
When the macular hole is incomplete, while reading, a person notices that letters disappear from words, lines are layered on top of each other. If you look at an object with a sore eye, you get the feeling that the visible object is much larger than if you look at it with a healthy eye. Often, signs of a macular hole in the retina are taken as manifestations of ordinary fatigue, which is why the patient is in no hurry to see a doctor. This leads to the pathology progressing, causing the development of blindness.
Read in a separate article: Retinal fibrosis: what it is, symptoms and treatment
Sometimes an imaginary well-being occurs, during which the symptoms disappear. However, this does not last long, and soon they return again.
Due to the lack of pain, a person often does not see a doctor until the very last moment, when visual function is almost impossible to restore.
Why do tears occur in the retina?
The most common causes of damage are:
- Suffered traumatic influences (bruises, chemical or thermal burns).
- Diseases associated with blood vessels (diabetes mellitus, hypertension).
- Myopia (myopia) of the eyes is a congenital change in the vitreous body.
- Brain diseases (neurosis and others).
The causes of retinal rupture should be known in order to prevent it. Thus, it is necessary to beware of negative influences on this organ, for example, direct bruises to the head, since the optic nerves may be affected. It is also undesirable to look at bright light for a long time.
This disease can be divided into both small ruptures and large-scale damage. In the first case, most likely, the disease can be cured without surgery. However, in the second case, unfortunately, it will not be possible to eliminate the disease without surgery using folk remedies.
Diagnostic methods
Due to the fact that the pathological process is asymptomatic for a long time, the rupture is often detected in an advanced form. To avoid this, you should consult a doctor if you have the slightest suspicion of visual impairment. The ophthalmologist can determine the nature of the problem based on the data obtained during the interview and physical examination of the patient. However, to confirm the diagnosis, determine the degree of its neglect and the cause of its origin, it is necessary to carry out the following diagnostic measures:
- Ophthalmoscopy. Using a special device, an examination of the fundus of the eye is performed, during which a lamellar gap can be noticed and its size can be determined.
- Biomicroscopy. The state of the eye structures is determined with a dilated pupil using direct lighting.
- Fluorescein angiography. It is used to detect the problem and differentiate macular hole from other pathologies.
- Visometry. The degree of visual acuity is assessed using special tables.
- Perimetry. Visual fields are studied.
- Optical coherence tomography (OCT) . One of the best ways to diagnose a macular hole in the retina, with the help of which a specialist obtains a detailed image of the retina and detects even minor defects.
The following research methods can also be carried out:
- Amsler test grid;
- tonometry;
- ultrasound scanning in beta mode;
- electroretinography.
In the absence of sufficient information about the condition of the retina and the course of the disease, various laboratory tests are additionally performed.
Surgical intervention
Surgery is the only way to cure a macular hole today. Surgical intervention can be performed using one of the following techniques:
Vitrectomy
It is carried out when both organs of vision are affected, as well as in case of a high probability of developing severe complications. The operation is carried out in several stages:
- 3 standard micropunctures are made, through which special equipment is installed for lighting, supply of saline solution and comfortable access to the defect;
- the affected areas of the vitreous body are excised;
- the posterior base of the vitreous is separated from the retina;
- the internal limiting membrane in the macula area is removed (thus closing the gap);
- A gaseous substance is injected into the eye cavity, which remains there until the vitreous body is filled with liquid (the gas resolves on its own within 14 days).
The operation is quick and painless, but there is a small risk of complications.
Laser coagulation
The safest treatment method for macular retinal hole. During the procedure, a laser is used to increase the temperature of the tissues, causing them to clot. As a result, fusion of the retina and choroid occurs, helping to restore vision. This minimally invasive operation is performed under local anesthesia, is not accompanied by bleeding and takes only 20 minutes, after which the patient can go home.
Reviews about this procedure are positive.
Cryocoagulation
By exposing the retina to low temperatures, a chorioretinal focus is created, as a result of which the gap is eliminated and vision is restored. The advantage of this operation is that it does not affect the sclera and muscle fibers.
The type of surgery is selected by the doctor individually. A number of factors are taken into account: the age and health of the patient, the nature of the injury, and the individual characteristics of the body.
Postoperative period
In order to reduce the risk of developing postoperative complications to a minimum, during the rehabilitation period, which lasts on average 5-7 days, it is necessary to follow the following recommendations of specialists:
- maintain eye hygiene, do not touch them with dirty hands;
- avoid intense physical activity and emotional stress;
- use antibacterial and anti-inflammatory eye drops prescribed by a doctor;
- avoid visual overload;
- avoid exposure to bad weather conditions;
- do not allow chemicals to come into contact with your eyes;
- refrain from applying decorative cosmetics during rehabilitation;
- wear a special protective bandage for the first 2-3 days;
- During the first few days, keep your head face down, placing your nose parallel to the floor (in this position, the gas bubble puts the best pressure on the macula, provoking its healing).
Also, during the postoperative period, you cannot visit saunas and steam baths, dive in open water and fly on airplanes.
Recovery after surgery
In the first days after surgery, the patient is under the supervision of the attending physician. The ophthalmologist prescribes eye drops for him, which prevent unwanted consequences and speed up recovery. In order to prevent infectious complications, the patient must be given antibiotics.
During the first 4–7 days after surgery, the patient is recommended to maintain a “face down” head position for as long as possible. This helps keep the gas bubble in the right place and creates optimal conditions for the rupture edges to heal.
In total, the recovery period after such an intervention lasts 1 month. After this period, the person can return to their usual lifestyle. Naturally, in the future he should take good care of his eyes, avoid injuries and visual fatigue.
Treatment with folk remedies
Since even drug treatment is not able to cure retinal macular hole, it is better not to try to get rid of the problem using traditional methods, since this is extremely dangerous. However, some experts argue that treatment with folk remedies helps to cope with the unpleasant manifestations of the disease and speed up recovery.
If the integrity of the retina is damaged, it is recommended to take decoctions and infusions of the following medicinal herbs:
- chamomile;
- fennel;
- calendula;
- celandine;
- eyebright.
Infusions can be taken orally or used as eye lotions. There are no reviews of alternative treatment for macular hole.
Before starting treatment with folk remedies, you must consult your doctor.
Possible complications
The retina is an important part of the visual analyzer, with the help of which a person can perceive the world around him. And if it is damaged, serious consequences arise, including complete blindness in one or two eyes. A macular hole causes retinal detachment, resulting in permanent vision loss. Therefore, it is very important to start timely treatment. But despite the fact that in almost 90% of cases the operation restores visual function, sometimes the following complications arise after surgery:
- defects in the field of view;
- iatrogenic retinal rupture;
- glaucoma;
- increase in macular hole.
One of the most severe postoperative complications is cataract – clouding of the lens.
Prevention
You can prevent the occurrence of a macular hole in the retina if you adhere to the following recommendations:
- protect your head and eyes from injury and mechanical damage;
- do not overload your eyes;
- promptly treat eye and central nervous system diseases;
- avoid intense physical activity and stressful situations;
- perform special gymnastics for the eyes;
- Healthy food;
- wear sunglasses;
- get rid of bad habits;
- lead a healthy lifestyle.
It is very important to undergo regular preventive examinations with an ophthalmologist. Especially if there are predisposing factors.
Author of the article: Kvasha Anastasia Pavlovna, specialist for the website glazalik.ru Share your experience and opinion in the comments.
Forecast and consequences
To prevent macular hole, it is necessary to avoid exposure to factors that have a damaging effect on the retina. At the same time, it is important to give up bad habits, eat right and engage in light sports. This will increase the strength of the macula tissue and help avoid accidental tears. After an injury, the prognosis for preserving the patient’s vision depends on the speed and scope of medical care. With lamellar tears, vision can be completely preserved, but extensive damage leads to impaired visual function.
Retinal tear: causes, symptoms and treatment.
Due to many factors, ophthalmological diseases can develop, which lead to impaired vision and even blindness. These include a tear in the retina, the retina through which our eyes perceive light. It remains to understand what causes this pathology, how it manifests itself and is treated.