All organs, tissues, structures and systems of the human body can be susceptible to inflammatory processes. This even applies to the system of blood vessels, where, it would seem, there is nothing to become inflamed - except the vascular walls. In medicine, there are several general terms to refer to vascular inflammation (vasculitis, angiitis), as well as a number of specific terms indicating the nature or localization of the affected vessels (arteritis, phlebitis, etc.).
The eyeball is “braided” with a network of thin blood vessels that nourish and saturate with oxygen all intraocular elements and media. The ocular vascular system, in its organization, is essentially no different from any other: blood enriched in the lungs enters the arteries, is delivered and distributed in the tissues by the smallest capillaries, then is discharged, along with metabolic products, through the veins. Normally, the vascular network of the eye is practically invisible; if we notice swollen, inflamed or, in common parlance, “burst” eye vessels, this is always a pathology and always a symptom.
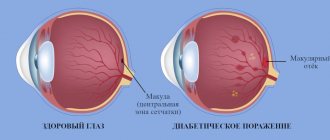
The blood supply system of the eye is called the “uveal tract” and consists of the iris (anterior section), ciliary body (middle section, also responsible for accommodation) and choroid (posterior section, which can be called strategic: this is the choroid itself, providing nutrition and oxygenation and regeneration of the photosensitive retinal tissue that covers the inside of the fundus of the eye).
In accordance with the rules of word formation accepted in medicine, inflammation of the vascular system of the eye is designated by the term “uveitis”. It is believed that the original name “uvea” (ancient Greek “grape”) was inspired by the grape-shaped appearance of the ocular choroid, which association becomes especially clear during inflammation.
Causes of uveitis
The statistical share of uveitis in the clinic of ophthalmological diseases is not so large, but noticeable: it is 5-7%. Depending on the location of the lesion, anterior uveitis (inflammation of the iris and/or ciliary body); posterior uveitis , or choroiditis (inflammation of the “back” choroid of the retina, the retina itself and the optic nerve); as well as panuveitis - total inflammation of the entire circulatory system of the eyeball.
Speaking about the causes of uveitis, as well as any other vasculitis, it should be noted that not everything in the etiology and pathogenesis of vascular inflammation has been studied and explained to date.
The dominant cause of any (not only vascular) inflammation is the vital activity of pathogenic microorganisms - viruses, bacteria and fungal cultures, however, in this regard, their sudden activation does not always seem natural and explainable, to which neither the body’s immune defense nor even timely medication has time to fully respond counterattack.
Accordingly, the causes of purely infectious uveitis are toxoplasmosis, syphilis, chlamydia, brucellosis, tuberculosis and other bacterial invasions, pathologically rapid proliferation of fungi (for example, the candida genus), herpes viruses, measles, cytomegalovirus, etc.; in some cases - infection by parasites.
However, a connection has also been established, at least statistically (which indicates a reliable cause-and-effect relationship, which remains to be clarified) between uveitis and background systemic inflammatory processes, such as rheumatism, ankylosing spondylitis (Bechterew-Strumpel-Marie disease), complex infectious-allergic syndromic Reiter triad (urethritis-conjunctivitis-arthritis). Sometimes uveitis develops after and, presumably, as a result of ophthalmic trauma. One of the risk factors is genetic predisposition.
Finally, in some cases the causes of uveitis remain simply unknown.
Benign tumors of the vascular tract
Treatment of Cancer >> Books on Oncology >> “Handbook of Oncology” Edited by Professor B. E. Peterson Third edition, revised and expanded Publishing House “Medicine”, Moscow, 1974 OCR Wincancer.Ru Given with some abbreviations
Main localization of intraocular tumors is the vascular tract of the eye in adults and the retina in children. They are observed mainly in the iris, but are rare in other parts. Most of them relate to neoplasms of a neuroectodermal nature: fibroids, neuromas, nevi, etc.
FIBROIDS
. Iris fibroids. They develop from the smooth muscle fibers of the sphincter or dilator. They have the appearance of a grayish or grayish-yellow nodule, but there may also be pigmented fibroids, which are difficult to distinguish from melanoblastomas. With special staining, myofibrils are found in the cytoplasm of fibroid cells. Tumor growth is slow and lasts for years. With a progressive course, fibroids acquire a tendency towards infiltrative growth. The tumor does not metastasize. Treatment. Removal of the tumor if it tends to grow.
NEURINOMA AND NEUROFIBROMA
. Neuromas and neurofibromas of the choroid usually present as manifestations of Recklinghausen's disease. Neurofibromas are most often observed in the iris in the form of multiple small grayish-brown nodules measuring 0.5-1.5 mm.
NEVUS
. Nevi of the vascular tract of the eye are focal accumulations of pigment-containing cells. They do not have the histological structure characteristic of nevi of the skin and conjunctiva. They occur much more often than other benign neoplasms. Being congenital neoplasms, iris nevi, as a rule, remain stationary.
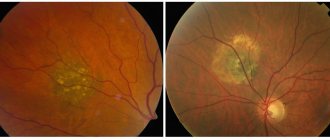
Choroidal nevi appear to be more common than they are diagnosed. They are best identified when examining the fundus with a wide pupil in the form of flat, slate-gray spots with blurry boundaries. In red-free light, pigmentation disappears, the functions of the eye are not affected. Choroidal nevi can undergo malignancy. Patients with choroidal nevus require observation.
MELANOMA
. Melanocytoma of the optic disc is characterized by excessive pigmentation of the disc and adjacent parts of the choroid. It does not worsen vision or increase the blind spot. Melanocytoma must be differentiated from choroidal melanoblastoma located near the optic nerve head.
ANGIOMA
. Vascular tract angioma is a rare tumor. Angiomas located in the iris are often accompanied by recurrent hemorrhages in the anterior chamber. Choroidal angioma in half of the cases is accompanied by nevus flammeus on the same side of the face. With a single lesion, the tumor is often mistaken for melanoblastoma, and only histological examination can clarify the nature of the disease.
Angiomas are located mostly near the optic nerve head and are early complicated by extensive retinal detachment, cystic retinal degeneration and later secondary glaucoma.
Fluorescein angiography can serve as an auxiliary diagnostic test. In the early stages of the disease, tumor photocoagulation may be effective. See further: Malignant tumors of the vascular tract >>
Symptoms of uveitis
The clinical picture of ophthalmovascular inflammation is determined by a number of conditions: the nature of the pathogenic factor, the localization of the primary lesion, the speed and intensity of development. Accordingly, the symptoms of uveitis are very diverse.
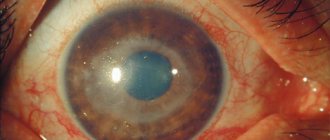
Thus, more or less typical manifestations of anterior uveitis are subjective sensations of “veil before the eyes” and heaviness in the eyeball; decreased visual acuity and clarity; noticeable redness of the sclera; aching, “pulling” or sharp pain; miosis (constriction of the pupil) with weakened or absent response to light, or, on the contrary, a painful reaction of the eye to bright light; hyperlacrimation (increased lacrimation); surge in IOP (intraocular pressure). The extreme, limiting symptom of uveitis in some cases is complete loss of vision.
Posterior uveitis (choroiditis) is dangerous due to a long period of asymptomatic development, when there are neither visible signs nor subjective painful sensations. A decrease in visual acuity and quality also develops, as a rule, too slowly and gradually for the patient to notice it in the early stages. Seeking help is usually due to obvious “fogging” or the appearance of scotomas (blind spots) in the field of vision.
Diagnosis and treatment of uveitis
Of course, the chances of radical therapeutic success in uveitis depend decisively on how quickly and adequately its treatment is prescribed. If the inflammatory process manages to go far enough, the risk of developing complications, including severe ones, increases - up to cataracts, glaucoma (if the drainage of intraocular fluids is disrupted), fusion of the pupil and the appearance of posterior synechiae (fusions, adhesions), loss of transparency of the vitreous body, damage optic nerve and/or retina (neovascularization, i.e. formation of new vascular networks, detachment). In cases where only one eye is primarily affected, if there is a delay in starting therapy, the second (healthy) eye may become involved in the inflammatory process.
However, early diagnosis and treatment of uveitis is not always possible, and the reasons for this are not only due to the subjective factor (late presentation, absence of symptoms in the initial stages of posterior uveitis). In some cases, uveitis is objectively difficult to diagnose: biomicroscopy of the anterior ocular structures, ophthalmoscopic examination of the fundus, ultrasound scanning or more complex instrumental diagnostic methods is required (and is not always performed). But even with a full-scale and relatively timely examination, it is not always possible to establish the direct cause of inflammation: according to available medical and statistical information, in 30% of cases of uveitis, its pathogenic factor remains unknown. In this case, accordingly, etiopathogenetic treatment (targeted not only at the symptoms, but also at the direct cause of the disease) can only be prescribed thanks to the doctor’s intuition or simple luck of the patient. The general treatment protocol for etiologically unclear uveitis includes anti-inflammatory measures (both local and systemic), antibiotic and immunostimulating (antiviral) drugs, vasodilators, enzyme and physiotherapy.
Medicines of all pharmacological forms are used: drops, ointments, gels, conjunctival and parabulbar injections, tablet preparations, etc. Particular importance is given to mydriatics - drugs that block accommodation and dilate the pupil - to prevent adhesions. In cases where uveitis is accompanied by increased intraocular pressure, hirudotherapy (placement of medicinal leeches) is often highly effective.
It is very difficult to heal a disease without knowing its causes and internal patterns; in many cases, healed uveitis recurs. Therefore, a strategically correct step, the need for which is extremely important to bring to the patient’s consciousness, is to continue an in-depth and comprehensive examination even after symptomatic improvement has been achieved.
Malignant tumors of the vascular tract
Treatment of Cancer >> Books on Oncology >> “Handbook of Oncology” Edited by Professor B. E. Peterson Third edition, revised and expanded Publishing House “Medicine”, Moscow, 1974 OCR Wincancer.Ru Given with some abbreviations
Melanoblastoma is the main primary tumor of the vascular tract. It occurs mainly at the age of 50-70 years as a unilateral disease. Histologically, there are 3 main types: spindle cell, epithelioid cell and mixed melanoblastoma. The most malignant of them is epithelioid cell, in which the mortality rate reaches 70-80%, while in the more benign form, spindle cell, it is only 10-30%. Melanoblastomas of the choroid are characterized by a predominantly hematogenous route of metastasis, with the liver most often affected. Most often, melanoblastoma originates from the choroid. Damage to the choroid is noted in 85%, ciliary body - in 9%, iris - in 6% of cases.
MELANOBLASTOMA OF THE IRIS
. It is observed in the form of two main forms - nodal and planar. Most of them are pigmented. The spindle cell structure of the tumor predominates. Growth is very slow and lasts for years. As the tumor grows, it can cover a significant extent of the iris, fill the anterior chamber, and involve the ciliary body in the process. The prognosis for life is much more favorable than with melanoblastomas of the choroid and ciliary body. Metastases are very rare.
The group of melanoblastomas with a special course includes the iridociliary form as a type of planar form. It is characterized by circular growth with simultaneous damage to the ciliary body, iris and anterior chamber angle along its entire length. In the clinical course, there is an early increase in intraocular pressure, a progressive change in color and blurring of the iris pattern, and early growth beyond the eyeball. The prognosis is always very serious; generalization of the tumor process and death are possible.
Treatment
. For isolated compact tumors of the iris, local surgical removal is indicated - iridectomy or iridocyclectomy; if the tumor has grown into the root of the iris or the ciliary body, when choosing a surgical method, determining the boundaries of the tumor is extremely important. For this purpose, biomicro-, gonio- and diaphanoscopy are used. For planar, diffuse tumors of the iris with circular involvement of the anterior chamber angle, and for the iridociliary form, enucleation of the eyeball is indicated.
MELANOBLASTOMA OF THE CILIARY BODY
. At first, the tumor does not give any symptoms. As its size increases, changes associated with the impact on the adjacent parts of the eye come to the fore: congestive injection of the anterior ciliary vessels in a limited area according to the location of the tumor; contact opacification of the lens, its deformation, and sometimes displacement. In some cases, early tumor growth into the root of the iris is observed.
Diagnostics
. Gonioscopy and diaphanoscopy provide valuable information. With transscleral transillumination, when the diaphanoscope is inserted as far as possible into the area of the conjunctival fornix, on the side opposite to the location of the tumor, it is possible to clearly determine its contour and boundaries.
Treatment
. Enucleation of the eyeball. Only in rare cases, with a limited tumor node, is local excision possible.
MELANOBLASTOMA OF THE VACUUM
(choroids). The most common form of growth is nodular, the rarer is planar. With a nodular form, the tumor takes on a rounded shape with clear boundaries, often in the shape of a mushroom. Depending on the pigment content, the tumor appears dark or light brown, and sometimes pink, devoid of pigment. Planar melanoblastoma grows diffusely in the thickness of the choroid, spreading over a large area of the fundus. A characteristic feature of the growth of this form is its early growth beyond the eyeball, sometimes with the formation of massive extrabulbar nodes, which is often mistakenly interpreted as a primary orbital tumor. The first clinical manifestations of the tumor depend on its location in the choroid. If melanoblastoma is located outside the macula, it is asymptomatic for a long time. During the process of progressive tumor growth, dystrophic changes develop that affect the clinical picture of the disease.
There are 4 stages of development of choroidal melanoblastoma: 1) stage of a quiet eye; 2) stage of development of complications (glaucoma or inflammatory process); 3) stage of tumor growth outside the eye; 4) stage of generalization of the process with the development of distant metastases.
Diagnostics
. Diagnosing choroidal melanoblastomas often causes great difficulties. A tumor in the initial stage of development should be differentiated from a nevus, chorioretinitis, exudative Coatz retinitis, limited subretinal hemorrhages, and discoid macular degeneration. Diagnosis can be extremely difficult when a tumor remains in the eye for a long time and secondary changes in the eye tissue develop - retinal detachment, vitreous hemorrhages, secondary glaucoma. The group of melanoblastomas with a special course includes necrotizing melanoblastoma. Rapidly developing total tumor necrosis gives a picture of an acute severe attack of glaucoma, combined with symptoms of inflammation of the uveal tract of the eye.
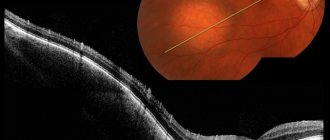
To recognize the disease, in addition to ophthalmoscopy, biomicroophthalmoscopy is necessary using a slit lamp, which helps to identify even slight elevation of the lesion, get an impression of the density of the tissue, and in case of extensive retinal detachment, detect a tumor node underneath it.
Diaphanoscopy (examination of the eyeball using a special lamp) is most valuable when the tumor is localized in the anterior half of the eyeball. When the diaphanoscope lamp is positioned in the tumor area, there is no glow from the pupil, but when illuminated from counterpoint, a shadow corresponding to the contours of the tumor is revealed on the sclera.
The radioisotope research method using P32 helps to clarify the diagnosis of a malignant tumor. The method is most effective in cases where it is possible to bring the counter relatively tightly to the focus being examined. Tumors of the posterior segment of the eye require a transconjunctival approach. Ultrasound diagnostics is of great help in tumor recognition in opaque optical environments. The diagnostic capabilities of these methods are significantly expanded when used in combination.
Treatment
. The main method of treatment is enucleation of the eyeball, and if there are signs of tumor growth into the orbit, exenteration of the orbit. In the postoperative period, deep radiotherapy is performed. In recent years, a more promising method of radiation therapy has been used - chipping the stump with a colloidal solution of radioactive gold Au198 with a total activity of 5-7 microcuries. The advantages of the method are that it is possible to concentrate large doses of radiation in the soft tissues of the orbit and dramatically reduce the radiation dose to the eyelids.
Patients maintain eyelash growth, atrophy of the eyelid skin and conjunctival xerosis do not develop, and good conditions for wearing a prosthesis are maintained. Chemotherapy (ThioTEF, sarcolysin) is used in combination with surgical and radiation treatment for stage II-III melanoblastomas. For small localized tumors no larger than 3-4 optic disc diameters and up to 1-1.5 mm in length, photocoagulation of the tumor is possible. Attempts are being made to treat small and flat tumors using beta applicators sutured to the sclera.
The prognosis is serious.
Depends on the stage of the disease, the cellular structure of the tumor. The prognosis of the disease is aggravated by tumor growth into the emissaries, blood vessels, and beyond the eyeball. Metastases mostly develop in the first 3-5 years after surgery, but they can also appear at a much later date. See further: Benign retinal tumors >>