Benign tumors of the orbit can be soft tissue, skeletogenic, epithelial, or originate from the optic nerve [Paches A.I., et al., 1980].
The first include fibroma, lipoma, myoma, myxoma, hemangioma, lymphangioma, neurofibroma, neuroma.
A glioma arises from the optic nerve.
Skeletogenic tumors are osteomagus chondroma.
In children, the most common tumors are vascular tumors - 27.6%, optic nerve glioma - 21.6%, dermoids - 9.2%, neurofibromatosis - 5.9% [Barkhash S. A., 1978].
Eye neoplasms – what are they?
The delicate and sensitive tissues of our eyes, unfortunately, are vulnerable to many carcinogenic factors: radiation, chemicals, some viruses, burns and injuries. There may also be hereditary reasons for their degeneration. Tumors of the organs of vision and surrounding tissues are so diverse that they are studied by a special branch of clinical medicine - ophthalmo-oncology. Due to the many variations of eye tumors, diagnosing the problem is not always easy; this requires a comprehensive examination by a highly qualified ophthalmologist. But, whatever the diagnosis, there is no need to be afraid - modern treatment methods have come so far that there is a suitable method for every case.
Classification of tumors of the eye and surrounding tissues
The same classification applies to tumors of the visual organs as to tumors in general. They are divided into:
- Benign - slowly growing, does not metastasize, and does not have a toxic effect. They can degenerate and become malignant. Among eye tumors, this type includes: papilloma, senile wart on the eyelid, benign nevus and a number of others
- With locally destructive growth - those that do not metastasize, but have invasive growth (intermediate category). Basal cell carcinoma and progressive nevus are characterized by such growth
- Malignant - fast-growing, destroying other tissues and releasing toxins. Their cells are transported with the blood to other parts of the body and can give rise to secondary lesions (metastases). Examples: cancer of the conjunctiva, meibomian glands, melanoma and sarcomas of the eyelids.
Eye tumors are also classified according to their location in the affected organ.
:
- Tumors of the orbit (eye socket)
- Tumors of the adnexal apparatus of the eye (eyelids, conjunctiva)
- Intraocular tumors (choroid and retina).
Tumors of the conjunctiva
Conjunctival cancer is a primary malignant tumor of the conjunctiva, usually arising against the background of precancerous diseases. It is rarely diagnosed and mainly affects older people. Men get sick more often than women. A risk factor is constant excessive sun exposure. In appearance, a conjunctival tumor may resemble Bowen's disease or keratinizing papilloma. It is a grayish or whitish film riddled with telangiectasia, or a cluster of pinkish nodules. As the conjunctival tumor grows, it spreads to nearby tissues, can invade the orbit, and metastasize to the cervical and parotid lymph nodes.
Cancer can also be located on the inside of the eyelid. Such neoplasms are more malignant than tumors of the conjunctiva located in the sclera. In the initial stages, the node grows intraconjunctivally, causing thickening and hardening of the eyelid. Subsequent ulceration is possible. As the conjunctival tumor progresses, it spreads to the lacrimal caruncle, cornea and scleral conjunctiva, but does not invade the tarsal plate.
The diagnosis is made based on examination and biopsy results. Limited nodes of small size are subject to surgical removal. It is possible to use diathermocoagulation. For large conjunctival tumors, radiotherapy or beta therapy is used. If the orbit is affected, orbital exenteration is performed. The prognosis is quite favorable. For tumors that do not spread to the orbit, the absence of relapses within 5 years after the end of treatment is observed in 50-80% of patients.
Melanoma is a malignant tumor of the conjunctiva that occurs against the background of acquired melanosis (75%), progressive nevus (20%) or unchanged tissue. It is a smooth or lumpy tumor-like formation. It can be pigmented (yellowish, brown) or lack pigment. Usually located at the inner corner of the eye or near the limbus. When examined at the slit lamp, pigmented “tracks” are detected, diverging beyond the conjunctival tumor.
As it progresses, it can give rise to new nodes in the conjunctival area, grow into the sclera and orbit, and also metastasize to regional lymph nodes and distant organs. Treatment is surgical. In the early stages, the tumor of the conjunctiva and surrounding tissues are removed; if the sclera grows, the eyeball is enucleated; if the orbit grows, the orbit is exenterated. Radiotherapy and chemotherapy are used. The prognosis in most cases is unfavorable.
Symptoms of the appearance of ocular tumors
Almost all tumors of the organs of vision become noticeable sooner or later. They can appear in the form of growths, thickening, pigmented areas on the skin of the eyelids, swelling, redness in the corner of the eye and around it. On the conjunctiva and cornea they look like a cloudy haze or a round whitish-yellow spot. Choroid tumors are visible as spots on the iris. But the deeper tissues of the eye affected by neoplasms cannot be seen with the naked eye. You may not be aware of them until a drop in vision occurs, pain begins, strabismus and exophthalmos develop (displacement of the eyeball forward (bulging eyes), sometimes with a displacement to the side).
The sooner pathological changes are detected, the greater the chance of completely protecting the Patient’s vision. It is better to proceed to treatment at a stage when the tumor is still small. Therefore, we recommend paying attention to various symptoms, which are not always associated with tumors: lacrimation, dark spots in the field of vision, decreased visual acuity, discomfort in the eye area. And, of course, regular comprehensive vision testing is the best protection against such unpleasant surprises as eye tumors.
Orbital tumors
| Benign | Intermediate | Malignant |
| Coming from bone structures | ||
| — — |
|
| Neurogenic | ||
| Meningioma | Malignant meningioma |
| Coming from soft tissue structures | ||
|
|
|
* Account for up to 25% of all neoplasms of the organ of vision.
Dermoid cyst
Congenital neoplasm. It develops from epithelial cells located subperiosteally at the bone sutures of the orbit, most often in its upper-inner quadrant. Symptoms: local non-inflammatory swelling of the eyelid. Upon palpation, a painless, immobile yellowish formation is determined (contains cholesterol crystals). Surgical treatment is subperiosteal orbitotomy. The prognosis is favorable.
Cholesteatoma (epidermoid cyst)
It develops in mature people under the upper or upper outer wall of the orbit, which is partially lysed. Here, a yellowish mass accumulates subperiosteally. The eyeball moves inward. Exophthalmos gradually develops. Treatment is surgical. The prognosis is favorable.
Cavernous hemangioma
A tumor consisting of dilated vessels surrounded by a pseudocapsule. It is usually of the cavernous type. Symptoms: slowly increasing exophthalmos, the eyeball is not changed, but the retinal veins are tortuous and dilated in the fundus. You can also detect the presence of folds in the vitreous plate of the choroid (the result of tumor pressure on the sclera). In other cases, when the cavernous ganglion is localized at the apex of the orbit, a congestive optic disc or descending atrophy develops. Treatment is surgical. The location and size of the tumor is determined using computed tomography.
Optic nerve glioma
Usually develops in children. Consists of astrocytes, oligodendrocytes and macroglia. It grows slowly. The dura mater of the nerve never grows, but along its trunk it can spread into the cranial cavity. Symptoms: gradually progressive decrease in visual acuity, the appearance of painless axial exophthalmos or with lateral displacement. In the fundus, over time, a picture of a congestive optic disc or its descending atrophy develops. The diagnosis of the disease is made using computed tomography. Treatment is varied: if vision is preserved - radiation therapy, otherwise - surgery. If the tumor does not extend beyond the orbit, then it must be removed along with the eye. When it penetrates into the optic nerve canal, and even further, the intervention plan must be determined by the neurosurgeon.
Optic nerve meningioma
The tumor develops from the villi of the arachnoid membrane of the nerve. It is able to germinate its soft shell and spread to the soft tissues of the orbit. It can also penetrate into the cranial cavity. Symptoms: decreased vision, exophthalmos. The fundus shows a congestive optic disc. Diagnosis is difficult even with CT scans. Treatment is surgical or radiation therapy. The prognosis for vision is unfavorable.
Neuroma
The tumor usually originates from the trunks of certain nerves - ciliary, supratrochlear and supraorbital, passing through the orbital cavity. It is usually located under the superior orbital wall and is delimited by the capsule. Symptoms: non-inflammatory swelling of the upper eyelid with the development of partial ptosis, pain in the affected area. Slightly later appearance of axial exophthalmos or with lateral displacement of the eyeball. In the fundus there is evidence of papilledema. For diagnostic purposes, ultrasound scanning of the orbit and its computed tomography are indicated. Treatment is surgical.
Sarcomas
Aggressive tumors, the source of which can be any tissue of the orbit. They make up at least 25% of malignant tumors of the localization in question. Occurs in people of different age groups. The greatest danger is rhabdomyosarcoma. Most often it is localized in the upper inner quadrant of the orbit and affects the levator muscle of the upper eyelid, as well as the superior rectus muscle of the eye. Symptoms: ptosis, displacement of the eyeball downward and downward outward with limited mobility. Exophthalmos develops quite quickly with congestive dilatation of the episcleral veins. Due to incomplete closure of the eyelids, infiltrates may appear in the cornea. The fundus shows a congestive optic disc. For diagnosis, it is necessary to use the results of ultrasound scanning of the orbit and its computed tomography. Combined treatment: polychemotherapy, followed by external irradiation of the orbit.
Lymphoma
The tumor often develops against the background of autoimmune diseases, immunodeficiency states and leukemia. Consists of lymphoid elements, mainly B-cells, and plasma cells. Develops in people of different ages. Symptoms: sudden appearance of exophthalmos with non-inflammatory swelling of surrounding tissues, sometimes the development of ptosis. In this case, the palpebral fissure is narrowed. Repositioning the eyeball is difficult and then becomes impossible. There is congestion in the fundus. Treatment: external irradiation of the orbit is effective.
Diagnosis and treatment of eye tumors
Typically, an eye tumor can be detected by ophthalmoscopy (examination of the fundus of the eye). To confirm and clarify the diagnosis, stages of examination are carried out
:
- Ultrasound of the eyeball
- CT scan
- Magnetic resonance imaging (MRI)
- Fluorescein angiography
- Tissue biopsy followed by histological analysis.
Modern methods of immunohistochemistry make it possible to accurately determine the nature of the tumor, and tomography - its location.
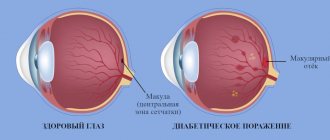
Choroidal tumors
Diagnosis of choroidal tumors is based on the results of ophthalmoscopy, visometry, fluorescein angiography, biomicroscopy, optical coherence tomography (OCT), ultrasound (US) in B-mode. With ophthalmoscopy, nevi look like flat formations up to 0.1 cm in size, raised above the level of surrounding tissues. Depending on the severity of pigmentation, their color varies from grayish to gray-brown. The boundaries are often uneven, but with clear outlines. The unevenness of the contours is caused by adjacent vessels. Nevi that lack pigment are characterized by an oval or round shape with smooth, but less defined contours. Unlike progressive nevi, stationary nevi have drusen on the surface. For their differential diagnosis, ophthalmoscopy with color filters is performed. The red color of the filter makes it possible to visualize this type of choroidal tumor; when green, the pathological formation is not detected.
The fluorescein angiography method in the stationary form reveals a decrease in fluorescence throughout the entire examination. However, no changes are detected in the surrounding choroid. Changes in the choroid are indicated by sweating and a bright glow of the dye. Ophthalmoscopy of uveal melanoma reveals a small nodule with postequatorial localization. Choroidal tumor is yellow-brown or slate in color with drusen on the surface or in surrounding tissues. The OCT method determines the exact location, size, and degree of spread to surrounding tissues. Most patients are diagnosed with decreased visual acuity during visometry.
When performing ophthalmoscopy, a circumscribed hemangioma has the appearance of a small rounded nodule with smooth contours with a diameter of 0.3-1.5 cm. The average thickness of the pathological formation is 0.3-0.4 cm. The color of this form of choroidal tumor is from light gray to dark -red. To differentiate hemangioma from melanoma, fluorescein angiography should be performed. With hemangioma, the average diameter of the tumor vessels corresponds to that of the choroidal vessels, and small foci of hemorrhage may also appear on its surface. Due to progressive angiogenesis in melanoma, newly formed capillaries have a smaller caliber and a more tortuous course. An ultrasound scan of a choroidal tumor detects blood flow and characteristic pulsation of blood vessels, which allows confirming the diagnosis. An external examination is carried out to identify the typical symptoms of strabismus.
Treatment of ocular tumors
Like many serious pathologies, tumors require an integrated approach to treatment. The choice of the necessary methods depends on the diagnosis, the stage of development of the tumor, and the individual characteristics of the Patient. It is important to understand that removing a tumor may not always be sufficient for subsequent health safety. In some cases, regular prevention of its re-development will be necessary.
Methods for removing tumors
:
- Laser evaporation
- Radiosurgical removal using robotic systems
- Cryotherapy (freezing cancer cells with liquid nitrogen)
- Thermotherapy (several sessions of heating tissues up to 45 degrees)
- Brachytherapy (contact radiation technique)
- Photodynamic therapy (destruction of cancer cells by the reaction of their product to light)
- Chemotherapy
- Surgical removal
The need for surgery usually arises only in the later stages of the disease. Until then, treatment may be limited to absolutely safe and minimally invasive techniques (a technique aimed at minimizing the area of intervention in the body and the degree of tissue injury).
The appearance of a neoplasm is a reason for active action, but not for panic. Your attending physician will select a combination of techniques that will achieve the most favorable result for your health. Check your vision regularly, contact a specialist if alarming symptoms appear - and be healthy!