When a tear duct is blocked, the eye's drainage system is either partially or completely blocked, preventing tears from draining naturally. This leads to watery eyes, irritation or chronic eye infection.
Most tears come from the lacrimal glands located above the eyes. Tears run down the surface of the eye, lubricating and protecting it, and then fall into tiny holes (points) in the corners of the upper and lower eyelids. They then pass through small channels in the eyelids to the lacrimal sac, the junction of the eyelids and the side of the nose, then down the nasopharyngeal duct and are either evaporated or reabsorbed before entering the nose.
Infants may have a congenital tear duct obstruction : almost one in five babies are born with a blocked tear duct, but this anomaly usually resolves after 4-6 months.
In adults, a blocked tear duct can be caused by an eye infection, swelling, injury, or tumor.
Causes of tear duct obstruction
A blockage can occur at any point in the tear drainage system. When this happens, tears do not drain properly, leading to watery eyes and increasing the risk of developing eye infections and inflammation.
Babies in the womb have a thin membrane that seals the nasopharyngeal duct. Congenital tear duct obstruction may result from the membrane not opening properly when the baby is born.
Another cause of blocked tear ducts can be chronic nasal infections, such as sinusitis, which irritate the tissue and form scars that block the tear duct system.
Other causes of blocked tear duct:
- Abnormal development of the skull and face, as in Down syndrome or other disorders, increases the likelihood of tear duct obstruction in children.
- Trauma to the nose, such as a broken nose; Scar tissue may block the tear duct.
- Nasal polyps that grow from the lining of the nose (affecting some people with allergic rhinitis) can block the tear duct system
- Conjunctivitis, an infection and inflammation of the conjunctiva, the thin membrane that covers the eye.
- In rare cases, the tear duct system can become infected and blocked, especially after certain viral infections.
- A tumor that can put pressure on the tear duct system and prevent drainage.
Symptoms of tear duct obstruction in children
One obvious manifestation is excessive tears, which may begin to flow with a vengeance after a cold or sinus infection. Additionally, symptoms may be more noticeable after exposure to cold, wind, or sunlight.
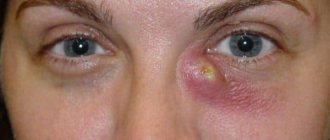
When the tear ducts are blocked, bacteria growing in the nasopharyngeal sac can lead to an infection called dacryocystitis .
Symptoms of dacryocystitis include:
- inflammation (swelling), tenderness, and redness of the inner corner of the eye or around the eye and nose;
- recurrent eye infections;
- secretion of eye mucus;
- brittle eyelashes;
- blurred vision;
- bloody tears.
Obstruction of the nasolacrimal duct in children
What is congenital dacryocystitis, what symptoms accompany the disease, and how is treatment done, says ophthalmologist Alexander Evgenievich Gorkin.
Gorkin Alexander Evgenievich Ophthalmologist
Good afternoon. My name is Gorkin Alexander Evgenievich, I am an ophthalmologist, ophthalmic surgeon at the Scandinavia clinic. Today I would like to talk to you about a disease such as congenital dacryocystitis. Tears are constantly produced in the mucous membrane of the eye. Its excess should normally flow through the lacrimal system, which consists of the upper and lower lacrimal canaliculi, located in the upper and lower eyelids. Next, the tear enters the lacrimal sac, from which it should flow down the nasolacrimal duct into the nose.
The tear drainage system has a series of valves that ensure the outflow of tears in a certain direction, from the eye towards the nose. It is the congenital underdevelopment of the valve at the mouth of the lacrimal sac at the transition to the lacrimal canal that is, as a rule, the cause of the development of dacryocystitis in newborns or obstruction of the lacrimal canal. What clinical picture is typical for this disease? The disease usually appears in the first month of life and is characterized by constant or periodic lacrimation. A tear can stand in the eye and flow onto the skin in the outer or inner corner. In this case, the skin, as a rule, becomes irritated and macerated. When a secondary infection occurs, purulent discharge may appear, but this is not a mandatory sign of this disease. The eye itself, as a rule, does not become red or irritated with this disease, which makes it possible to distinguish it from ordinary conjunctivitis.
What are the treatment tactics? First of all, for this disease, the doctor will prescribe a massage. Massage of the lacrimal sac is carried out at home by parents themselves. Pressure on the lacrimal sac must be carried out in the direction from top to bottom, since in this case it is possible, as a result of pressure in the lacrimal sac, to break through this barrier at the exit into the nasolacrimal canal. If pressure is applied in a circular or jerky manner, the contents of the sac will simply be squeezed into the lumen of the palpebral fissure through the lacrimal canaliculus and there will be no effect from the massage. The principle here is similar to a balloon: in order to burst, it must be filled. There is no point in squeezing an empty bag.
In most cases, dacteocystitis resolves with massage. If a child has purulent discharge, the doctor will additionally prescribe anti-inflammatory and antibacterial drops. If dacteocystitis does not go away due to massage, it is necessary to probe the nasolacrimal canal. This operation is performed on an outpatient basis under local anesthesia. The optimal time for performing this operation is the age of 3-4 months, since a child at this age tolerates this procedure as easily as possible. The operation is carried out, as I already said, under local anesthesia. No incisions are made during this operation. The surgeon, using a special thin probe, passes through the natural lacrimal ducts and pierces the obstruction at the exit from the lacrimal sac. As a rule, after this, symptoms completely disappear within 2-3 days. In some cases, extremely rarely, repeated probing is required. But, again, this happens quite rarely.
Is probing always necessary? No not always. Because in some children, lacrimation occurs only occasionally, for example, when going outside into the cold air. In this case, as a rule, the disease is not associated with any mechanical obstruction, but is associated exclusively with the physiological narrowness of the lacrimal ducts. Typically, this condition resolves on its own by about 1 year of age as the child grows.
I would like to draw attention to such a serious complication of dacryocystitis in newborns as phlegmon of the lacrimal sac. This condition causes swelling, redness and swelling in the inner corner of the eye. It is connected with the fact that the lacrimal sac is blocked not only at the exit into the nasolacrimal canal, but it is also blocked in the lacrimal canaliculus, and the sac becomes completely clogged and swells with purulent contents. This disease requires emergency hospitalization and treatment in an ophthalmological hospital. After the probing procedure, the doctor will prescribe anti-inflammatory antibacterial drops, which will allow postoperative swelling to go away as quickly as possible and restore the patency of the lacrimal ducts.
Publication date: 10/26/16
Treatment of tear duct obstruction
Sometimes several procedures are required to completely open a blocked tear duct. If an infection is suspected, the doctor will most likely prescribe antibiotics .
For many children with congenital tear duct obstruction, the condition resolves in the first few months of life as the drainage system matures or the additional membrane that includes the nasolacrimal duct opens. To stimulate these actions, the ophthalmologist may recommend a special massage .
The purpose of the massage is to apply pressure to the lacrimal sac in order to open the membrane at the bottom of the tear duct. To do this, the adult places his hands on either side of the child's face and, with his index fingers placed between the inner corner of the eye and the side of the nose, presses and lowers the tear sacs for a few seconds. One session includes 10 such movements.
Massage should be done in the morning and evening. The best time for this procedure is during a diaper change.
If the obstruction of the tear duct is caused by injury, then, as a rule, within a few months after the injury, the drainage system recovers on its own. If this does not happen, the patient is scheduled for surgery.
For infants whose blocked tear ducts do not open on their own, dilatation, probing, and irrigation . During this procedure, a narrow probe is passed through the puncture and nasal opening, and the tear drainage system is flushed with saline solution. This helps clear any residual clogs.
Balloon dacryoplasty involves opening narrowed or scar-blocked drainage channels under general anesthesia. For this, a narrow catheter and a balloon are used.
Through a procedure called stenting or intubation , which is performed under general anesthesia, microscopic tubes are used to open blockages. The doctor places a tube through one or both of the corners of the eye, drainage system and nose and leaves it there for 3-4 months, after which it is removed.
There is also an option with surgery. It is suitable for babies with a congenital anomaly when all other methods have been tried.
Dacryocystorhinostomy is the name of a surgical procedure that is usually performed to treat most cases of blocked tear ducts in adults and rarely in children. This operation creates a new route for tears that runs between the lacrimal sac and the nose. It passes by the nasolacrimal duct, which is usually the site of the blockage. Stents are placed there for 3-4 months for healing, which are then removed.
Depending on the type of blockage, the surgeon may recommend creating an entirely new route from the points to the nose, bypassing the tear drainage system. In essence, this is the restoration of the entire drainage system, which is called conjunctivodacryocystorhinostomy . After about 3-6 months, the ophthalmologist will remove any stents that were placed to keep the new canal open while it heals.
If the obstruction of the tear duct is caused by a tumor, then surgery is usually performed to remove it or other methods are used to reduce the tumor.
On the Vikids platform you can:
Dacryoadenitis - symptoms and treatment
Acute dacryoadenitis. The acute form is characterized by a sharp onset - the patient complains of pain on palpation, redness and swelling of the outer part of the upper eyelid. Due to edema, the outer edge of the upper eyelid is drooped, the palpebral fissure becomes S-shaped or completely closed. Swelling can spread to the temporal region and the entire half of the face, leading to complete closure of the palpebral fissure.
In acute dacryoadenitis, the pre-auricular lymph nodes enlarge and become painful. The eyeball deviates inward and downward, a slight protrusion of the eyeball from the orbit and double vision appear. The upward and outward movement of the eye is impaired. When the upper eyelid is retracted, redness and swelling of the conjunctiva are visible [6].
In children with weakened immune systems, severe cases may develop an abscess or phlegmon of the gland, which can spread to the space behind the eye.
There is also a deterioration in the general condition: body temperature rises, headache and weakness appear, sleep and appetite are disturbed [2]. Acute dacryoadenitis usually lasts 1-3 weeks.
Chronic dacryoadenitis. There are no signs of acute inflammation. The lacrimal gland is dense, enlarged and in rare cases painful on palpation. The skin color of the upper eyelid does not change. Due to the enlargement of the lacrimal gland, the palpebral fissure can be narrowed from the outside. Eye movements are not impaired. Symptoms develop gradually, so it may take several months before you see a doctor. When determining the function of the lacrimal gland, a decrease in tear production is detected, and histological examination reveals the presence of chronic inflammation around the ducts [5].
With tuberculous chronic dacryoadenitis, swelling in the area of the lacrimal gland gradually increases, and pain appears on palpation. Other signs of tuberculosis are also present: enlarged cervical lymph nodes and fluoroscopic changes in the lungs [12].
Dacryoadenitis with syphilis. Dacryoadenitis can occur both with primary syphilis and manifest itself as a painless enlargement and thickening of the gland, enlarged lymph nodes, and with tertiary syphilis - in this case, a soft tumor appears in the area of the lacrimal gland. The diagnosis is based on a thorough history taking and identifying symptoms of syphilis in other organs [12]. Syphilis leads to chronic inflammation of the lacrimal gland in very rare cases.
With Mikulicz's disease. Mikulicz disease is a chronic lymphomatosis of the lacrimal and salivary glands caused by systemic diseases of the lymphatic system, such as leukemia and pseudoleukemia [2]. With the disease, there is a bilateral enlargement of the lacrimal and salivary glands (usually the submandibular glands, less often the parotid and sublingual glands). The lacrimal glands enlarge to such an extent that the eye moves downward and inward. Possible protrusion of the eye forward. The palpebral fissures are narrowed by overhanging eyelids, the lymph nodes are enlarged. Patients complain of dry mouth and eyes - this is due to decreased gland function.
For sarcoidosis. Sarcoidosis is a systemic disease from the group of granulomatosis, the cause of which is not fully understood. With sarcoidosis, many nodules form in the skin, lymphatic system and internal organs. Granulomas are of the same type and clearly demarcated from the surrounding tissue. Damage to the lacrimal gland usually occurs against the background of general manifestations of the disease, but can also occur without the involvement of other organs and systems. The disease begins unnoticed and lasts a long time. It is characterized by enlargement of the lacrimal gland, often uniform, without clear identification of the sarcoid node. The lacrimal gland is painless on palpation, its function is reduced. Making a diagnosis is always difficult.
Pseudotumorous dacryoadenitis. It is a type of orbital pseudotumor - a group of diseases the development of which is caused by inflammation; the name “pseudotumor” (tumor - tumor) reflects their ability to masquerade as an oncological process. Recently, pseudotumors have been classified as autoimmune diseases, although the cause of their occurrence is unknown.
Clinically, pseudotumor of the lacrimal gland occurs subacutely and is characterized by a pronounced enlargement of the lacrimal gland. Upon palpation, a dense, non-displaceable, painless formation with a smooth surface is determined. Patients complain of swelling of the upper eyelid and its slight drooping. However, the skin at the site of swelling is usually not inflamed. With prolonged progression, inflammation spreads to surrounding tissues. The pseudotumor ends with the stage of dense fibrosis—the proliferation of connective tissue with the appearance of scars[12].