Redness, pain and itching in the corners of the eyes can indicate visual fatigue. But sometimes such symptoms are caused by inflammation of the lacrimal sac. Dacryocystitis develops due to complete or partial blockage of the lacrimal canal. Infections and injuries can provoke this phenomenon. Often the cause of this pathological condition is an abnormally narrow or tortuous tear duct. Inflammation of the lacrimal sac must be treated as quickly as possible, since the disease can quickly develop into a chronic form.
Causes
The main cause of the disease is an inflammatory process in the nasal cavity, paranasal sinuses, and bones surrounding the lacrimal sac. This leads to blockage and narrowing of the nasolacrimal canal and the retention of pathogenic microorganisms in it - most often streptococcal or staphylococcal flora. As a result, inflammation of the mucous membrane of the lacrimal sac develops.
Dacryocystitis is divided into simple, ecstatic, catarrhal and phlegmonous forms. The disease can also occur in the form of empyema of the lacrimal sac and stenosing dacryocystitis.
Chronic dacryocystitis mainly develops after an acute form.
In newborns, dacryocystitis occurs due to the persistence of the germinal film covering the lower segment of the nasolacrimal canal. By the time of birth, this film undergoes reverse development; with the first breath, it breaks. However, in some children (approximately 5-7% of newborns), the film retains its integrity. In newborns, dacryocystitis can occur in a simple, ectatic, catarrhal, purulent and phlegmonous form.
In some cases, the cause of inflammation of the lacrimal sac in newborns is congenital pathology of the lacrimal ducts or birth trauma.
Mechanism of occurrence
The lacrimal sac is located between the inner corner of the eye and the bridge of the nose. The back part is in the bone notch, and the front part is under the skin. The lacrimal sac is connected to the nose by the nasolacrimal duct; through this duct, tear fluid exits into the nasal cavity. When for some reason this channel becomes clogged, the drainage of fluid from the lacrimal sac is disrupted.
As a result of a blocked tear duct, fluid from the eyes cannot drain normally through the nose. Gradually, the inflammatory process begins and bacteria actively multiply.
Dacryocystitis is a fairly rare phenomenon in adults; it is more common in women.
Symptoms
Objectively, swelling is observed in the area of the lacrimal sac. When you press on it, mucous or purulent discharge is released from the lacrimal opening.
The rinsing solution does not pass into the nose. Long-standing dacryocystitis leads to overstretching of the lacrimal sac. The chronic form of the disease can be complicated by an acute inflammatory process in the form of phlegmon or abscess. Phlegmon is a diffuse purulent inflammation, an abscess is a purulent process limited by a capsule.
Acute dacryocystitis is accompanied by the formation of a painful infiltrate in the area of the lacrimal sac. The patient complains of severe lacrimation, redness, swelling and severe pain in the inner corner of the eye. Hyperemia and swelling of the lacrimal sac area are objectively determined.
Severe swelling leads to narrowing of the palpebral fissure. Pus from the lacrimal openings is released when pressure is applied to the area of the lacrimal sac at the onset of the disease. The tubular test initially shows a positive result, then the nasal and tubular tests become negative. CP is performed to determine the degree of patency of the lacrimal ducts.
Additionally, general symptoms are observed: fever, lethargy, weakness, apathy, headache. After a few days, an abscess may form.
Chronic dacryocystitis is accompanied by lacrimation, tearing along the edge of the lower eyelid and discharge of pus from the conjunctival zone. Upon examination, a bean-shaped soft-elastic protrusion is determined in the area of the lacrimal sac. Pressure on the area of the lacrimal sac leads to the release of purulent mucous discharge from the lacrimal opening. There is hyperemia of the conjunctiva of the eyelids. The tubular test gives a positive result; the nasal test gives a negative result. Rinse water does not pass into the nasal cavity.
Some patients develop hydrocele of the lacrimal sac. In this case, the lacrimal sac is overstretched so much that it is visible through the thinned skin.
In newborns, in the first days of life, mucopurulent discharge is observed from one or both eyes. When you press on the area of the lacrimal sac, mucus and pus are released from the lacrimal opening. The nasal test is negative, the tubular test is positive. Washing solutions do not pass into the nasal cavity. The disease can be complicated by the type of acute phlegmonous dacryocystitis.
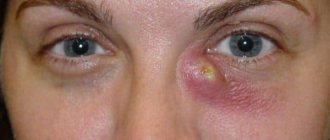
Photo
The photo shows variants of the course of dacryocystitis in adults and children.
Classification
Dacryocystitis can be congenital and acquired. Congenital inflammation of the lacrimal sac is divided into several forms, depending on the cause of the disease.
- Hypoplasia. In this case, the lacrimal glands are not fully formed.
- Aplasia. The lacrimal gland is completely absent.
- Hypertrophy is an enlarged lacrimal gland.
Inflammation can be unilateral or bilateral. In addition, acute and chronic forms of the disease are distinguished.
Diagnostics
Diagnosis includes an external examination of the eye, collection of anamnestic data and additional research methods. The examination plan includes:
- West test - a tampon is inserted into the nostril on the affected side, and a dye is installed into the eye. With normal patency, after a short period of time the tampon will acquire the color of the solution; if this does not happen after ten minutes, it means that the lacrimal canal is impassable.
- Probing - with the help of research, damage to the tear ducts can be detected.
- Bacterial culture of a smear from the nasolacrimal duct - analysis allows you to determine the infectious agent.
Treatment
Chronic dacryocystitis is treated surgically. Dacryocystorhinostomy is performed. In the acute form, anti-inflammatory therapy is indicated; after relief of signs of inflammation, surgery is performed. There are some differences between treatment tactics for adults and children.
In adults
Acute dacryocystitis is treated in a hospital setting. When a symptom of fluctuation appears (balloting or fluctuation of purulent contents), the abscess is drained, followed by washing the cavity with antiseptic solutions - 0.02% nitrofural solution. Before fluctuations appear, dry heat and ultra-high frequency therapy are used.
Antibacterial drugs are instilled into the conjunctival sac for 7-10 days - 5-6 times a day (0.3% solutions of ofloxacin, ciprofloxacin). Before going to bed, apply antibacterial eye ointment to the lower eyelid.
After opening the abscess, drainage is carried out with a 10% sodium chloride solution. For 3-7 days, the wound is washed with antiseptic solutions. As the area is cleaned over 5-7 days, the area is lubricated with agents that accelerate regenerative processes (10% methyluracil ointment or levomekol) - up to 3-4 times a day.
As part of systemic therapy, broad-spectrum antibacterial agents are used for 7-10 days: cephalosporins, semi-synthetic penicillins. In case of severe intoxication, detoxification therapy is prescribed. Non-steroidal anti-inflammatory drugs are also used intramuscularly. At the same time, magnetic therapy is carried out.
After the manifestations of the acute form subside, patients complain for a long time of lacrimation. Timely surgery allows you to restore lacrimal outflow.
Chronic dacryocystitis requires radical treatment. Dacryocystorhinostomy is performed - the formation of a direct anastomosis between the nasal cavity and the lacrimal sac. After surgery, antibacterial and non-steroidal anti-inflammatory drugs are prescribed intramuscularly, intravenously and locally.
In children
In case of inflammation of the lacrimal sac in newborns, a descending massage and lavage of the lacrimal ducts are performed. If these measures do not produce a positive effect, probe the nasolacrimal canal.
Dacryocystitis of newborns is treated as follows:
- jerky massage of the lacrimal sac area from top to bottom - up to 3-4 times a day for 10-15 days;
- a combination of massage with instillation of antiseptic solutions into the conjunctival cavity for one to two weeks - 0.02% furatsilin solution;
- if there is no effect from massage and rinsing, they resort to probing using a Bowman probe.
We recommend reading: Probing the lacrimal duct in children
Lacrimal sac
- Topography of the lacrimal sac
- Histology
- Blood supply and innervation
Topography of the lacrimal sac 1 - lacrimal sac, 2 - internal ligament of the eyelids, 3 - Horner's lacrimal muscle, 4 - tarso-orbital fascia, 5 - thickening of Tenon's bursa, 6 - conjunctiva of the eyeball, 7 - lacrimal caruncle, 8 - Tenon's bursa, 9 - retinaculum laterale.
The lacrimal sac is a cylindrical cavity closed at the top, 10-12 mm long and 3-4 mm in diameter; it is the upper part of the nasolacrimal duct. Its walls consist of mucous membrane and submucosal tissue, on top of which there is also a thin lacrimal fascia. The lacrimal sac is located at the inner corner of the orbit in the fossa of the lacrimal sac. The lower end of the lacrimal sac is somewhat narrowed and passes into the nasolacrimal duct without sharp boundaries.
Topography of the lacrimal sac
In a horizontal section of the skull at the level of the lacrimal sac, it can be seen that the lacrimal sac is located in a triangular space, having bone on the inside (the lacrimal fossa), in front - the internal ligament of the eyelids and the orbicularis muscle attached to it, and on the back - the tarso-orbital fascia.
Thus, the anterior wall of the fascial sheath of the lacrimal sac is formed by a deep layer of fascia of the circular muscle of the eyelids (fascia profunda m. orbicularis), the inner wall is the periosteum lining the lacrimal fossa, and finally, the posterior wall is the tarso-orbital fascia. It can also be mentioned that between the lacrimal sac and the tarso-orbital fascia there is another layer of muscle fibers associated with the orbicularis muscle of the eyelids and attached to the bone immediately behind the posterior lacrimal crest.
Therefore, when surgically approaching the lacrimal sac, when extirpating it, the surgeon’s knife must sequentially cut: the skin, the superficial layer of the fascia of the orbicularis muscle along with the internal ligament and fibers of the muscle, and finally, the deep layer of fascia covering the muscle behind and at the same time forming the anterior wall of the fascial sheath of the lacrimal sac. When this deep layer of fascia is cut, free access to the lacrimal sac lies in its fascial bed.
Histology
The mucous membrane of the sac and canal is lined with columnar epithelium, which has goblet cells that produce mucus. The submucosal layer is rich in adenoid tissue. The outer layers consist of dense fibrous tissue containing elastic fibers. The lower parts of the anterior wall of the lacrimal sac are poor in elastic tissue, and therefore, in this place, during dacryocystitis, stretching and protrusion of the sac wall occurs. This is where the incision is made for phlegmonous dacryocystitis.
Blood supply and innervation
The blood supply to the lacrimal sac is carried out by branches of the ophthalmic artery.
Accordingly, the area of the lacrimal sac under the skin passes a small angular artery (a. aogularis) and a much larger angular vein (v. angularis); This circumstance must be taken into account by the surgeon when performing operations on the lacrimal sac.
Sensitive innervation of the lacrimal part of the lacrimal system is carried out in such a way that the apex of the lacrimal sac receives sensory fibers from the subtrochlear nerve (n. infratrochlearis, from n. nasociliaris n. ophthalmici, i.e., from the first branch of the trigeminal nerve), and the lower half of the lacrimal sac and the upper part of the nasolacrimal canal - from the suborbital nerve (n. infraorbitalis, from n. maxillaris, i.e., the second branch of the trigeminal nerve.