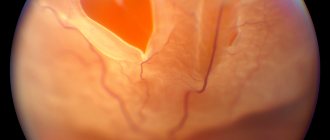
When the retina is detached from the adjacent choroid, irreversible consequences can occur that can lead to loss of vision. Various methods are used to treat detachment, one of which is episcleral filling. How this procedure is performed and what results it gives is in our article.
Episcleral filling is a type of surgical operation that ensures the adhesion of the retina to the choroid in the detachment zone by installing special fixing fillings on the sclera. These fillings, made of fine-mesh silicone, are sewn or installed seamlessly in those areas where the projections of detachment are located. The filling elements provide pressure on the sclera and press it against the choroid in the detached areas. This allows you to restore nutrition to the retinal cells and at least partially restore vision.
Filling is performed in different ways - radial, sectoral, circular - which directly depends on the scale and location of the detachment.
Extrascleral retinal ballooning
The purpose of extrascleral ballooning is to restore the impaired blood supply to the retina at the detachment site. A tight fit to the inner surface of the eye, penetrated by blood vessels, is achieved by “soldering” with a laser beam. In this case, access to the retina is provided by surgical intervention on the surface of the sclera. As a result of surgical manipulations, fluid may accumulate under the retina, but usually during the rehabilitation process such accumulation resolves without special treatment.
The idea of extrascleral ballooning is extremely simple: it consists in mechanically pressing the retina to the layer that nourishes it. However, this is very difficult to achieve: a special balloon is placed on the sclera in the area of projection of the retinal detachment, then through a catheter its internal space is filled with liquid, which creates the necessary pressure. However, this is only preparation for “soldering” laser coagulation: under the influence of a powerful laser beam with precisely calculated parameters, the detached areas of the retina are again fixed in the right place. Although the retinal tissue is already connected to the adjacent layers during the operation, the balloon is removed only 5-7 days after the formation of natural adhesions in the areas of exposure to the laser beam. The extrascleral ballooning operation is low-traumatic, but due to its technical complexity it lasts, by the standards of modern ophthalmology, quite a long time: from 30 to 50 minutes. When carried out in a timely manner, such treatment gives positive results in 98% of cases.
Retinal disinsertion
Diagnostics
Diagnostics will be carried out to examine the retina and assess its condition. It may include the following types of examination:
- Electroretinogram (recording of electrical signals in the retina made when you see things)
- Fluorescein angiography
- Measuring intraocular pressure
- Ophthalmoscopy
- Amsler test
- Retinal photography
- Test to determine the ability to see colors
- Visual acuity test
- Slit lamp examination
- Ultrasound examination of the eye
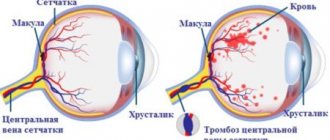
Treatment of retinal detachment
Most people with retinal detachment require surgery. The operation must be performed as soon as possible, because the nervous tissue that makes up the retina quickly dies without adherence to the choroid that feeds it.
Some types of retinal detachment surgery can be done in a doctor's office.
- Laser coagulation of the retina can be used if there is a rupture or degenerative changes leading to rupture.
More severe detachments may require surgery in the operating room. Such procedures include:
- Episcleral filling. When the sclera is brought closer to the retina from the outside using a special silicone filling that is sutured to the sclera.
- Vitrectomy. When the vitreous body with the cords that cause traction of the retina is removed, it is replaced with a special intraocular fluid, gas or silicone oil.
Prospects (forecast)
How well you will see after surgery depends on the extent, duration and nature of the retinal detachment. If the macular area was not affected, the outlook after treatment may be good.
Most retinal detachments can be operated on, but it is often not possible to restore high vision.
Without surgical treatment, retinal detachment leads to vision loss. The entire eye then dies and in some cases must be removed.
Retinal detachment surgery prevents the risk of eye loss and can help restore your vision.
When should you see a doctor?
Retinal detachment is a pressing problem that requires medical attention within 24 hours after the first symptoms appear.
Preventing retinal detachment?
Wear safety glasses to prevent eye injury. Monitor your blood sugar if you have diabetes. See your ophthalmologist at least once a year, especially if you have risk factors for developing retinal detachment.
Scleral retinal buckling
Scleral filling is aimed at restoring the adhesion of the detached area of the retina to the pigment epithelium that feeds it. This treatment, like alternative methods, allows you to preserve the viability and functionality of the retina if the patient seeks help in a timely manner. Delay and refusal of professional medical care for retinal detachment risks complete blindness.
Diagnostics prior to filling include assessment of the size, shape, location of the detachment area, as well as the approximate duration of the pathological process. This makes it possible to produce a strictly individual filling for application to the sclera. Modern fillings are made from biocompatible elastic silicone with a spongy structure.
Through an incision in the conjunctiva, the filling is placed in the desired location and secured with sutures. As an auxiliary technique, it is often necessary to introduce an expanding gas into the eye cavity. During treatment, fluid accumulation may occur, which is removed by drainage before suturing the conjunctiva.
The surgical plan for scleral retinal buckling is based on the results of preliminary diagnostics. Filling can be radial, sectoral and circular. The prognosis depends on the area of detachment, localization and preservation of nutrition of the adjacent areas of the retina. If general dystrophy occurs, there is a high risk of relapse (repeated detachment).
Possible consequences.
Complications after retinal filling are divided into 3 groups:
- Early postoperative period:
- infection of the surgical wound or tissues surrounding the eyeball;
- detachment of the choroid;
- imbalance of the extraocular muscles;
- increase in intraocular pressure;
- drooping of the upper eyelid due to muscle strain.
- Late postoperative period:
- exposure of the implant and, as a result, its possible infection;
- various changes in the macular area - the formation of microcysts, membranes and foci of degeneration;
- change in refraction towards myopia;
- cataract formation.
- Failed extrascleral filling.
- lack of a strong fit of the detached area of the retina;
- repeated retinal detachment.
Contraindications
Scleral ballooning and retinal filling are not performed in the following cases:
- retinal detachment is accompanied by extensive tears;
- retinal detachments are located along the dentate line;
- fixed retinal folds over a large area are observed in the fundus;
- with extensive tears in the posterior part (ballooning in this case carries a serious risk of deformation and formation of retinal folds);
- retinal rupture complicated by vitreous hemorrhage.
Recovery after surgery
Restoring vision in patients who have suffered retinal detachment is a long process, the end result of which cannot always be predicted. In most cases, patients' vision is not fully restored. Maximum visual acuity after extrascleral retinal filling surgery will depend on several factors, the main ones being the size of the damage, how involved the central parts of the retina are in the detachment process, and how long ago the retinal tear occurred.
Improvement in the patient's visual acuity after surgery occurs slowly. On average, it takes from several months to six months, but in people with myopia and elderly patients, the recovery period may take longer.
Preparing for surgery
If retinal detachment is suspected, it is necessary, first of all, to limit physical activity. Bed rest is most desirable for the entire period before the start of treatment. In any case, physical and emotional stress is contraindicated. If the patient is truly interested in preserving vision, he and his family should do everything possible to maintain the clinical status in a stable condition. In particular, detachment is often accompanied by the accumulation of subretinal fluid, and immobility allows you to reduce the volume of these bubbles, which reduces the total area of detachment and facilitates manipulation during surgical treatment.
Retinal detachment. What is important to know about it and how to recognize this disease
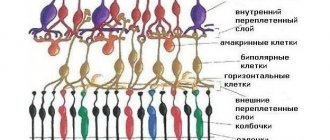
The retina is one of the membranes of the eyeball that lines it from the inside. This inner shell is a nervous tissue, the structure of which has more than 10 layers and provides image perception. Retinal detachment is a dangerous ophthalmological disease that requires immediate surgical intervention! It occurs due to a tear in the retina; through this tear, the vitreous body enters under the retina and detaches it from the choroid, which leads to complete or partial loss of vision.
Efficiency
The results of scleral ballooning and retinal filling depend not only on the skill of the surgeon, but also on a number of objective factors:
- area and structure of exfoliation;
- localization (primarily the involvement of the macular zone or its intactness);
- timeliness of medical care;
- patient compliance with preoperative and rehabilitation recommendations;
- general condition of retinal tissue;
- age, presence of chronic diseases and other anamnestic data.
With timely treatment and strict adherence to the recommendations of the attending physician, treatment is effective in 98% of cases. The operation restores blood supply to the retina and preserves its functionality. Visual acuity after ballooning and filling increases gradually.
In our ophthalmology center, vitreoretinal surgeries are performed by experienced surgeons using the most modern equipment from leading global manufacturers. This allows you to achieve a high treatment result and avoid possible complications. Trust your vision to professionals!
Preventive peripheral laser coagulation
The operation of preventive peripheral laser coagulation (PPLC) is a technique that is used to detect degenerative processes in the retina. These formations can further lead to the development of ruptures and detachments. The principle of the method is based on strengthening the retina with laser radiation of a certain wavelength.
An additional advantage of this intervention is improving the nutrition of the retina and reducing the permeability of its blood vessels. PPLKS refers to low-traumatic and effective methods of ocular microsurgery, which are performed on an outpatient basis and do not require hospitalization.
Laser radiation in this case does not affect visual acuity (since the refractive power of the transparent media of the eye does not change). The goal of treatment is to prevent retinal detachment and to stop the progression of the dystrophic process.
Rehabilitation after surgical treatment of retinal detachment
The rehabilitation period is one of the factors influencing the effectiveness of treatment. Failure to comply with postoperative recommendations can make even the most timely and qualified assistance pointless. It is worth understanding that normal nutrition of the retina is not restored at once: the operation only creates the conditions for recovery.
After surgery, swelling of the eyeball may develop, limiting its mobility. It is important to minimize visual stress (reading, watching TV) so that the swelling does not increase.
In the first days after surgery, strict bed rest must be observed. Then you are allowed to get up for a short time, but semi-bed rest must be maintained for 2-3 postoperative weeks. Sharp turns of the head and bends are especially dangerous; lifting weights and any other physical activity are strictly and completely excluded. A short stay in an upright position should be alternated with rest in bed. However, it is recommended to sleep on high pillows.
You can feel the effect of treatment only some time after the operation. Don't wait for sudden insight; many patients have to explain again and again that as blood supply to the retina is restored, vision returns gradually.
Rehabilitation.
Universal recommendations for the postoperative period (you must check with your doctor!):
- Compliance with the regime. This may be a certain position of the head or special bed rest, a ban on lifting loads of more than 5 kg. An individual regimen is developed for each patient;
- Hygiene. Avoid getting water and soap into your eyes when washing your face. When washing your head, you need to tilt your head back, not forward. If water gets into the operated eye, it is necessary to rinse it with an aqueous solution of chloramphenicol 0.25% or an aqueous solution of furatsilin 0.02%;
- Bandage. Wearing a bandage is recommended for the first few days after retinal filling. This is a measure to protect the eye from exposure to bright light and dust particles. The bandage is gauze folded in several layers. The bandage must be changed at least once a day;
- Eye drops. Necessary to improve healing and prevent possible complications. As a rule, disinfectant (Floxal, Tobrex) and anti-inflammatory (Naklof, Indocollir) eye drops are prescribed;
- Regularly visit your doctor!
Possible complications
The complexity of the intervention inevitably increases risks, incl. the likelihood of very serious complications. Thus, scleral filling and retinal ballooning can cause the development of cataracts, be complicated by hemorrhages and/or cause an increase in intraocular pressure.
Our highly qualified vitreoretinal surgeon will do everything possible to reduce such chances to a minimum. The rest is up to the patient; naive belief in a miracle that does not require one’s own efforts and reasonable self-restraints is just as dangerous here as the legendary “maybe.”
Prognosis and possible complications
Rhegmatogenous retinal detachment that occurs once is prone to recurrence. They occur in 80% of successfully operated patients already in the first year after the intervention. Another difficulty faced by patients with this type of detachment is incomplete restoration of visual acuity. Even timely surgery does not guarantee that the patient will see clearly, and in most patients, visual acuity remains reduced compared to the period before the rupture. However, in half of the patients, visual acuity partially improves within 1-2 years, but is not completely restored.
The most dangerous complication of the pathology is complete loss of vision.
. Patients with undiagnosed and unoperated pathology face it. Another group of complications are diseases caused by vitrectomy. These include hemorrhages in the preritinal, retinal or subretinal area, injury to the lens capsule, uveitis, and macular edema. Long-term consequences of the disease can be optic nerve atrophy, glaucoma and cataracts.
To reduce the risk of complications, the patient is recommended to strictly follow the doctor’s recommendations in the postoperative period and be regularly observed by an ophthalmologist, even if the functionality of the visual organs does not cause concern.