Causes of dacryoadenitis
The disease develops as a result of penetration of pathogenic microflora into the lacrimal sac. Acute dacryoadenitis often develops as a complication of mumps (mumps), which occurs with damage to the submandibular and parotid salivary glands, gonorrhea, tonsillitis, rheumatism, scarlet fever, pneumonia, typhoid fever and influenza.
The chronic form of the disease is often observed against the background of certain diseases of the hematopoietic system. Cases of dacryoadenitis of syphilitic or tuberculous nature are much less common.
Diagnostics
Diagnostic measures for dacryoadenitis are performed by an ophthalmologist. The examination at the reception begins with the collection of complaints and an external examination.
The position of the eyelids, eyeballs, and their mobility are assessed. The fundus is examined, the lacrimal gland is palpated, and the lacrimal duct is washed. In the presence of purulent discharge, microflora culture is recommended.
Additional studies may require consultation with related specialists for a systemic disease (infectious disease specialist, hematologist, dermatologist, otolaryngologist), blood test for immunoglobulins, c-reactive protein, ultrasound of the eye, CT/MRI of the orbit.
Symptoms of dacryoadenitis
In its course, dacryoadenitis can be acute or chronic. The acute form of the disease is quite rare and is most often observed in children. At the same time, acute dacryoadenitis never occurs as an independent disease, but manifests itself as one of the possible complications of tonsillitis, flu, intestinal and other infections. Often, acute inflammation of the lacrimal gland is observed against the background of mumps. Moreover, in children vaccinated against mumps, dacryoadenitis may be the only symptom of this infectious disease.
The first sign of incipient inflammation of the lacrimal gland is the appearance of a slight swelling of the upper eyelid, which then gradually or quite quickly increases in size. The eyelid becomes painful, swollen, and red. Then the body temperature rises, headache, fatigue, and weakness appear. Due to the increase in edema, the edge of the eyelid begins to take on an S-shape.
The process is progressing quite quickly. The pain intensifies, and the swelling of the upper eyelid becomes so pronounced that the patient cannot open his eyes. The pain can be so intense that the patient does not allow the doctor to even touch the affected lacrimal gland. Subsequently, the swelling begins to spread to the temporal region, and the lymph nodes in the postauricular region enlarge.
The course of acute dacryoadenitis is usually favorable. Full recovery occurs within two weeks. But in patients with reduced immunity, the disease may be complicated by the development of an abscess of the upper eyelid or phlegmon spreading to the fatty tissue of the orbital region. This is a very dangerous complication, since a widespread purulent process can cause meningitis or cavernous sinus thrombosis - diseases that can be fatal.
Chronic dacryoadenitis is usually observed against the background of certain diseases of the hematopoietic system (alukemic lymphadenosis, chronic lymphocytic leukemia). Also, the disease can have a tuberculous and, much less frequently, syphilitic etiology. In very rare cases, acute inflammation of the lacrimal gland becomes chronic.
Chronic dacryoadenitis is manifested by the formation in the area of the lacrimal gland of a swelling that is quite dense to the touch, which extends deep into the orbit. The skin over it remains unchanged. If you turn out the upper eyelid, then in its upper outer corner you can see a small protrusion formed by the enlarged palpebral part of the gland.
Chronic dacryoadenitis can be either unilateral or bilateral. The disease usually occurs without pronounced signs of inflammation.
Diagnosis of syphilitic dacryoadenitis is carried out on the basis of the characteristic symptoms of a chronic inflammatory process in the lacrimal gland, positive serological reactions and anamnesis.
With tuberculous dacryoadenitis, small areas of calcification form in the lacrimal gland, which are clearly visible on radiographs. In addition, many patients experience other symptoms of tuberculosis (positive Mantoux and Pirquet tests, enlarged cervical lymph nodes, etc.).
Clinical picture
- Severe pain in the outer part of the upper eyelid.
- Swelling of the eyelid.
- Restricted mobility of the eyeball outward and upward.
- The upper eyelid takes the shape of the English letter S in a horizontal position.
- Sharp pain when palpating the eye area.
- Retracting the upper eyelid allows you to see the enlarged lacrimal gland.
- Swelling of the conjunctiva of the eyeball.
- Diplopia.
- Headache.
- Fever, chills.
- Lymphadenopathy.
Dacryocystitis and its prevalence
Pathology is detected in approximately 5-7% of cases of all diseases affecting the lacrimal organs, while in women dacryocystitis is detected 8 times more often than in men. This is due to the presence of a narrower nasolacrimal duct in females. Among age groups, most cases of dacryocystitis are diagnosed in people of mature age (30-60 years). Dacryocystitis of newborns is a very common phenomenon, which is classified as a special form of the disease.
If dacryocystitis is not treated, purulent lesions of the eye tissue often develop, which poses a risk of septic complications due to the proximity of the brain. The most severe consequences of dacryocystitis are meningitis, encephalitis, and brain abscess.
In a healthy person, the tear fluid, which is produced by the lacrimal glands, flows around the eye, after which it is directed to its inner corner to the lacrimal openings, and from them into the lacrimal canals. Then the tear fluid passes into the lacrimal sac, and then through the nasolacrimal duct it enters the nasal cavity. If a person develops dacryocystitis, then a complete or partial blockage of the canal occurs. Lacrimal drainage changes pathologically, so tear fluid accumulates in the lacrimal sac. This sac is a cylindrical cavity located at the top of the nasolacrimal duct. Gradually, stagnant fluid causes tissue inflammation - dacryocystitis.
Forecast
The disease usually lasts from 1 to 3 weeks. The duration of treatment ranges from 14 to 21 days, depending on the form and severity of the disease. The entire examination takes place in special institutions, where all the necessary tests are taken, the causes are identified and treatment is prescribed.
With timely treatment, improvements can be seen within a week. As for the acute form, in the absence of the need for surgical intervention, everything depends on the severity of the underlying disease.
Comparing acute and chronic diseases, the second will be quite easier, both in terms of timing and recovery. But in this case, you must go to the hospital, otherwise dacryoadenitis will not only develop into an acute form, but will require additional examination and surgical intervention.
Dacryoadenitis (inflammation of the lacrimal glands)
Dacryoadenitis is an ophthalmological disease characterized by inflammation of the lacrimal gland. As a rule, the disease rarely occurs independently; usually inflammation of the lacrimal gland is a complication of another disease. In ophthalmology, acute and chronic dacryoadenitis is distinguished.
The acute form is more common in children, the chronic form is observed in people of mature age. Treatment of dacryoadenitis is usually conservative, using anti-inflammatory drugs and physiotherapy. In severe cases, surgical intervention is required when an abscess forms.
Description and features
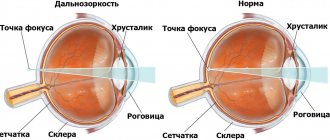
The lacrimal glands are one of the main elements of the accessory elements of the human visual apparatus. They belong to the tubular glands and visually resemble a horseshoe of two segments.
It is thanks to the lacrimal gland that the normal functioning of the eyeball is ensured.
They produce tear fluid, which cleans the surface of the cornea, lubricates it, moisturizes it, ensures clear images and protects it from minor damage.
Inflammation of the lacrimal glands usually occurs against the background of infectious processes of the visual apparatus. Dacryoadenitis is diagnosed in people of any age and gender.
Acute dacryoadenitis usually occurs in young children with weakened immune systems. The provoking factors in this case are:
- sore throat, scarlet fever;
- parotitis;
- flu;
- intestinal infections.
Acute dacryoadenitis, as a rule, develops against the background of other infectious diseases
Several other reasons for the development of chronic dacryoadenitis. A sluggish inflammatory process of the lacrimal gland can develop in the following cases:
- active tuberculosis;
- syphilitic lesions, gonorrhea;
- chronic lymphocytic leukemia;
- sarcoidosis;
- reactive arthritis;
- Wegener's granulomatosis.
In recent years, thanks to numerous studies, a connection has been established between dacryoadenitis and lymphomatous hyperplasia, which also affects the salivary, parotid and submandibular glands.
Symptoms and development
Symptoms of inflammation of the lacrimal glands in the acute stage appear clearly, it is impossible not to notice them. Typical complaints of patients with dacryoadenitis:
- redness and swelling of the eyelid;
- pain on palpation in the area of the lacrimal gland;
- as inflammation progresses, pronounced ptosis of the upper eyelid appears in the shape of the letter “S”;
- limited movement of the eyeball in all directions;
- “dry eye” syndrome due to decreased production of tear fluid by the inflamed gland.
It is almost impossible to miss the symptoms of acute inflammation of the lacrimal gland in a child.
In the photo you can see exactly what an eye affected by acute dacryoadenitis looks like. In most cases, only one gland becomes inflamed; in the acute phase, general symptoms of intoxication are also noted:
- Increase in body temperature, sometimes very significant.
- Headache.
- Severe enlargement and pain of the lymph nodes.
Upper eyelid abscess
In the chronic form of the disease, the symptoms are the same, but they are less pronounced.
The eyelid over the affected lacrimal gland is moderately hyperemic, dense and hot to the touch, but the patient does not feel painful sensations on palpation.
Ptosis can be very mild; in some cases, there is a slight narrowing of the palpebral fissure. The movements of the eyeball are not impaired, tear fluid is produced in sufficient quantities.
It is noteworthy that in the chronic form of the disease, two eyes are most often affected.
Symptoms can be very mild for a long time, sometimes months and even years pass before the patient consults an ophthalmologist and begins treatment.
The most dangerous complication is the development of an abscess or phlegmon. In this case, the infection can spread to the brain tissue and cause meningitis.
Diagnostic and treatment methods
Inflammation of the lacrimal gland is easy to pre-diagnose through visual examination and questioning of the patient. Modern laboratory and instrumental methods are also used to collect a complete history:
- viziometry;
- tonometry;
- biomicroscopy of the eye.
For successful treatment of the inflammatory process, local and systemic drugs, as well as physiotherapy, should be used in combination
All these manipulations are needed more to identify the cause of dacryoadenitis and determine optimal treatment methods. Usually external symptoms are enough to diagnose an acute form of the disease. The diagnosis of chronic inflammation of the lacrimal gland is somewhat complicated. In this case, the following procedures may additionally be carried out:
- Ultrasound of the eyeball.
- MRI or CT, if differential diagnosis is required for suspected neoplasms in the structures of the eyeball.
- Fluorography or chest x-ray if tuberculosis is suspected to be the cause of dacryoadenitis.
- Mantoux test or Diaskintest for the same reason.
- Biopsy of lung tissue for suspected sarcoidosis.
- Serological tests.
- Biochemical study of saliva in cases of suspected Mikulicz disease.
Treatment is prescribed depending on the form of the disease and its etiology. Acute forms of dacryoadenitis are usually treated with conservative methods. What can an ophthalmologist prescribe in such cases:
- a course of antibiotic therapy, using products for external use (ointments, rinsing solutions), tablets for oral administration, intramuscular injections;
- physiotherapy – warming with dry heat, UHF;
- anti-inflammatory drugs in various forms;
- analgesics for severe pain.
Treatment of dacryoadenitis alone does not make sense if the underlying disease that provoked it is not treated. A comprehensive scheme is selected by an ophthalmologist together with a specialist - pediatrician, immunologist, phthisiatrician, venereologist, etc. As a rule, doctors recommend going to a hospital during treatment.
Surgery is required if inflammation has led to the formation of an abscess. In this case, under local anesthesia, the abscess is opened, the wound is cleaned, washed with an antiseptic, after which drainage is installed to ensure the outflow of residual pus and prevent re-suppuration. Next, treatment is carried out according to the standard regimen, always using antibiotics.
Important: if the chronic form of dacryoadenitis is difficult to treat, X-rays are used to irradiate the affected eyeball. This method is considered outdated, as it has a number of contraindications and side effects; it is not suitable for treating young children. But if there is no choice, then irradiation is carried out, strictly controlling the irradiation dosage.
Prevention of inflammation
It is no secret that pathology is much easier to prevent than to cure. To prevent the development of the inflammatory process in the lacrimal duct, you should adhere to the following recommendations:
Careful hygiene of the eyes and the entire face as a whole
It is important to avoid touching your eyes with your hands, especially if they are not washed. If there are certain congenital abnormalities in the general physiological structure of the lacrimal system, it is important to carry out a special correction, and to do this before the inflammatory process occurs. Mechanical and physiological damage to the visual organs must be avoided. It is required to treat diseases of the paranasal sinuses and other eye pathologies that have an inflammatory form as promptly as possible. It is advisable to undergo preventive examinations by a professional ophthalmologist. This must be done at least once a year.
Due to the fact that dacryocystitis is usually accompanied by pronounced symptoms, there are no special problems with its diagnosis. The only problem in this case is ignoring the pronounced signs of inflammation.
You shouldn’t do this, you shouldn’t hope that the problem will go away on its own, and especially you shouldn’t self-medicate.
Therapeutic measures
Dacryoadenitis requires urgent treatment, especially its acute form. The main goal of therapy is to eliminate inflammation. Any therapy must be agreed with a specialist. When using insufficient dosage and duration of therapy, dacryoadenitis acquires its chronic form.
Antibiotics are used as drugs for local and internal use. Drops are used locally (lasting up to 7–10 days):
- levofloxacin, 1 drop 3 times a day;
- "Tobramycin", 1 drop 4 times a day;
- chloramphenicol 0.25%, 2 drops 4 times a day.
Among the ointments used:
- tetracycline 1%;
- gentamicin 0.1%;
- antiviral acyclovir 3%.
Ointments are placed behind the lower eyelid up to three times a day. In addition to antibacterial agents, anti-inflammatory (diclofenac sodium drops 0.1%) and hormonal (Prednisolone, Dexamethasone in the form of ointment or drops) drugs, tear substitutes (artificial tears) are used.
Dacryocystitis.
Dacryocystitis occurs in the form of acute or chronic inflammation of the lacrimal sac. Patients complain of lacrimation and purulent discharge from the conjunctival cavity. Swelling in the area of the lacrimal sac is often visible. When pressing on this area, mucous or mucopurulent contents flow out abundantly from the lacrimal openings. The tubular test is most often positive, and the nasal test is negative. When rinsing, the liquid does not pass into the nose and flows out in a stream along with the contents of the lacrimal sac through the upper lacrimal punctum.
Chronic dacryocystitis is a serious danger to the eye, as it is often the cause of a purulent ulcer of the cornea, which develops with minor damage to the epithelium, for example, when a speck accidentally enters the eye.
Treatment of chronic dacryocystitis is only surgical. Dacryocystorhinostomy is performed - the creation of a direct anastomosis between the lacrimal sac and the nasal cavity to restore the outflow of tears into the nasal cavity.
Dacryocystitis of newborns is a borderline condition between a developmental anomaly and an acquired pathology. The outcome of the disease depends on timely diagnosis and treatment. Dacryocystitis of newborns occurs due to obstruction of the nasolacrimal duct, in which in approximately 2-3% of newborns there is a membrane that closes the exit from the nasolacrimal duct into the nasal cavity.
The first sign of the disease is mucous or mucopurulent discharge from the conjunctival sac. This is often regarded as conjunctivitis and appropriate treatment is prescribed. The cardinal sign of dacryocystitis helps to distinguish dacryocystitis from conjunctivitis - the presence of mucopurulent discharge from the lacrimal openings when pressing on the areas of the lacrimal sacs. The West test confirms this diagnosis.
Unrecognized dacryocystitis leads to a serious complication - phlegmon of the lacrimal sac.
Treatment.
- Treatment of dacryocystitis in newborns should begin with a massage of the lacrimal sac, carried out by gentle pressure with a finger at the inner corner of the palpebral fissure from top to bottom. In this case, the membrane covering the nasolacrimal duct, under the violent pressure exerted by the contents of the sac, can break through and the patency of the lacrimal ducts is restored.
- Mandatory instillation of antiseptic drops (30% sodium sulfacyl solution, antibiotic solutions) is recommended.
- If recovery does not occur within weeks with this treatment, it is necessary to try to break through the membrane by washing the lacrimal ducts with antiseptic solutions under pressure. The procedure is performed by a doctor.
- If this procedure is unsuccessful, they resort to probing, which is repeated if necessary.
Treatment
In the acute phase, treatment is usually aimed at combating inflammation (since the eyelid can swell to such a size that it completely closes the eye and increases pain). Observation of the acute form is carried out under the supervision of specialists in a hospital. Inpatient treatment of dacryoadenitis also includes the following measures:
- Physiotherapy. They include UHF therapy, dry heat.
- Prescription of medications: antibacterial drugs administered orally or intramuscularly, anti-inflammatory drugs, analgesics.
- Surgical intervention.
In addition to antibiotics, folk remedies are also used:
- massage of lacrimal points;
- washing with a mixture of various infusions;
- tea and bread compresses.
Treatment of the general disease is carried out together with the main treatment, and includes anti-inflammatory drugs.
Tavegil and analgesics are most often prescribed. The first is for severe swelling, the second is for unbearable pain and bifurcation.
Magnetic therapy is used along with the main treatment. After reducing the aggravating phase of inflammation, physiotherapeutic treatment is prescribed.
Boy with dacryoadenitis
In some cases, the lacrimal gland has to be opened with an incision through the conjunctiva to improve outflow.