- What is dry eye syndrome?
- What is the ocular surface?
- What is tear film?
- Causes of dry eye syndrome
- At what age does dry eye syndrome most often appear?
- How does dry eye develop and what should you be wary of?
- What signs and symptoms does a patient with dry eye syndrome exhibit?
- Diagnostic examination for dry eye syndrome
- Modern treatment of dry eye syndrome
- Video about dry eye syndrome
- Cost of treatment for dry eye syndrome
Dry Eye Syndrome (DES) is currently one of the pressing problems in ophthalmology. According to WHO, more than 350 million people worldwide suffer from this pathology.
In Russia, Dry Eye Syndrome affects 26% to 31% of the adult population. This disease is most often detected in people over 40 years of age. And in women during menopause it occurs in 90% of cases.
What is dry eye?
Dry Eye syndrome is a chronic polyetiological disease of the ocular surface, developing as a result of a disorder in the tear-producing system of the eye, leading to disruption of the stability and hyperosmolarity of the tear film, and manifested by a complex of symptoms of drying of the surface of the cornea and conjunctiva.
Symptoms of drying out (xerosis) include burning, itching, sandy or foreign body sensation, photophobia, pain, difficulty opening the eyes spontaneously in the morning, decreased clarity and blurred vision.
It is important to know! Dry eye disease not only leads to discomfort in the eyes, but also reduced performance and a sharp deterioration in the quality of life of patients; moreover, it contributes to the development of secondary eye diseases, including disability.
Dry eyes after surgery: what to do?
Table of contents
How does the tear film work?
Causes of dry eye after surgery Symptoms and diagnosis of dry eye after surgery Treatment of dry eye after surgery Gilan solution for eliminating dry eyes One of the main conditions for good vision is a stable tear film, but it is this film that is primarily affected during surgery. This is why dry eye syndrome occurs to one degree or another in all patients who have undergone eye surgery.
How does modern medicine solve this problem? What measures can be taken to ensure that postoperative eye rehabilitation goes without complications? The article will discuss cataract surgery.
How does the tear film work?
The tear film simultaneously performs several functions: protects against microbes, ensures metabolism, and moisturizes the surface of the eye. The latter is the most important, since the moisturizing film is one of the components in the complex mechanism of human vision.
The eyes see well when the tear film is evenly renewed, thereby ensuring constant hydration of the surface of the cornea.
Causes of dry eye after surgery
If the structure and composition of the tear film changes, for example, due to disruption of the lacrimal glands, the use of drops, damage to the cornea during the formation of the incision, which are inevitable during cataract operations, dry eye syndrome develops.
Not only microtraumas of blood vessels and nerves, but also local and systemic medications can affect the stability of the film. The risk of inflammation as a consequence of dry eye symptoms is higher in the following groups of patients:
- suffered from this disease before the operation;
- underwent blepharoplasty;
- patients with chronic blepharitis.
Symptoms and diagnosis of dry eye after surgery
After cataract removal, most patients experience irritation and dry eyes, foreign body sensation, blurred vision, itching, burning sensation, that is, classic symptoms of dry eye.
For diagnosis, it is enough to conduct a fluorescein test to determine the time of tear film rupture. Normally, it should occur no earlier than 10 seconds after blinking. If the indicator is different, you need to undergo a course of treatment to restore the regulation of tear fluid.
Treatment of dry eye after surgery
When choosing tactics and treatments for dry eyes, the doctor is guided by test results, since the patient’s sensations do not always objectively reflect the real clinical picture.
Under no circumstances should you self-medicate! Most drugs used to treat inflammation and dry eye syndrome cause complications if the dosage or duration of use is violated. Some products help to consolidate the effect of the operation, but dry eyes will not cure.
The main emphasis is on maintaining tear production safely (without side effects). In case of irritation and inflammation, its composition is unstable, therefore, “artificial tear” preparations based on hyaluronic acid are recognized as the optimal means of providing a stabilizing effect. This natural substance qualitatively improves the structure of the tear film and helps restore natural functions.
Gilan solution to eliminate dry eyes
The drug "Gilan" is a multifunctional solution based on hyaluronic acid. Helps painlessly and without complications eliminate postoperative eye inflammation and other manifestations of dry eye syndrome.
Gilan can be used by pregnant women and children, when wearing soft contact lenses and during flights. To reduce the risk of exacerbation of the syndrome, it is recommended to use the solution before cataract surgery.
What is the ocular surface?
The ocular surface is a complex biological structure, including the surface layer of epithelial cells of the cornea, conjunctiva, nasolacrimal outflow system, as well as a secretory apparatus consisting of a complex of multidisciplinary glands and secretory cells that produce components of the tear film, which is an integral part of the ocular surface.
The ocular surface includes the glands of Meibom, the glands of Moll and Zeiss, which produce lipid secretion for the tear film, as well as the secretory glands of Wolfring and Krause, which provide the basal (main) production of fluid for the formation of the aqueous layer of the tear film. In addition, the secretory system of the ocular surface includes Goblet cells, Manz cells, the crypt of Henle and Becher goblet cells, which produce mucin, forming the layer of the same name.
In addition to these structures, the ocular surface includes the hair follicles of the eyelashes and the edges of the eyelids.
What is the tear film and why is it necessary?
The tear film is a liquid, constantly renewed biostructure, which is part of the ocular surface, covers the cornea and performs important functions for the life of the eyes: optical, protective, immune, respiratory and nutritional.
The tear film is necessary for the proper, full functioning of the eyeball. Structurally, it is heterogeneous and consists of three layers. The tear film also has a very complex chemical composition, including water, numerous nutrients and special protective substances, all the necessary and balanced components for the normal functioning of the anterior surface of the eye. It also provides support for local immunity, antibacterial and respiratory functions. The tear film, leveling the surface of the cornea, provides its optical function and is a refractive medium, while having on its surface at the border with the air the highest refractive power of the order of 60D. In this regard, even minor disturbances in the tear film can greatly reduce visual acuity.
The amount of basic tear secretion per day is up to 2 ml, while the tear film has nothing in common with the tear produced by the lacrimal gland in a reflex state.
Need to know! The lacrimal gland provides only reflex lacrimation only for a protective purpose in response to physical or other irritation of reflexogenic zones (foreign body, volatile chemicals, thermal effects), as well as due to a psycho-emotional response.
The lacrimal gland is capable of secreting up to 30 ml of tears per minute, depending on the intensity of the irritating agent. Its secretion has a higher osmolarity and therefore moderately irritates the ocular surface and cannot replace the tear film.
Mucin layer of the tear film
The mucin layer is produced by goblet and granule cells, glands of Manz (limb) and crypts of Henle.
A gel consisting of mucin forms a smooth surface of the epithelium, facilitates the sliding of the eyelids along the cornea, cleanses and moisturizes the epithelium, and imparts hydrophilic properties to the epithelium.
The mucin layer makes up only 0.5% of the total thickness of the tear film. Its main task is to impart hydrophilic properties and adhesive ability to the primarily hydrophobic corneal epithelium. It is for this reason that the tear is held quite firmly on the cornea. In addition, mucin smoothes out all micro-irregularities of the epithelial surface and gives the cornea its characteristic mirror shine.
Aqueous layer of the tear film
The aqueous layer is the most prominent, produced primarily by the tear glands (95% of the aqueous component of the tear film), with the additional glands of Krause and Wolfring producing the remaining 5%. The aqueous layer consists of water-soluble electrolytes and organic low-molecular and high-molecular substances. Continuously updating, this layer ensures, on the one hand, the delivery of oxygen and nutrients to the epithelium of the cornea and conjunctiva, and on the other, the removal of carbon dioxide, metabolic products and exfoliated epithelial cells.
Lipid layer of the tear film
The lipid layer is produced by the Meibom glands located in the upper and lower eyelids. Normal meibomian gland secretion is formed from unsaturated fats, and its oleic acid content determines its melting point. When the amount of oleic acid decreases, the secretion hardens (compacts) due to an increase in the melting point of lipids and normal body temperature becomes insufficient to maintain lipids in a liquid state. Under the influence of body temperature, the meibomian glands become denser, causing secondary blockage of the excretory ducts, which leads to inflammation. The lipid layer prevents excess evaporation of the aqueous layer and gives the outer surface of the tear film a smooth appearance.
Physiology of tear production and functioning of the tear film in healthy people
Description
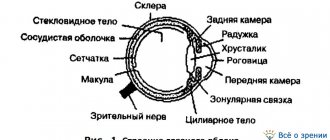
The fluid located in the conjunctival cavity and constantly moisturizing the surface of the epithelium of the cornea and conjunctiva has a complex composition, including the secretion of a number of glands (main and accessory lacrimal, meibomian, Zeiss and Moll), as well as glandular cells of the conjunctiva (Fig. 1).
Of the latter, Becher's goblet cells are of greatest importance, the localization of which in various parts of the conjunctiva is schematically presented in Fig. 2. In addition, some other substances from the blood plasma pass through the capillary wall into the conjunctival cavity. It is this “prefabricated” moisture that is usually called tears or tear fluid (FL).
It is currently known that the main lacrimal gland provides only reflex lacrimation, which occurs in response to mechanical or other irritation of reflexogenic zones.
It is also stimulated by emotions, sometimes reaching 30 ml per minute in such cases. At the same time, the constant, so-called main secretion of tears occurs exclusively due to the functioning of the accessory lacrimal glands of the conjunctiva of Krause and Wolfring and is only 0.6-1.4 μl/min (up to 2 ml per day), gradually decreasing with age. The conjunctival cavity of a healthy person constantly contains about 6-7. µl SG. When the eyelids are closed, the tear completely fills the capillary gap between the walls of the conjunctival sac. When the palpebral fissure is open, the configuration of the distribution of fluid changes due to its additional coverage of open areas of the cornea and conjunctiva with the formation of the so-called tear film (TF) (Fig. 3). The latter, throughout the contact of the edges of the eyelids with the eyeball, forms tear menisci (upper and lower) with a total volume of up to 5.0 μl.
According to N. Ehlers (1965), the thickness of the SP varies, depending on the width of the palpebral fissure, from 6 to 12 μm. It has been established that it performs a number of important physiological functions: moisturizes the epithelium of the cornea and conjunctiva, ensures its metabolism, protects against certain exogenous influences and, in addition, serves as a refractive optical medium.
Structurally, the SP is heterogeneous and includes visual layers: mucin (covers the corneal and conjunctival epithelium), aqueous and lipid (Fig. 4). Each of them has its own morphological and functional characteristics.
The mucin layer is quite thin (0.02-0.05 µm) and makes up only 0.5% of the entire thickness of the SP. Its main function is to impart properties to the primarily hydrophobic cornea, making the SP quite mute. In addition, mucin adsorbed on the corneal epithelium smoothes out all micro-irregularities of the epithelial surface, providing its characteristic mirror-like shine. However, it is quickly lost if for some reason the production of mucins decreases.
The second, aqueous layer of the SP, has a thickness of about 7 microns (98% of its cross section) and consists of water-soluble electrolytes and organic low- and high-molecular substances. Among the latter, water-soluble mucoproteins deserve special attention, the concentration of which is maximum in the mucin layer of the SP. The “OH” groups present in their molecules form so-called “hydrogen bridges” with dipole water molecules, due to which the latter are retained by the mucin layer of the joint venture.
The continuously renewed aqueous layer of the SP ensures both the delivery of oxygen and nutrients to the epithelium of the cornea and conjunctiva, and the removal of carbon dioxide, “slag” metabolites, as well as dying and exfoliating epithelial cells. The enzymes, electrolytes, biologically active substances present in the liquid, components of nonspecific resistance and immunological tolerance of the body, and even leukocytes determine a number of its specific biological functions.
On the outside, the aqueous layer of the joint venture is covered with a rather thin (0.004-0.4 µm) lipid film. Theoretically, it can perform its functions already in a monomolecular layer. However, as established, the layers of lipid molecules, through the blinking movements of the eyelids, either become thinner, spreading throughout the entire conjunctival cavity, or layer on top of each other and, with a half-closed palpebral fissure, form a “common shutter” of 50-100 molecular layers 25-500 nm thick.
The lipids that make up part of the SP are secreted by the meibomian glands, and also, possibly, by the glandular cells of Zeiss and Moll, located on the free edges of the eyelids. The lipid portion of the tear film performs a number of important functions. Thus, its surface facing the air, due to its pronounced hydrophobicity, serves as a reliable barrier to various aerosols, including infectious ones.
In addition, lipids prevent excessive evaporation of the aqueous layer of the joint venture, as well as heat transfer from the surface of the epithelium of the cornea and conjunctiva. And finally, the lipid layer imparts smoothness to the outer surface of the SP, thereby creating the conditions for the correct refraction of light rays by this optical medium.
It is known that the refractive index of SP is 1.33 (cornea -1.376). As a number of studies have shown, the SP is constantly updated, and this process is of a natural nature in terms of time and quantitative parameters. So, according to 1980 data, for only 1 minute. About 15% of the entire joint venture is renewed. Another 7.8% of it evaporates during the same time due to heating by the cornea (1 = +35.0 ° C with closed eyelids and +30 ° C with open eyelids) and air movement.
E.Holly (1973-1987) and others. They established that the basis for the renewal of the SP is periodic violations of its integrity (stability), which leads to fragmentary exposure of the epithelial membrane and, as a result, to the stimulation of blinking movements of the eyelids. Unmoistened areas of the epithelial membrane (so-called “dry spots”) that appear as a result of rupture of the joint joint, according to N. Ehlers (1965), PNDilly (1985) and others, stimulate the blink reflex.
When blinking, the posterior ribs of the eyelid edge, sliding along the anterior surface of the cornea, like a windshield wiper, “smooth out” the joint and shift all exfoliated cells and other inclusions into the lower tear meniscus, due to the fact that when blinking, the outer edges of the eyelids first come into contact and only lastly the inner ones. , the tear is displaced by them towards the tear lake (Fig. 5). True, some authors also explain this direction of tear flow by flickering of the microvilli of the conjunctival and, possibly, corneal epithelium.
During blinking movements of the eyelids, the so-called “pumping” function of the lacrimal canaliculi, which drain the fluid into the lacrimal sac. It has been established that, on average, one blink cycle processes from one to two microliters of fluid, that is, up to 30 μl of tears in one minute. According to most authors, tear production occurs continuously during the daytime.
According to FJHolly (1973), rupture of the joint occurs due to the evaporation of liquid from its outer surface. Although this process is inhibited by the lipid layer, the joint venture becomes thinner, and its surface tension increases. As a result, the joint ruptures in the described area, forming an unwetted “spot” on the outer membrane of the epithelium (Fig. 6).
Microscopic “crater-like” defects that periodically appear on the epithelial membrane of the cornea are also important. The latter arise as a result of the physiological renewal of the epithelium of the cornea and conjunctiva, that is, due to its constant desquamation.
As a result, the place where the surface hydrophobic membrane of the epithelium is defective, exposing the deep hydrophilic layers underlying this membrane, is instantly filled with a watery layer of the tear film that “tears” here. This mechanism of SP ruptures is confirmed by observations that they often occur in the same places. Often in such cases, microbulls and microerosions of the corneal epithelium are found in the same areas, which are then stained with a sodium fluorescein solution.
The considered circumstances relate to tear production and the functioning of the joint system in healthy people. Disturbances in these processes underlie the pathogenesis of the so-called dry eye syndrome (DES), which is the subject of the following sections of the manual.
Causes of Dry Eye Syndrome (DES)
The causes of dry eye syndrome are varied and can be divided into two large groups - endogenous and exogenous.
Endogenous causes include the presence of a certain pathology in the patient, including autoimmune, such as Sjogren's syndrome, or these may be normal physiological changes corresponding to age. Also, the causes of its occurrence may be associated with taking certain types of medications, pathological hormonal disorders, as well as the consequences of inflammation of the anterior segment of the eye and various damage to it, including after surgical treatment such as, for example, after blepharoplasty, refractive laser operations.
Exogenous causes of dry eye syndrome include household and professional causes. The most common causes include environmental pollution, excessive exposure to air conditioning, and using video screens for long periods of time. When a person works for a long time with gadgets, computers and actively fixes the picture on the monitor, he may not blink for more than a minute. This has a detrimental effect on the condition of the tear film, leading to its rapid rupture, less frequent renewal and, accordingly, increased drying of the ocular surface.
Dry eye syndrome often develops during pregnancy, when physiological and hormonal changes occur in a woman's body. A special category of causes includes in vitro fertilization, which is accompanied by serious hormonal changes, which also causes the development of dry eye syndrome.
Regarding the occurrence of dry eye syndrome in women in general, the most discussed cause of dry eye syndrome is undoubtedly menopause - a condition in which the detection of dry eye syndrome reaches 90%. However, this does not make the syndrome a prerogative of women; on the contrary, dry eyes, although to a lesser extent, occur quite often in men, especially for smokers or those who live in areas with particularly high air pollution.
Among the less discussed exogenous causes are also seasonal allergies, which lead to intense and constant stress in the respiratory tract with subsequent irritation of the mucous membranes, including the eyes. Many allergies tend to last for months, causing a persistent inflammatory condition that gradually worsens and stimulates an immune system response that can eventually alter the tear film.
A separate list of medications, long-term use of which provokes the development of dry eye syndrome, should be provided:
- drugs that lower blood pressure: β-blockers;
- adrenomimetic substances;
- antiarrhythmic drugs;
- antidepressants;
- drugs for the treatment of peptic ulcers (anticholinergics);
- tranquilizers;
- antihistamines;
- oral contraceptives.
It should be noted that dry eye syndrome can also be stimulated by certain eye drops with long-term use: antiglaucoma drops, anticholinergics, glucocorticosteroids, as well as drugs containing certain preservatives.
Risk factors
- General somatic pathology;
- Autoimmune pathology (Sjögren's syndrome);
- Diseases that disrupt metabolism;
- Hormonal changes, menopause;
- In vitro fertilization;
- Excessive use of cosmetics, eye and eye creams;
- Eyelash extensions;
- Use of contact lenses;
- Chronic blepharitis, conjunctivitis;
- Long-term use of antiglaucoma drugs;
- Complications after blepharoplasty;
- Previously performed laser vision correction;
- Age-related changes (from 40-50 years);
- Prolonged work in front of monitor screens;
- Long-term use of systemic drugs;
- Contaminated air;
- Smoke, including from cigarettes, smog;
- Long stays in rooms with air conditioning and heat radiators.
- Stress;
- Smoking;
- Excessive alcohol consumption.
Dry eye syndrome
1. Itching. Patients with dry eye syndrome experience increased sensitivity and irritability of the cornea. This leads to itching. Allergic reactions are also a common cause of burning and itching in the eyes. These conditions are treated with antihistamines, one of the side effects of which is dry eye syndrome.
2. Burning sensation. One of the functions of the tear film is to wet the surface of the cornea. When the integrity of the film is damaged, the cornea, which contains a large number of nerve endings, dries out and begins to send impulses to the brain, which it recognizes as a burning sensation.
3. Foreign body sensation. One of the characteristic symptoms is a feeling as if a grain of sand or other object has gotten into the eye. Such sensations occur when the eyeball is not sufficiently hydrated. When such signals appear, the brain begins to send response impulses to the eye, causing it to produce more fluid to wash away the foreign object.
4. Redness. Redness is a sign of inflammation. When the eye is not sufficiently hydrated, it becomes susceptible to inflammatory diseases. The functions of tears include the transport of nutrients to the tissues of the eye. If transport is impaired, the eyes react to this condition with inflammation.
5. Blurred vision that disappears when blinking. Tears provide a smooth outer optical layer for incoming light rays. As the surface of the eye dries, the surface becomes uneven, causing blurred images. When you blink, the tear film is renewed, and a smooth optical layer again appears on the surface of the eye, ensuring the correct perception of light waves.
6. Watery eyes. Most patients who experience excessive tearing are perplexed when they are diagnosed with dry eye syndrome. In this case, the system responsible for the production of tear fluid works in an enhanced mode precisely because of dry eyes. Increased lacrimation can also be a reflex in response to the sensation of a foreign body, which was described above.
7. Increased discomfort after reading or watching TV. Blinking rate decreases significantly when a person is concentrating on a specific task. Since when blinking, the tear film on the surface of the cornea is renewed, a decrease in the frequency of blinking will lead to increased dryness of the eyes.
At what age does dry eye syndrome most often appear?
Dry eye syndrome can be detected in patients at almost any age. But most often it is diagnosed in patients over 40-50 years old. However, due to environmental changes, the widespread use of technology at work and at home, and the increasing use of contact lenses, the age of patients with detectable dry eye syndrome is becoming younger.
You need to understand! If everyday life is associated with the constant presence of risks or taking medications, the side effects of which disrupt the secretory function of the glands, then regular monitoring by an ophthalmologist is necessary in order to timely correct and take the necessary measures.
How does dry eye develop and what should you be wary of?
The development of dry eye syndrome is based on the processes of disruption of the secretory function of the glands of the ocular surface and, as a consequence, the formation and renewal of the tear film. These violations can be varied and affect different parts.
In the first place among them are problems with the production of tear film components (aqueous layer, mucins, lipids) due to dysfunction of the corresponding glands. As a result, the composition of the tear film changes and the evaporation of tears increases, resulting in corresponding symptoms.
An increase in the evaporation of the tear film can also cause a change in the anatomical structure in case of pathology of the adnexal apparatus of the eye - ectropion, entropion, lagophthalmos, deformation of the edges of the eyelids and, as a result, a violation of the smoothness and congruence of the ocular surface, as well as after some surgical interventions that reduce innervation and trophism of the cornea. A special place is occupied by operations on the eyelids - aesthetic blepharoplasty, performed by plastic surgeons with insufficient knowledge about the adnexal apparatus of the eye or taking patients for surgery without consulting an ophthalmologist.
Of course, we should not forget about the physiological decrease in tear secretion that occurs with age.
Against the background of impaired stability of the tear film, pathological changes in the ocular surface gradually develop and signs appear, and then characteristic complaints that cause discomfort and certain symptoms in the patient.
It is important to understand! In the initial stages of dry eye syndrome, there may be no obvious external clinical symptoms or ocular manifestations, but the level of corresponding signs in the patient is usually high.
At this stage, a timely professional approach and accurate specialized diagnostics are important in order to identify dry eye syndrome in its early stages and begin pathogenetic treatment.
If no therapeutic action is taken, the disease will inevitably progress, damage to the ocular surface will be significant and will lead to the appearance of obvious clinical symptoms and manifestations.
At this stage of development of dry eye syndrome, a more complex and comprehensive approach to treatment is required, but even then, it is not always possible to achieve complete recovery.
Inflammation and Dry Eye Syndrome
Inflammation is an integral component in the development of dry eye syndrome. Pathogenetically, inflammation is always one of the main reactions of the body to any damage to its tissues. Accordingly, this is also inherent in the ocular surface. With the development of a pathological process and its transition to a chronic form, inflammation plays a key role, as a result of which damage to the ocular surface becomes more serious. Consequently, the inflammatory process is an important mechanism in the development of the disease and plays a large role in the progression of the pathological condition, which must be taken into account in its complex therapy.
What signs and symptoms does a patient with dry eye syndrome exhibit?
Main signs of Dry Eye Syndrome
Even before the formation of any clinical manifestations and symptoms of dry eye syndrome, patients experience various subtle signs, which are often not given due attention and, moreover, are not always associated with eye disease. Also, these signs do not prompt patients to seek professional ophthalmological help. However, in conversations with their friends and acquaintances, patients often note fatigue, heaviness in the eyes, rapid fatigue when working with a computer or simply when reading, and also note periodic blurred vision. These precursors are subjective signs of the presence of serious problems in the ocular surface and mark the beginning of the development of dry eye syndrome.
Main symptoms of Dry Eye Syndrome
During the course of the disease, pathological changes occur in the tissues of the ocular surface, which leads to the formation and occurrence of persistent symptoms and characteristic complaints of varying degrees of intensity. At first, they simply periodically distract the patient’s attention, but, gradually intensifying in accordance with the course of the disease, they become a real painful, debilitating obstacle in everyday life.
Common symptoms include:
- tension and feeling of heaviness in the eyes;
- redness;
- itchy feeling;
- feeling of sand;
- sensation of a foreign body inside the eye;
- burning;
- decreased visual acuity (temporary or permanent);
- discomfort in front of intense light sources (photophobia);
- feeling of increased eye fatigue;
- double vision;
- pain (in severe cases).
These symptoms can worsen, creating serious difficulties in daily life, and also affect the psycho-emotional state of patients.
Symptoms of dry eye syndrome:
- The appearance of a persistent sensation of a foreign body in the eye
- Burning sensation and pain in the eyes
- Feeling of dry eye
- Painful reaction to eye drops
- Deterioration of vision in the evening
- Intolerance to wind, sun, tobacco smoke
It is very important to identify the exact cause of the disease in order for a complete recovery to occur. If you have discovered any of the above symptoms, which have been observed for a long time, then you should not endure visual discomfort, but you should consult an ophthalmologist. Sometimes dry eye syndrome can be a consequence of other serious diseases (diabetes mellitus, malignant neoplasms and skin diseases).
Diagnostic examination for dry eye syndrome
Diagnostics
Diagnosis of dry eye syndrome should be carried out in a specialized ophthalmological clinic and include a number of professional tests, as well as specific diagnostic studies, based on the results of which the stage of dry eye syndrome is verified and determined. After this, the ophthalmologist prescribes the necessary physiotherapy and medication, as well as laser or surgical treatment individually for each patient.
In recent years, thanks to scientific research and the development of new devices, it has become possible to introduce into everyday ophthalmological practice a number of accurate diagnostic tests using the latest devices, which are indispensable in the diagnosis of dry eye syndrome and the proper correct assessment of the condition of dry eye syndrome.
Our clinic is equipped with professional equipment for specialized diagnostics for dry eye syndrome, which we use every day in our work to establish a diagnosis and monitor the therapy used.
Specialized diagnostic techniques for dry eye syndrome
It is impossible to assess the state of the secretory function of the ocular surface without diagnostic studies and specialized tests, on the basis of which modern diagnosis of dry eye syndrome is currently not possible. Among them are the main ones:
Digitized biomicroscopy
This is a diagnostic study that involves the study and subsequent clinical assessment of the anterior structures of the eye and eyelids using a slit lamp with an effective optical and computer system of digitized images at maximum resolution. Also, during the study, additional staining of the tear film, conjunctiva and cornea is carried out, which makes it possible to assess the severity of changes in the ocular surface and identify the presence of abnormalities in the tear film and secreting glands.
Meibography
This is a necessary and very important diagnostic study, which allows us to evaluate the morphology of the meibomian glands, which produce lipid secretions for the full formation of the tear film. In our clinic we perform this study using a special Me-Check device (Italy) for photomeibography. The device allows you to determine the state of functioning of the meibomian glands and set the degree of their dysfunction from 0 to 4 on the Meyboscale by Dr. Heiko Pult in a few minutes without additional devices and contrast agents. This study is also carried out at the stages of treatment in order to determine the effectiveness of the therapy used.
Interferometry of the tear film
It is an important diagnostic method for studying primarily the tear film, its quantity, composition and distribution, as well as the quality of tears. This technology also allows the assessment and study of the lipid layer of the tear film and its formation and distribution, providing extremely detailed images of the tear. The procedure is non-invasive and lasts less than five minutes. Before undergoing the interferometer test, patients are advised to remove contact lenses at least 48 hours in advance, not to use oil-based cosmetics around the eyes, and not to rub their eyes before the test.
Tear Film Osmolarity Test
This test is necessary to determine the total concentration of all dissolved particles in the patient's tear film. This is a very precise threshold value, which is 316 mOsm/L. By analyzing a sample of the patient's tear film using a special osmometer, we can identify not just deviations in the level of osmolarity, but in fact, disturbances in the body's ability to regulate the homeostasis of the tear film, which is the basis for the pathogenesis of the development of dry eye syndrome. Accordingly, the higher the osmolarity, the more concentrated the tear is and the more it can cause damage to the ocular surface.
The I-PEN® Tear Osmolarity System is a diagnostic device for quantitatively measuring the osmolarity (concentration of dissolved salts) of tears in normal and ocular patients.
Otto Schirmer test, or quantitative assessment of tear production
This diagnostic test allows you to determine the quantitative function of the secretory apparatus of the anterior surface of the eye, which is necessary for its proper hydration. The test is carried out within 5 minutes. The normal secretion rate is at least 15 mm of the test strip. The test is carried out both with the use of an anesthetic (to determine the basic secretion) and without (to determine the reflex and basic secretion).
Lipcof test
This test is quite informative for diagnosing dry eye syndrome. Over time, with dry eye syndrome, friction occurs between the eyelids and the surface of the eye, due to which the tension of the conjunctiva decreases and its folds are formed parallel to the eyelids, depending on the number and severity of which the severity of this symptom is assessed.
Norn's Test
This is a diagnostic test of tear dysfunction in which the breakup time of the tear film is determined after fluorescein staining to assess the quality and stability of the tear film in a blue filter at the slit lamp. If the patient being examined is in the age group from 16 to 35 years, then the normal time for the tear film to break up for him will be 21 seconds after the last blink. With age, this time decreases. For example, if the patient's age ranges from 60 to 80 years, then a tear film breakup time of 11-12 seconds would be considered normal.
Meniscometry
It occupies a special place in the diagnosis of dry eye syndrome. This is a measurement of the tear meniscus (tear rivulet) between the surface of the conjunctiva, the cornea of the eye and the edge of the lower eyelid. Its height is on average 0.4 mm. Changing its height has important diagnostic significance. Measuring the radius of curvature of the tear meniscus can be helpful in diagnosing dry eyes.
Test to determine the presence of inflammation
InflammaDry test is very convenient to use. This test examines a small sample of the patient's tears taken from the conjunctival fornix of the lower eyelid. This test detects increased levels of MMP-9 (matrix metalloproteinase-9) protein. This inflammatory marker in the tear film of patients provides tremendous information about the presence of inflammation of the ocular surface. In most cases, inflammation is present before clinical symptoms of the disease appear, so identifying dry eye disease at the preclinical stage using this test will allow it to be treated at an earlier stage. This test is also indicated before any ophthalmological operations in order to avoid complications in the postoperative period, as well as increase the safety of the rehabilitation period.
What additional studies and tests are prescribed for dry eye syndrome?
The mandatory complex when examining patients with dry eye syndrome includes examination of other parts of the eye to exclude the presence of concomitant pathologies. Among these studies, we can note some general clinical tests that need to be prescribed to patients.
In some cases, tests may need to be ordered, such as a test that measures an iron-binding protein called lactoferrin. The amount of this molecule is closely related to tear production. Patients with dry eye syndrome have low levels of this protein. This analysis may be especially valuable for such patients, since this is one of the areas of pathogenetic treatment. It is also valuable to evaluate tears for the content of lysozyme, an enzyme that is usually found in tears.
Another necessary item is tests for a number of hormones. These are thyroid hormones, male and female sex hormones, as well as some others. Many studies have been conducted that have proven the relationship between the condition of the tear film and the hormonal status of the patient.
Schrimer's test
The Schrimer test is based on reflex stimulation of tear fluid production, as well as the absorbency of filter paper, which is placed in the conjunctival cavity.
The purpose of the study is to determine the amount of tears that are produced over a certain time.
The Schrimer test cannot be performed in case of an ulcer or fistula of the cornea, extensive erosion of its surface, or in case of perforation of the eyeball.
Methodology
To carry out the test, you must use special filter paper strips. They can be produced in a set or you need to make them yourself (length 40 mm, width 5 mm). The end of the strip at a distance of 5 mm from the edge is bent at an angle of 40-450. Next, the patient is asked to look up, and this curved tip is placed under the lower eyelid of the eye (in the outer third). It is necessary that the edge of the strip touches the bottom of the lower fornix of the conjunctiva, then the bend will be located at the level of the edge of the eyelid. It is advisable to carry out the test on both sides simultaneously.
After administering the strips, the doctor should start the stopwatch and the patient closes his eyes. After exactly five minutes, the strips are removed and the length of the wet part is measured, starting from the point of inflection. If the wetting boundary cannot be established, the strips can be illuminated. When the wet boundary is located obliquely, the average result is taken into account.
Interpretation of results
In healthy patients, 15 mm test strips are wetted for 5 minutes. With a decrease in tear production, the length of the wetted test strip decreases; with hypersecretion of tear fluid, on the contrary, it lengthens significantly, reaching 35 mm within 2-3 minutes. The Schrimer test does not exclude a decrease in the main tear production, which can be masked for a long time by its reflex increase.
Modern treatment of dry eye syndrome
Dry eye syndrome is a complex, polyetiological disease of the ocular surface, in which today there is no single effective drug that can influence all the mechanisms of occurrence of this disease, as well as achieve a positive therapeutic effect on all damage to the ocular surface caused by dry eye and restore its secretory functions .
Today in modern medicine there are various approaches and methods for the treatment of dry eye syndrome, in which restoration of the secretory function of the glands that produce components of the tear film, and, consequently, the volume of tears sufficient to moisturize the ocular surface becomes only part of a multi-stage approach in the pathogenetic therapy of dry eye syndrome. Such complex treatment is aimed at all stages involved in the pathogenesis of the development of this disease. And in addition to general healthy lifestyle measures aimed at improving the health of the entire body as a whole (replenishing water-salt balance, correcting nutrition and normalizing sleep-wake patterns), and aimed at minimizing the impact of environmental conditions, the following are distinguished:
Reparative therapy
Aimed at eliminating damage to the ocular surface resulting from insufficient hydration due to changes in the composition of the tear film.
In this case, the use of reparative drugs is indicated, aimed primarily at the regeneration of damaged areas. Among them, gel-based preparations and ointment forms are most often used (Korneregel, Vidisik, Parin Pos and others).
Need to know! Drug therapy for dry eye syndrome is used only in combination with other therapeutic measures and should be under medical supervision from the moment of prescription until the drug is discontinued once a therapeutic effect is achieved.
Tear replacement therapy
Aimed at temporary or permanent replacement of the missing tear volume and prevents premature rupture of the tear film on the ocular surface. Currently, there are more than 40 types of various tear replacement drugs on the pharmaceutical market, most of them are based on hyaluronic acid. The latest generations of artificial tears are well tolerated by patients due to the absence of preservatives, and their moisturizing effect is maximum and comfortable. In our practice, the drugs of choice include Hilo-komod, Artelak Splash, Gilan Comfort, Vizmed.
You need to understand! The choice of drugs is determined only by the doctor, depending on the clinical manifestations and diagnostic results in balance and mode with other types of drug and physiotherapeutic treatment.
Tear conserving therapy
It is aimed at preserving one’s own tears by retaining its volume on the ocular surface through obturation of the lacrimal openings (with polymer obturators or using laser or surgical intervention).
This technique is used either when medication is ineffective and as a supplement to it, as well as to eliminate the need for excessively frequent (over 6 times a day) instillation of tear substitutes. Installation of special occluders in the lacrimal openings is carried out by an ophthalmologist. There are occluders that dissolve on their own after some time and do not require removal.
Need to know! Reparative, tear replacement and tear preserving therapy belong to the group of symptomatic treatment methods; they can only compensate for the signs and superficial manifestations of dry eye syndrome and do not pursue the goal of a pathogenetic cure for the existing problem.
Anti-inflammatory therapy
It is aimed at reducing the inflammatory factor, which is always present in dry eye syndrome, and which underlies the “vicious circle” of development and progression of this disease, and also plays a major role in the development of complications in this condition. A pathogenetic approach to anti-inflammatory treatment for dry eye syndrome is the use of a certain group of drugs such as steroidal anti-inflammatory drugs and cyclosporine drops (Restasis), as well as tetracyclines. These drugs have a beneficial effect on the restoration of natural tear production by reducing the level of the inflammatory component in this syndrome. The choice of drug is always determined strictly individually, depending on the clinical picture and objective condition of the patient.
Stimulation therapy
Aimed at restoring and normalizing the functioning of the secretory glands responsible for the production of tear film components.
The use of correct dietary supplements has a stimulating effect on the production of tears of normal composition. Vitamins, minerals and omega-3s are valuable “ingredients” for eye health, necessary to maintain visual function and the proper functioning of all eye structures. In addition, omega-3 contains essential fatty acids - an essential component of the tear film, which prevents it from evaporating too quickly.
Another progressive aspect of stimulation therapy is the resumption of natural tear production by activating the natural tear-producing system using physiotherapeutic methods of therapeutic and stimulating effects. For this purpose, magnetic stimulation, laser stimulation, subconjunctival administration of drugs based on autologous blood plasma (PRP technology), exposure to polychrome light (visible radiation spectrum, a combination of intense pulsed light IPL and low-intensity phototherapy LLLT) are used. Such treatment is used both as an independent method and in combination with other methods of influence to restore the function of the meibomian glands, such as massage and eyelid hygiene.
Should be considered! The number and frequency of sessions of physiotherapeutic treatment and its combination with other types of therapy directly depends on the initial degree of dysfunction of the meibomian glands and, accordingly, the stage of dry eye syndrome, as well as on the dynamics of the manifestation of the effect of the therapy used.
Prices for treatment of dry eye syndrome
| Primary appointment (examination, consultation) with an ophthalmologist (examination for dry eye syndrome) | 8 790₽ |
| Service code | Service name | Number of services | Price |
| A02.26.004 | Visometry, 2 eyes Code: A02.26.004 | 1 | 350 ₽ |
| A02.26.013 | Determination of refraction using a set of trial lenses, 2 eyes Code: A02.26.013 | 1 | 550 ₽ |
| A02.26.015 | Ophthalmotonometry, 2 eyes Code: A02.26.015 | 1 | 400 ₽ |
| А03.26.001 | Biomicroscopy, 2 eyes Code: A03.26.001 | 1 | 990 ₽ |
| A03.26.003.001 | Examination of the periphery of the fundus using a lens, 2 eyes Code: A03.26.003.001 | 1 | 1 950 ₽ |
| А03.26.018 | Biomicroscopy of the fundus (central zone), 2 eyes Code: A03.26.018 | 1 | 900 ₽ |
| A12.26.016 | Autorefractometry with a narrow pupil, 2 eyes Code: A12.26.016 | 1 | 350 ₽ |
| B01.029.001.009 | Consultation with an ophthalmologist Code: B01.029.001.009 | 1 | 900 ₽ |
| A02.26.020 | Schirmer test Code: A02.26.020 | 1 | 600 ₽ |
| A03.26.021 | Determination of tear film breakup time Code: A03.26.021 | 1 | 200 ₽ |
| A02.26.017 | Determination of corneal surface defects (with fluorescein) Code: A02.26.017 | 1 | 400 ₽ |
| A03.26.005.001 | Biomicrography of the eye and adnexa (me-check), 2 eyes Code: A03.26.005.001 | 1 | 1 200 ₽ |
| SERVICE PACKAGE В01.029.001.010 | Promotion! Price for a package of services under the promotion ( Discount: 41% ): | 5 200₽ |
| Treatment and prevention of dry eye syndrome |
| Service code | Service name | Number of services | Price |
| A22.30.002.001 | Exposure to visible radiation M22 IPL, 2 eyes Code: A22.30.002.001 | 1 | 5 400 ₽ |
| A22.30.002.002 | Exposure to visible radiation EyeLight, 2 eyes Code: A22.30.002.002 | 1 | 5 400 ₽ |
| A22.30.002.003 | Exposure to visible radiation My Mask Red, 2 eyes Code: A22.30.002.003 | 1 | 5 500 ₽ |
| A22.30.002.004 | Exposure to visible radiation is complex (EyeLight, 1 eye + My Mask Red, 2 eyes) Code: A22.30.002.004 | 1 | 9 800 ₽ |
| A22.30.002.005 | Exposure to visible radiation is complex (EyeLight, 2 eyes + My Mask Red, 2 eyes) Code: A22.30.002.005 | 1 | 10 900 ₽ |
| A22.30.002.006 | Exposure to visible radiation (My Mask Yellow, 2 eyes) Code: A22.30.002.006 | 1 | 6 800 ₽ |
| A22.30.002.007 | Exposure to visible radiation is complex (EyeLight, 2 eyes + My Mask Yellow, 2 eyes) Code: A22.30.002.007 | 1 | 12 200 ₽ |