Classification of the disease
According to the anatomical structure of the uveal tract, the following types of uveitis are distinguished:
- Front. The development of inflammation in the iris and vitreous body is characteristic. This is the most common type of disease, which can occur in the form of iritis, anterior cyclitis, iridocyclitis;
- Intermediate. Inflammation affects the ciliary body, retina, vitreous body, and choroid. The pathology occurs in the form of posterior cyclitis, pars planitis;
- Rear. Damage to the choroid, retina, and optic nerve is typical. Depending on the location of the pathological process, chorioretinitis, retinitis, choroiditis, neurouveitis may occur;
- Generalized. The inflammatory process affects all parts of the uveal tract. In such cases, they talk about the development of panuveitis.
Depending on the nature of inflammation, 4 forms of pathology are distinguished:
- Serous;
- Purulent;
- Fibrinous-plastic;
- Mixed.
Based on etiological factors, uveitis is usually divided into:
- Endogenous. Infectious agents enter the eye through the bloodstream;
- Exogenous. Infection occurs as a result of injury to the choroid of the eye.
Uveitis can develop as a primary disease when it is not preceded by pathological processes. Secondary uveitis is distinguished when the pathology occurs against the background of other eye diseases.
According to the nature of the flow, they are distinguished:
- acute process, the duration of which does not exceed 3 months;
- chronic pathology that lasts more than 3-4 months;
- recurrent uveitis, when after complete recovery inflammation of the uveal tract develops again.
Uveitis
- Classification
- Clinical picture
- Diagnostics
Inflammation of the choroid of the eye (uveal tract). The frequency is 0.3-0.5 cases per 1,000 population, approximately 40% of cases of uveitis occur against the background of a systemic disease. Predominant gender: with anterior uveitis associated with the presence of HLA-B27 Ag in the blood, men become ill more often (2.5:1). This disease is a common cause of low vision and blindness (about 25%).
Anatomically, the choroid of the eyeball is divided into the iris, the ciliary body and the choroid itself, located behind the ciliary body and making up almost 2/3 of the choroid (actually lining the outside of the retina). The blood supply to the choroid itself is carried out mainly by the posterior short ciliary arteries, and the iris and ciliary body by the anterior and posterior long ciliary arteries, i.e. The blood supply to these two sections comes from different sources, so the anterior and posterior sections of the choroid are usually affected separately, which was the reason for the separation of anterior and posterior uveitis.
If you have uveitis, you should urgently consult an ophthalmologist. The main symptoms of the disease are “fog” before the eyes, blurred vision (even complete blindness is possible), redness of the eyes, photophobia and lacrimation.
Pathomorphology
- Anterior uveitis. Protein (including fibrin), red blood cells in the case of hemorrhagic inflammation, pus, and pigment are found in the aqueous humor of the anterior chamber. Synechiae (fibrous adhesions between the iris and lens) are also detected. The iris is swollen and infiltrated. Possible clouding of the vitreous due to the formation of connective tissue
- Posterior uveitis. Papilledema, inflammation of the perivascular tissue of the retinal vessels.
Classification
- Congenital
- Early childhood (from 0 to 3 years)
- Preschool and younger age (rheumatoid, peripheral)
- unilateral (viral, parasitic, uveitis in sarcoidosis, acute retinal necrosis)
- bilateral (uveitis in systemic diseases, peripheral uveitis)
Anatomical classification
By predominance of localization in the vascular tract (although isolated lesions are rare)
- Anterior uveitis (27-63%) - more often idiopathic iridocyclitis and HLA-B27 associated acute anterior uveitis, rheumatoid anterior uveitis, enteroviral uveitis in children, herpetic iridocyclitis, etc.
- Iritis - inflammation of the iris
- Anterior cyclitis - inflammation of the ciliary body
- Iridocyclitis - inflammation of the iris and ciliary body
- Peripheral (“medium”) uveitis (14-20%) (streptococcus, viral, idiopathic)
- Posterior cyclitis
- Pars planets
- Peripheral (basal)
- Retinochoroiditis
- Vitriites
- Posterior uveitis (19-38%)
- Focal (choroiditis)
- Multifocal (retinochoroiditis)
- Diffuse (neurouveitis, chorioretinitis)
- Panuveitis - the entire choroid of the eye becomes inflamed.
According to the nature of the flow:
- acute (sudden acute onset, average duration up to 6 weeks - most anterior uveitis, some posterior)
- subacute
- chronic (long course, less active onset - rheumatoid, tuberculosis, peripheral, sarcoidosis)
- sluggish, recurrent (with recurrent ones, activity during exacerbation is more pronounced, periods of remission are clearer than with sluggish ones)
According to the nature of infiltration of the affected tissues with inflammatory cells: granulomatous - specific granulomas in the iris or choroid (sarcoidosis, Harad syndrome, syphilitic, tuberculous uveitis) and non-granulomatous.
By etiology
- exogenous (post-infectious, autoimmune post-traumatic uveitis, sympathetic ophthalmia, phacogenic uveitis)
- endogenous (conditionally divided into infectious, infectious-allergic, non-infectious; “idiopathic”
- ambiguous understanding of terms, complex interpretation of the concept “etiology of uveitis” (more details in the monographs of L.A. Katargina)
The causes of inflammation of the choroid of the eye can be very different: infections, metabolic disorders, immunosuppression, autoimmune processes, etc. Uveitis can be a secondary disease, while the source of inflammation is located in another place, and the infection spreads hematogenously (with sore throat, meningitis, sinusitis , septic endocarditis). In some cases, uveitis can develop after penetrating trauma to the eye.
- Viruses, bacteria, protozoa, fungi
- Immune factors suggest the participation of autoimmune and immune complex mechanisms in diffuse connective tissue diseases
- Idiopathic causes (approximately 25%). Genetic aspects. In 50-70%, HLA-B27 Ag is detected (with ankylosing spondylitis, Reiter's disease).
Risk factors are diffuse connective tissue diseases, foci of chronic infection.
Clinical picture
Anterior uveitis (approximately 80% of patients with uveitis)
- Usually acute onset, most often unilateral (95% in cases of uveitis associated with the presence of HLA-B27 in the blood)
- Complaints: decreased visual acuity and pain in the eyeball, aggravated by palpation
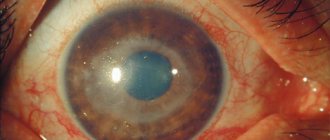
- Pericorneal or mixed injection, change in iris color (greenish or rusty color, unclear pattern)
- Constriction of the pupil of the affected eye, the shape of the pupil is incorrect, the reaction to light is impaired
- The presence on the endothelium of the cornea (from the side of the anterior chamber of the eye) of polymorphic precipitates or exudate in the anterior chamber (hypopyon in the case of a purulent nature of the exudate, hyphema in the case of a hemorrhagic one), the occurrence of posterior adhesions of the iris (fusion of the posterior surface of the iris with the anterior capsule of the lens) is possible. In some cases, adhesions can cause a circular fusion of the iris and lens, which leads to fusion of the pupil and an increase in intraocular pressure - secondary glaucoma and bombardment of the iris develop (it protrudes into the anterior chamber of the eye in the form of a roller)
- Manifestations of the underlying disease are possible both in the case of endogenous and exogenous origin of uveitis.
Posterior uveitis. Due to the close proximity of the retina and its frequent involvement in the inflammatory process, the term chorioretinitis is used in practice.
- The onset is usually inconspicuous
- Decreased visual acuity
- Complaints: the appearance of photopsia (flashes before the eyes), metamorphopsia (distortion of the shape of objects), hemeralopia (blurred vision in poor lighting) with peripheral localization of the process
- When examining visual fields - scotomas of various sizes (this research method does not require the participation of a qualified ophthalmologist, but allows one to suspect choroiditis)
- Characterized by the absence of pain, which greatly complicates diagnosis.
Intermediate uveitis is inflammatory infiltration of the vitreous body, exudation and formation of membranes that partially cover the ciliary body.
- The symptoms resemble those of posterior uveitis.
- Laboratory tests are nonspecific (the disease is polyetiological).
- Signs of the underlying disease are more often detected (laboratory indicators for collagenosis are the most informative).
Diagnostics
- Biomicroscopy for anterior uveitis - swelling, change in iris color, the presence of precipitates on the posterior surface of the cornea or exudate in the anterior chamber of the eye, posterior adhesions of the iris
- Ophthalmoscopy for posterior uveitis - opacities in the vitreous body, grayish or yellowish foci of various shapes and sizes with edema and hyperemia around (perifocal inflammation phenomena), the retinal vessels above them are not interrupted. Possible swelling and hyperemia of the optic nerve head. In the later stages, atrophic changes in the choroid occur - it becomes pale and sometimes pigmented
Additional research methods can identify signs of the underlying disease (for example, radiography of the spine for ankylosing spondylitis).
Intraocular inflammation is a polyetiological disease, one of the common complications of which is ocular hypertension, the frequency of which varies from 10 to 60%. A transient increase in intraocular pressure in most cases occurs during the acute phase of inflammation and is not accompanied by signs of glaucomatous optic neuropathy, which distinguishes ocular hypertension in uveitis from secondary glaucoma, which is recorded against the background of subsidence of acute signs of the inflammatory process or in the remission phase. Pathogenetic mechanisms of increased ophthalmotonus in uveitis include hypersecretion of aqueous humor, mechanical blockade of the anterior chamber angle with exudate and pigment, edema of the trabecular apparatus, the formation of anterior peripheral and posterior synechiae with the development of pupillary block, neovascularization of the anterior segment of the eye. \
Therapy of acute uveitis with intraocular hypertension aims not only to relieve inflammation, but also to adequately compensate for impaired ophthalmotonus without the subsequent development of persistent secondary glaucoma, which can be achieved by creating a balance between anti-inflammatory therapy and antihypertensive drugs. According to foreign authors, among the variety of antihypertensive drugs, β-blockers and carbonic anhydrase inhibitors are the drugs of choice in the treatment of uveal glaucoma and ocular hypertension. However, monotherapy with drugs from these groups, as well as in some cases, their combined use may be ineffective, which may require strengthening the antihypertensive regimen.
Brimonidine tartrate 0.2% is a highly selective α-2 adrenergic receptor agonist, which effectively and safely, according to the literature, reduces intraocular pressure (up to 25%) due to a dual mechanism of action, used both in monotherapy for ocular hypertension and in combination with timolol and carbonic anhydrase inhibitors. Thus, it is relevant to study the effectiveness of the combined use of β-blockers, carbonic anhydrase inhibitors and brimonidine tartrate in the complex therapy of ocular hypertension in uveitis.
Etiological factors
The following reasons for the development of uveitis are identified:
- bacterial infection caused by streptococci, staphylococci, chlamydia, toxoplasma, tubercle bacilli, Brucella, treponema pallidum, leptospira;
- viral infection: herpes virus (including the causative agent of chickenpox), cytomegalovirus, adenovirus, HIV;
- fungal infection;
- the presence of foci of chronic infection - tonsillitis, caries, sinusitis;
- development of sepsis;
- autoimmune diseases (rheumatism, systemic lupus erythematosus, spondyloarthritis, ulcerative colitis, Crohn's disease, polychondritis, interstitial nephritis, glomerulonephritis);
- eye injuries, burns, foreign bodies;
- hormonal imbalances;
- eye damage from chemical reagents;
- genetic predisposition;
- development of hay fever, food allergies;
- metabolic disorders.
The disease often develops in patients who have a history of other eye pathologies. In childhood and old age, infectious uveitis is mainly diagnosed, which occurs against the background of allergies or stressful situations.
Causes
The cause of uveitis is primarily considered to be the peculiarity of the structure of the choroid, as mentioned above. But if we talk about influencing factors, then first of all the disease is provoked by:
- Injuries;
- Infectious lesions;
- Metabolic disorders;
- Allergic reactions;
- Syndromic and systemic diseases;
- Violation of hormonal regulation.
The most common are infectious uveitis, which occupy a niche of 44%. In such cases, the pathogens that caused the disease are tuberculosis bacteria, toxoplasma, streptococci, cytomegalovirus, fungi, herpes virus, and so on. In this case, the focus of development will not necessarily be in the eye area. The pathogen simply needs to enter the bloodstream and reach the eye area. Most often, this pathology develops with tuberculosis, syphilis, tonsillitis, caries, sepsis, and so on.
Important! There are many causes of uveitis and it is impossible to determine them accurately without examination. For example, children are characterized by traumatic and infectious diseases, while in adults the most common are infectious and systemic diseases. But even this is not a 100% guarantee.
Allergic uveitis is not infectious in nature. In such cases, the immune system plays a major role. And her reaction to allergens - medications, food, pollen, fluff, and so on. In this case, even serum uveitis may develop, which usually occurs after the administration of vaccines and serums.
Uveitis is often caused by systemic or syndromic pathologies, for example, rheumatoid arthritis, psoriasis, Reiter's syndrome, rheumatism, sarcoidosis, colitis, and so on. In such cases, in parallel with uveitis, it is necessary to treat the underlying pathology. Rheumatoid uveitis of the eye often develops as a complication of rheumatoid arthritis.
Caused by trauma, uveitis can develop after a burn, mechanical contusion or penetrating injuries, or foreign bodies. Hormonal and metabolic dysfunction in diabetes mellitus, diseases of the circulatory system, menopause, diseases of the organ of vision and other pathologies and conditions often lead to inflammatory processes in the choroid.
Important! Sometimes the cause of uveitis cannot be determined. In such cases, a diagnosis of “unspecified ocular uveitis” is made.
Symptoms of the disease
The clinical picture depends on the localization of the inflammatory process, the state of the immune system, and the nature of the disease. In acute anterior uveitis, patients report the following symptoms:
- soreness and redness of the affected eye;
- constriction of the pupil;
- increased lacrimation;
- photophobia;
- decreased visual acuity and clarity;
- increased intraocular pressure.
Chronic inflammation of the anterior uveal tract is characterized by an asymptomatic course. Only in some cases do patients notice slight redness of the eyeballs and the appearance of dots in front of the eyes.
A characteristic sign of peripheral uveitis is damage to both eyes. Patients complain of decreased central vision and the appearance of “floaters” before the eyes.
The following symptoms are typical for posterior uveitis:
- feeling of blurred vision;
- objects become distorted;
- the appearance of floating spots before the eyes;
- decreased visual acuity.
It is also possible to develop macular edema, optic neuropathy, macular ischemia, and retinal detachment.
Diagnostic measures
Diagnosis of uveitis is carried out by an ophthalmologist. As part of the initial appointment, the specialist must examine the eyes, check visual acuity, visual fields, and conduct tonometry to determine the value of intraocular pressure.
Additionally, the following studies are carried out:
- Ultrasound of the eye;
- study of pupillary reaction;
- biomicroscopy, which involves examining the eye using a slit lamp;
- gonioscopy, which allows you to determine the angle of the anterior chamber;
- ophthalmoscopy. The study is carried out to study the fundus of the eye;
- fluorescein angiography of the retina;
- tomography of various eye structures if necessary;
- electroretinography;
- rheoophthalmography, which allows you to measure the speed of blood flow in the vessels of the eyes.
Features of treatment
Drug therapy for anterior and posterior uveitis involves the use of the following groups of drugs:
- Broad-spectrum antibiotics (fluoroquinolones, macrolides, cephalosporins). Drugs can be administered subconjunctivally, intravitreally, or parenterally. The choice of a suitable antibiotic depends on the type of pathogen, its sensitivity to drugs;
- Antiviral drugs are prescribed for the treatment of uveitis of viral origin. Widely used: Acyclovir, Zovirax while taking Viferon or Cycloferon. Medicines are prescribed in the form of intravitreal injections or taken orally;
- Non-steroidal anti-inflammatory drugs and glucocorticosteroids can stop inflammation in a short time. Dexamethasone or prednisolone drops are prescribed subconjunctivally, Ibuprofen, Movalis or Butadione are taken orally;
- Immunosuppressants are used when anti-inflammatory treatment is ineffective. Cyclosporine and Methotrexate are indicated, which can suppress immune reactions; To prevent the occurrence of adhesions, drops of Cyclopentolate, Tropicamide, Atropine are recommended;
- Fibrinolytics have a resolving effect. Widely used: Gemaza, Lidazu, Wobenzym;
- Complex multivitamins;
- Antihistamines: Claritin, Lorano, Cetrin, Clemastin, Suprastin.
If drug therapy helps eliminate acute inflammation, then physiotherapeutic treatment is indicated. Electrophoresis, infitatherapy, laser blood irradiation, vacuum pulse massage, phototherapy, phonophoresis, laser coagulation, cryotherapy are highly effective.
Treatment of uveitis
After a full diagnosis with determination of the area and nature of the lesion, a course of adequate, comprehensive therapy is determined. Drug and systemic drug treatment is mainly used. Surgery may also be performed to correct complications of uveitis, but these are rare cases. Typically, classical therapy is practiced using different types of medications. Some of them involve administration in a hospital setting, but most are used either orally or topically in the form of drops, ointments, and so on.
Therapy is carried out under the careful supervision of an ophthalmologist and other specialists. When diagnosing uveitis, differential diagnosis plays an important role. Based on the diagnosis, the following is prescribed:
- Substitute;
- Pathogenetic;
- Etiotropic;
- Corrective therapy.
At the same time, treatment is being carried out for the root cause - the pathology that provoked uveitis. It is prescribed by a specialized specialist after conducting an appropriate examination.
Drug treatment
Drug therapy involves the use of a number of drugs. This largely depends on the type of pathology, the presence and type of pathogens, and so on. Mainly used:
- Antiviral and antimicrobial medications;
- Mydriatics - atropine, phenylephrine and so on;
- Steroids - prednisolone, dexamethasone, and so on;
- Systemic immunosuppressants;
- NSAIDs;
- Cytostatics;
- Antihistamines.
Mydriatics eliminate the spastic state of the ciliary muscle. They also prevent the development of adhesions and fistulas. Also, drugs of this type help to break up already formed adhesions.
Hormonal drugs are perhaps the main method of treating uveitis. They are not used only for fungal infections. Such medications are used both locally and systemically. If the effectiveness is low or completely absent, then immunosuppressants are prescribed in parallel. So, for different pathologies, different drugs can be used:
- Syphilitic uveitis requires the use of benzylpenicillin drugs, doxycycline, tetracycline, erythromycin.
- Leptospirosis is treated with gemma globulins, doxycycline, amoxicillin, sulfone.
- Parasitic involves the use of mebentazole, thiabenzene.
- Brucellosis involves the use of sulfonamides, tetracyclines, aminoglycosides.
- The tuberculosis variety is treated with rifampicin and isoniazid.
- For toxoplasmosis uveitis, sulfadimezine, pyrimethamine, and folic acid are used.
- For herpes, acyclovir and valacyclovir are used.
In parallel, agents that promote vasodilation are used, as well as immunostimulants and physiotherapy. For increased pressure inside the eyes, antiglaucoma medications are used. The duration of treatment is determined by the doctor.
Hormonal drugs are usually used in short courses due to their systemic effect on the body. But the doctor can extend their use if there are certain indications, for example, for psoriasis, hormonal drugs are used for a month or more. Cancellation is carried out gradually with decreasing dosages and extending the time between use of funds.
Important! Hormonal medications require a doctor's prescription. Available only by prescription. It is prohibited to use several funds from such a group at once. If side effects occur, you should consult your doctor about discontinuing or replacing the drug with another one.
Physiotherapy
To increase the effectiveness of treatment, physiotherapy is also used. Its effectiveness has been proven over time. But it is worth considering that such procedures can only be applied after the severity of the pathology has been relieved:
- Electrophoresis;
- Hirudotherapy;
- Phonophoresis.
These are effective techniques that will help you quickly cope with the disease, and in case of a chronic type of pathology, put it into a stage of long-term remission.
Surgical intervention
Surgical intervention is practiced mainly to eliminate complications that have developed against the background of uveitis, for example, to dissect the area of fusion of the iris with the lens. Surgical treatment of glaucoma, retinal detachment, cataracts, and so on can also be performed. Depending on the type of pathology, techniques such as:
- Vitrectomy for iridocyclochoroiditis;
- Evisceration when it is impossible to save the eye.
The success of a particular surgical procedure depends on the type of complication. Sometimes the eye cannot be saved, and sometimes vision can be restored to 100%.
Important! Do not be afraid to go to the doctor because of the risk of prescribing a surgical procedure. This is an extremely rare phenomenon and is accepted only after attempts to cure the patient in the classical way. The longer the pathology is delayed, the greater the chances of falling under the surgeon’s knife.
Where are they treated?
This pathology can generally be treated at home, but it is necessary to first undergo a diagnosis. An accurate determination of the pathology and its causes will allow you to correctly and completely cure your eyes. Some products can only be administered by qualified healthcare professionals. In this case, it is necessary to remain under the supervision of the establishment’s specialists for some time.
Sometimes semi-inpatient treatment may be used, when the patient comes to the hospital for manipulations or medication. Modern medicine offers many different techniques and medications that will help to cope with pathology as quickly as possible.
Important! It is better to seek help from qualified ophthalmological institutions that have already proven themselves in this area. This way you will receive high-quality service and complete diagnostics.
Surgical intervention
The development of complications or severe course of uveitis requires surgical treatment. The operation may include the following steps:
- dissection of the commissure between the iris and the lens;
- removal of vitreous, glaucoma or cataracts;
- soldering of the retina using a laser;
- removal of the eyeball.
Surgery does not always have a favorable outcome. In some cases, surgery causes an exacerbation of the inflammatory process.
Traditional medicine methods
During the treatment of uveitis, you can use some folk recipes. However, before any manipulation it is necessary to consult a doctor .
The following recipes will help effectively eliminate inflammation:
- washing the eyes with a medicinal decoction. It is necessary to take equal quantities of chamomile, calendula, and sage flowers. Grind the raw materials. Take 3 tablespoons of the mixture and pour a glass of boiling water. The composition is infused for 1 hour. Strain the resulting product and rinse the eyes with the decoction;
- aloe juice is diluted with cold boiled water in a ratio of 1:10. The resulting solution is dripped 1 drop no more than 3 times a day into the affected eye;
- marshmallow root lotions. The raw materials should be crushed, pour 3-4 tablespoons of 200 ml of cold water. The product is infused for 8 hours, then used for lotions.
Treatment of panuveitis
Panuveitis is quite difficult to treat. If it is possible to identify the cause of inflammation, then etiotropic treatment is prescribed. Thus, for cytomegalovirus, ganciclovir is prescribed, for nephropathy - antibiotics and other specific drugs. For all types of generalized uveitis, painkillers, mydriatics (to prevent the formation of synechiae), anti-inflammatory steroidal and non-steroidal drugs are used. In the presence of a viral or bacterial infection, it is advisable to use antibiotics and antiviral agents.
Complications and prognosis
Without effective treatment, uveitis can lead to the development of serious eye diseases:
- cataracts, in which the lens becomes cloudy;
- damage to the retina up to its detachment;
- glaucoma, which develops due to impaired outflow of fluid inside the eye;
- persistent vitreous opacification;
- damage to the optic nerve;
- pupillary fusion, in which the pupil stops responding to light due to adherence to the lens.
With timely and comprehensive treatment of acute inflammation of the eye, it is possible to completely cure the patient in 3-6 weeks. However, chronic uveitis is prone to relapses when the underlying pathology worsens, which significantly complicates therapy and worsens the prognosis.
Uveitis is an inflammatory pathology of the choroid of the eye that can lead to complete loss of vision. Therefore, it is so important to diagnose and begin treatment of the disease in time. Prevention of the disease is of great importance, which involves timely treatment of pathological processes in the body, exclusion of household eye injuries, and allergization of the body.