Today, ophthalmologists increasingly use modern electronic devices to diagnose eyes. There is no longer any need to name letters from a special table. There is no need for magnifying glasses to examine the fundus of the eye. Modern devices - autorefractometers - help to study the visual organs in detail. The units will examine the eyes in just a few minutes and provide scan results. The ophthalmologist will only need to decipher the data and prescribe treatment, if necessary.
Types of diseases associated with visual acuity
— Myopia, or myopia, is a visual impairment characterized by poor focusing on objects located in the distance. — Farsightedness, or hypermetropia, is low visual acuity, expressed in “poor visibility” of close objects. — Astigmatism is a disorder of the surface of the eyeball, which leads to inaccurate focusing of objects. Symptoms of myopia and farsightedness appear in childhood. With a high degree of both diseases, both distant and close objects “blur.” Astigmatism also affects visual acuity in children and is often accompanied by myopia or hypermetropia.
The principle of twilight vision
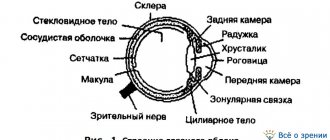
The retina of the eye contains cones and rods, which are responsible for visual acuity in different lighting conditions. Cones help a person see during the day and in bright light; they are responsible for the perception of colors and details. Rods are active mostly in poor lighting; they help us use black-and-white twilight vision.
The rods contain the visual pigment rhodopsin, which is responsible for excitation of the optic nerve. Rhodopsin breaks down in light and is restored in darkness, so a person needs time to adapt when moving from light to darkness.
Twilight vision would be impossible without vitamin A (a component of rhodopsin), since it is involved in the adaptation of the eyes to darkness. Therefore, with a lack of this element, twilight vision disorders develop.
Dark adaptation is the process of transition of the visual system to twilight and night vision modes. In this mode, a person sees in a black and white spectrum, and all objects appear gray to us.
Main causes of vision problems
— Non- compliance with visual hygiene.
Prolonged strain on the eyes and optic nerve, incorrect reading (in poor lighting, in the wrong position).
— Heredity.
-
Lifestyle.
There are a huge number of factors that do not contribute to improving visual acuity.
These include bad habits, poor diet, and low mobility. - Age.
Even people with high visual acuity can develop farsightedness and (less commonly) other problems with age.
More often this happens after 45 years. Age-related deviations in visual acuity are also characteristic of young children whose eyeball has not yet fully formed. - Eye injuries.
Burns, bruises of the eyeball, exposure to a foreign body, hemorrhages in the retina and orbit.
- Other diseases.
Often, vision problems are a symptom or consequence of some chronic disease.
Photos and pictures, where to download and print A4?
It is not difficult to find pictures of letters for a vision test at an ophthalmologist. You can enter the corresponding query in the search engine.
It is advisable to find resources that detail the structure of the table, decipher the data, and provide its versions for other types of diagnostics.
For example, you can visit the sites imbf.org, oftalmologiya.info and sizozh.ru
It’s easy to download the letters for a vision test with an ophthalmologist on any computer. The first resource already has ready-made links through which you can download archives with files to your computer. In the second option, you simply need to enlarge the image to the original size and download it to your hard drive.
Sivtsev’s table is most often downloaded. It includes three parts. This is a special division to make it more convenient to print out letters for vision from an ophthalmologist in A4. In the settings you should select landscape orientation.
Next, the sheets are printed and glued together. You can connect them with simple tape, safety pins, buttons or glue. This creates a sign with letters for the vision test in the original scale.
I see 1, 2 and 3 lines of letters, is that good?
After the indicated actions, the table is fixed on the wall so that the 10th line is at eye level. Position yourself five meters away from her. Provide the table with good lamp or solar lighting. After this, testing can begin.
Check your eyes one at a time. Cover one eye with an opaque flat object—a screen or your palm. Don't close your eyes. For others, read the letters.
Under such conditions, diopters are not calculated. This is due to the lack of special lenses. And there is no guarantee of scrupulous accuracy. This can only be achieved through examination by an ophthalmologist. In the clinic, the examination begins with closing the left eye. A special damper is used here. Thanks to her, the patient does not squint.
The right eye recognizes the letters shown by the doctor. 2-3 seconds are allotted for identification.
If you only see the first three lines well, then that's okay. It all depends on the number of errors in subsequent rows. We accept one error on lines 4-6, and two errors on lines 7-10. If the number of errors is more than normal, the doctor develops treatment measures.
Typically, testing continues until the patient has difficulty recognizing the letters. Then the doctor spends more time to accurately identify in which places the patient does not see the letters. Then, a vision correction device for the second eye is tested in the same way.
If the patient does not see the top row, then:
- He is brought closer to the table. In this case, visual acuity is analyzed based on the distance from which it recognizes the top line.
- The ophthalmologist shows him his fingers, and he must name the quantity and position in space.
- Light perception is checked. The doctor shines a light on the patient and determines whether the patient can see where the light is coming from. If the patient makes a mistake at least once, it means he has a pathology expressed in incorrect projection of light.
If the patient does not recognize the light source and its location, he has zero visual acuity.
What size are the letters on the board?
Maintaining the correct parameters in this procedure is essential to obtain more accurate data.
The letter sizes in the table for testing vision at home must correspond to the following values:
- 7 cm - in the starting line,
- 3.5 cm - in the second,
- 0.7 cm - in tenths.
The size of the letters for a vision test at an ophthalmologist's office is identical. Only today they additionally use special projectors. This allows you to achieve the most accurate results.
Where can I buy such stands and posters?
If you need a board with letters for a vision test, you can purchase it on the Internet, for example, on the deal-med or AlmaMed resource. There are all kinds of tables for different surveys. The average price tag for each table is 300 rubles.
A similar poster is also available in large bookstores.
Our recommendations
To achieve better accuracy in home testing, you should:
- Print the table on white matte paper. The letters should be clear and black, with well-defined edges. If necessary, tint them with a marker.
- Carry out the procedure in good health. You cannot test if you have a fever, headaches, weakness, or after prolonged eye strain. The test is also prohibited after taking certain medications.
- Do not squint your eyes or tilt your head when reading letters.
When conducting home diagnostics without an assistant to point out the rows, write down all recognized letters on paper. Then compare the results with the original source. If you get weak readings, you should contact an ophthalmologist.
Correction of low visual acuity
Vision correction methods include glasses, contact lenses and laser therapy.
- Glasses.
The most ancient and simplest way to prevent the process of vision deterioration.
For people with mild myopia and farsightedness, glasses are prescribed as needed. With severe myopia, glasses become a permanent accessory. - Contact lenses.
The advantage of this method is that the lenses and the eye form an integral optical system, which leads to natural work of the eye muscles.
— Laser therapy.
Allows you to physically change the condition of the eye and prevent more serious diseases.
INSTRUMENTS AND DEVICES FOR STUDYING THE FUNCTION OF THE VISUAL ORGAN
To study the eye and its functions, a significant range of various devices are used, which make it possible to give an objective quantitative assessment of the degree of dysfunction of the visual apparatus. Let us dwell only on those of them that are most widely used in the practice of an eye doctor.
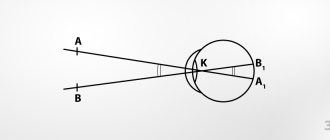
Devices for studying visual acuity. Visual acuity is usually understood as the ability of the eye to distinguish between two points or lines lying close to each other. When, for example, two black stripes on a white background are at a considerable distance from one another, the eye clearly sees the gap between them. As the stripes gradually come closer together, a moment comes when the eye stops seeing this gap and the two stripes merge into one. Conventionally, visual acuity is considered to be 1.00 if the minimum angle between two points at which these points are visible separately is 1' (one minute). To determine visual acuity in an outpatient setting, there are special tables containing rows of black characters on a white background. Most often they use tables with letters and the so-called Landolt rings (Fig. 118, A).
The table is intended for studying visual acuity from a distance of 5 m and contains 12 rows of characters. They correspond to visual acuity 0.1; 0.2; 0.3; 0.4; 0.5; 0.6; 0.7; 0.8; 0.9; 1.0; 1.5 and 2.0. The line width of letters and rings is 1/5 of their size. The table is placed in a plywood frame. It must be well and evenly illuminated, for which it is equipped with a special illuminator, which is an electric reflector with a 40 W electric light bulb, and the body (frame) has mirrored walls. To protect against contamination, the table with the illuminator is covered with special curtains. The device is called “Table Illuminator for Determining Visual Acuity.” It also includes a table with small print that is used when selecting glasses for reading or work related to the need to clearly see close objects. The small table is glazed and equipped with a handle.
In addition to the described tables with an illuminator, the industry produces tabletop instruments for studying visual acuity for distance—POZD-1 and for near vision POSB-1. These devices are transparent: test objects (Landolt rings) are illuminated by lamps from the inside, which ensures constant lighting conditions during the study.
Devices for determining the refraction of the eye. Sets of trial lenses (Fig. 118, B) are used to determine the refraction of the eye and select corrective glasses. The set contains positive and negative lenses of various refractions (usually from 0.25 to 20.0 D), as well as cylindrical glasses and special diaphragms.
The industry produces two types of sets: medium NS-2 and small - NM. The middle set is intended for regional and city hospitals and clinics. It includes 34 pairs of positive and negative non-astigmatic lenses (from 0.25 to 20.0 D), 20 pairs of positive and negative astigmatic lenses (from 0.25 to 6.0 D), 6 paired and 3 single spectacle prisms from 0 .5 to 10.0 prism diopters (pr. diopters). The small set is intended for district hospitals, clinics, outpatient clinics and points for the selection and dispensing of glasses. It contains 32 pairs of non-astigmatic lenses (up to 18.0 D), 12 pairs of astigmatic lenses (up to 4.0 D), 4 paired and 2 single spectacle prisms from 0.5 to 8.0 diopters.
Each set contains a universal frame that makes it possible to center the glasses along the optical axis of the eye, as well as rotate astigmatic glasses when determining refraction in different meridians, an interpupillary distance meter and other accessories.
The sets are produced in a well-finished wooden box, lined inside with velvet or cloth.
Skiascopic rulers (Fig. 118, B) are used to determine the refraction of the eye. They are an aluminum plate with positive or negative lenses built into it. The kit has two rulers with refraction from 1.0 to 9.0 D. A slider with additional lenses 0.5 and 10.0 D moves along the ruler .
The slider should move easily along the ruler and be fixed against each lens using a spring latch so that the optical axes of the slider and ruler lenses coincide.
One of the ends of the ruler ends with a handle for convenient holding of the ruler in your hand. to
determine the refraction of the eye in the range of 0.5-19.0 D. The rulers are produced in two types - with round and rectangular lenses.
Rice. 119. Ophthalmometer OF-3.
An ophthalmometer is used to measure the corneal astigmatism of the eye. They make it possible to measure the radius of curvature of the anterior surface of the cornea and thus determine astigmatism, the value of which is equal to the difference in refractions in two mutually perpendicular meridians (principal sections).
The device is based on determining the distance between reflections on the cornea of two light sources located close to each other. The cornea produces a reduced mirror image of objects in front of the eye, and the greater the curvature of the cornea, the more the image decreases. With astigmatism, the curvature of the cornea in mutually perpendicular meridians is not the same; the sizes of objects and the distance between them will also be different. Using the relationship between refraction and the size of objects, astigmatism is determined, while simultaneously establishing the direction of the two main sections.
Ophthalmometer OF-3 (Fig. 119) consists of a cast base with two stands, on one of which the measuring part of the device is fixed, and on the second there is a chin rest with a forehead rest for fixing the position of the head of the subject. The measuring part has an optical tube, on both sides of which two light sources are located on the arc, producing images on the cornea. These are usually red and green shapes. The device is powered from a 220 V mains voltage.
Perimeters are designed to study the boundaries of vision with a stationary eye. The most advanced is the so-called projection perimeter PRP-60 (Fig. 120 A), which works on the principle of obtaining a light spot on its arc. It consists of a projection head (1) with an electric lamp, a lens and a device for adjusting the size, color and brightness of the mark ; arc onto which the brand image is projected (2); devices for fixing the head of the subject (3); devices for moving the mark along an arc and recording readings on a special graph (4). The light source is a light bulb (8V, 20 W). A step-down transformer is built into the base of the device. The device operates from a mains voltage of 220 V or 127 V at the request of the consumer.
Along with the projection perimeter, a simple tabletop perimeter is produced, in which the fixation objects - marks are metal circles on a rod moved along an arc, painted in different colors.
They produce a tabletop perimeter with a PNR-1 recording device, with the help of which a doctor can relatively quickly record the boundaries of the field of view on a special chart form.
The simplest design is the portable perimeter (Fig. 120, B), which can be easily disassembled and placed in a wooden box.
The described devices serve, as already indicated, to study the functions of the visual apparatus. Along with this, in the practice of an ophthalmologist, various instruments are used to study the anatomical state of the eye (cornea, sclera, eyeball as a whole, pupil, lens, fundus, etc.), as well as the physiological characteristics of the eye, in particular intraocular pressure.
A binocular magnifying glass (Fig. 121, A) is used to better view the eye with some magnification. Magnifier lenses provide 2x magnification. They are built into the body in the form of a visor. The magnifying glass is secured with an adjustable band on the doctor's head. The visor and bands are made of dark plastic.
An ophthalmoscope is used to examine the fundus of the eye. The principle of ophthalmoscopy is that part of the rays entering the eye is reflected by its tissues and comes out back. Collecting them, an image of the fundus is observed.
A mirror ophthalmoscope (Fig. 121, B) is a mirror inserted into a spring holder with a handle. There are two such mirrors: flat and concave. Each of them has a hole in the center with a diameter of 3 mm, through which the doctor makes observations. The device kit includes two magnifiers with a refraction of +13.0 and +20.0 D. All parts of the ophthalmoscope are placed in a soft, portable case that fits easily in your pocket.
The OR-2 manual ophthalmoscope is a more versatile device for examining the eye. In addition to the usual examination of the fundus, this device can be used to perform research in so-called red-free light. When examining an ammetropic eye, it is necessary to use a corrective lens to obtain a sharp picture of the fundus. In an electric ophthalmoscope, this is easily achieved by turning special disks with a set of 23 lenses. The device is equipped with slit and diaphanoscopic attachments, which expands its diagnostic capabilities. Mains power supply via a transformer supplied with the device.
They produce a manual universal ophthalmoscope with a slit lamp and a fiber light guide OVS-01 with an OS-250 illuminator, which gives an ophthalmoscopic picture of increased contrast and allows measurements on the fundus.
A large non-reflex ophthalmoscope is used in inpatient medical institutions. This device is intended for examining the fundus of the eye at high magnification and in the absence of extraneous light reflexes from the cornea and lens of the eye being examined. The device allows you to observe the fundus of the eye monocularly and binocularly (stereoscopically). A very important device included with the device is the refracterometric attachment, which allows you to use an ophthalmoscope to determine the refraction and astigmatism of spectacle glasses in the range from -15.5 to +19.0 D with an accuracy of 0.25 D.
Devices for measuring intraocular pressure. The value of intraocular pressure is a very important indicator in the diagnosis of diseases such as glaucoma, retinal detachment, etc. Various tonometers and elastotonometers are used to measure intraocular pressure.
Tonometers are used to measure intraocular pressure according to Maklakov and for elastotonometry (obtaining an elastotonometric curve) according to Filatov-Kalf.
The Filatov-Kalf tonometer (Fig. 122, A) consists of four Maklakov tonometers weighing 5; 7.5; 10 and 15 g, handle holder, stamp pad, measuring ruler and table-diagram by T. A. Polyak. Each of the tonometers is a nickel-plated cylinder, expanded at the ends, into which milk glass discs with a diameter of 10 mm are inserted. The load moves freely in the cavity of the cylinder, due to which the center of gravity of the tonometer is always at the bottom. The tonometer disk is smeared with paint using a stamp pad and placed on the cornea (the subject must be in a horizontal position). Under the weight of the tonometer, the cornea is slightly flattened, and the diameter of the flattening area depends on the amount of eye pressure. In the flattening area, the paint is erased from the disc and the value of intraocular pressure is judged by the diameter of the discolored circle (measured with a ruler). The obtained data is converted into a pressure unit according to the table-diagram of T. A. Polyak. Based on pressure measurements using four tonometers, an elastotonometric curve is constructed. Determination accuracy is no less than 0.3%. The set is supplied in a wooden case.
The most commonly used set is produced under the name “Maklakov Tonometer”, which contains two tonometer weights weighing 10 g each and a Maklakov table-diagram. The tonometer is equipped with the same accessories: a holder and a pad, placed in a case..
Ophthalmodynamometer (Fig. 122, B) is designed to measure blood pressure in the central retinal artery. It is a spring dynamometer with a scale graduated in millimeters of mercury. The device consists of a rod with a movable end, which is attached to the sclera. The appearance of a pulse in the retinal artery, which characterizes diastolic pressure, is recorded on a dynamometer scale. To measure systolic pressure, continue to increase the pressure on the sclera until the pulse disappears.
Quality indicators of ophthalmological devices. Ophthalmic devices must be carefully finished. All main parts of the devices are coated with black enamel paint, black chrome or blackened. They, as well as other optical instruments, should not contain shiny parts that give off glare. Scales, inscriptions, divisions, numbers must be clear and clear. Eyepieces and lenses must be clean, free of stains, bubbles, streaks, midges, etc. All moving parts must move easily and smoothly.
Laser therapy to improve visual acuity
This type of vision correction refers to non-drug methods of neurometabolic and neuromodulatory orientation.
Increased visual acuity with laser therapy is possible due to the effect on the retina and intracranial parts of the visual analyzer. This causes morphofunctional changes in neurons.
The physiological potential of neurons increases, which is expressed in accelerated conduction of nerve impulses, axonal growth and positive myelination of nerve cells.
Vision correction is carried out using an infrared laser emitter (ICL). The emitter is placed alternately in the temporal and superciliary areas of the eyes when the patient is in a sitting or lying position.
An ICL with an LED power of 0.25 and a frequency of 50 Hz acts on the eye for 5 minutes. The session time decreases with higher emitter power. The correction course is designed for 6 sessions, each of which is carried out every other day.
Functioning of autorefractometers
A modern vision testing device makes it possible to accurately determine the refraction of a patient’s eyes. This device scans using infrared rays. To do this, a person needs to look motionlessly at a certain point for a short period of time. The device will fire a beam of infrared rays through the pupil of the eye. In this case, special sensors will record the radiation frequency appearing at the input and output.
The device not only records scanning results, but also calculates other parameters that are obtained by calculation. In this case, the unit uses the data obtained through the survey. All results are summed up to obtain the device’s conclusion about visual acuity and the condition of the eyes in general.
Features of the autorefractometry procedure
It is very important that the patient does not move his eyes during the examination. It is advisable not to even move your gaze from a specific point. Only in this case can a reliable scanning result be guaranteed. Therefore, the procedure is strictly monitored by an ophthalmologist. After the examination is completed, the device will show the following data:
- refractive features of both eyes;
- the exact distance between the two pupils;
- information about vertex distance;
- data on corneal curvature and radius;
- information about the refractive power of a cylindrical lens.
Thanks to such accurate information, the ophthalmologist will be able to diagnose the patient. The device helps to identify the following diseases of the organs of vision:
- astigmatism,
- farsightedness,
- myopia.