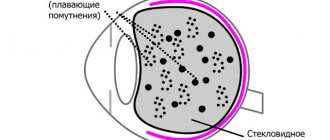
One of the reasons for decreased visual acuity is clouding of the internal refractive media.
If this occurs in the vitreous, vision may be reduced or remain normal.
This depends on the degree of spread of the pathological process and areas of accumulation of various fractions of substances. This condition should not be tolerated; it develops over time. The sooner therapy begins, the greater the patient’s chances of fully maintaining vision function.
Why does cloudiness occur?
There are many different reasons why vitreous opacities can develop:
- age over 50 years, at which physiological processes associated with the accumulation of various substances occur;
- severe myopia, in which the patient develops vision from -6 diopters;
- inflammatory conditions of the eyeball that develop periodically, becoming chronic;
- diseases spreading to the endocrine glands (hyperthyroidism, diabetes mellitus, pancreatitis);
- temporary disruption of the endocrine background, which occurs during pregnancy, adolescence, menopause, andropause;
- pathological conditions of the microcirculation vessels of the eye, which develop due to systemic diseases (hypertension, atherosclerosis, coronary disease, vascular fragility);
- Excessive strain on the eyes, which occurs with frequent exposure to cramped spaces, prolonged use of a computer and other electronic devices;
- mechanical damage to any parts of the visual organs;
- lack of vitamins and other beneficial substances from food, which leads to hypovitaminosis or vitamin deficiency;
- stress, depression, neuroses, psychoses;
- the effect on the body of infections, viruses, fungi, toxins, especially if pathological processes occur in the organs of vision.
It is not enough for a doctor to simply clear the vitreous body of accumulated substances. He needs to identify the root cause to completely eliminate the risk of recurrence of the condition.
Therapy
If a pathology is detected in the structure of the vitreous body, there are no treatment methods as such. But what should we do? Only carrying out prevention. In case of severe pathological processes in the VT in the absence of effect from conservative treatment, today it is possible to perform a vitrectomy operation (fragmentation, aspiration and replacement of the vitreous body) provided that the IOP - intraocular pressure - is constant. But it is not widely used due to its high morbidity. It is also possible to perform YAG laser vitreolysis (cleavage of visible opacities with a laser).
Diagnostics
If the patient’s visual acuity has sharply decreased, or clouding occurs in only one or both organs of vision, it is recommended to consult an ophthalmologist. He will conduct several diagnostic tests to make a reliable diagnosis:
- Anamnesis collection. The doctor will ask the patient when vision loss began and whether there were such conditions in the past. The patient may complain of spots before the eyes, multiple opacities that progress over time.
- General inspection. If the pathological condition is at an early stage of development, no symptoms will be visually detected. In the presence of severe clouding of the vitreous body, the accumulated fractions of substances can transfer to the cornea, which causes white spots inside it.
- Visometry. This is a study using diagnostic tables. The more lines the patient sees in them, the better his visual acuity.
- Autorefractometry. This is a test that can be used to determine the refractive ability of the eyeball. The vitreous body refracts rays, transmitting them to the retina. If this structure is broken, the autorefractometer will show this data.
- Ultrasound examination of the eyes. Using the test, you can identify the shape of the eyeball and the condition of the intraocular elements.
- Optical coherence tomography. The patient sits in front of the tomograph and focuses his gaze on the mark. The device scans the organ of vision, producing layer-by-layer image results.
- Fundus examination. The patient is first instilled with Atropine or similar agents that dilate the pupil. The doctor determines the quality of the structural elements; vitreous opacities are always visible through examination.
Based on these data, it is possible not only to identify vitreous opacities, but also other pathological conditions of the eyeballs. Only after making a diagnosis can the doctor begin treatment.
Treatment
Initial and slowly progressing variants of DST, as a rule, do not require treatment - especially since effective drug regimens have not yet been found (in such cases, as a rule, ophthalmologists prescribe “vascular eye drops” - Emoxipin or Taufon, vitamins for vision, enzyme drugs in tablets - Wobenzym).
In the worst case, and under the condition of constant conscious (or unconscious, neurotic) fixation of attention on them, floating threads or spots can become a source of psychological discomfort, without objectively affecting either visual acuity or other characteristics of the visual system. However, in most cases, the natural development of the process (for example, a gradual increase in age-related changes) leads to the gravitational lowering of inhomogeneities under the main optical axis of the eye, i.e. “floaters” simply stop creating interference in the most active central field of view. At the same time, the visual centers of the cerebral cortex gradually adapt to the existence of persistent interference and begin to ignore them, filtering them out and excluding them from the final visual image.
If the destruction of the vitreous body is a consequence of a more general and serious pathology, for example, inflammation of the retina, diabetic retinopathy, etc., such trends certainly require diagnosis, constant monitoring and treatment (at least preventive or supportive) by an ophthalmologist . In the most advanced, rapidly progressing and threatening variants of the development of DST, vitrectomy is performed - an ophthalmic surgical operation to partially or completely remove the vitreous substance and replace it with a balanced biocompatible salt solution, the physical and optical parameters of which correspond to the natural characteristics of a healthy vitreous.
Not being absolutely safe in terms of risks and possible complications (however, like any other surgical intervention practiced today), vitrectomy is considered as an ultima ratio, i.e. as a “last argument”, a forced measure to preserve vision, and ends in therapeutic success in a very large percentage of cases - according to various estimates, from 80% to 90%.
Methods of therapy
The doctor selects the treatment method depending on the severity of the patient’s visual condition. There are several ways in which the eyeball can be treated conservatively. But the doctor can also choose surgical or laser therapy.
Treatment is not always carried out. Often the patient has a partial vitreous opacification that does not develop over time. But such patients need to periodically visit an ophthalmologist to determine the condition of the eyeballs. If the clouding develops and fills all structures, conservative and surgical therapy is necessary.
Conservative therapy includes the following types of drugs:
- medications that normalize the state of microcirculation of the blood vessels of the eyes (Emoxibel, Emoxipin), they are used in small courses to periodically stimulate the blood flow of the eyeball;
- medications that normalize blood circulation in the central nervous system (Cinnarizine), they are prescribed both orally and intravenously; in addition, they promote the resorption of thromboaggregates;
- drugs that prevent the accumulation of insoluble protein fractions in the refractive structure of the eyes (Quinax);
- local vitamin therapy using medicinal drops, which enhance metabolism, leading to increased regenerative capacity (Okovit, Taufon).
Even with the use of conservative therapy, the patient’s condition progresses, the doctor immediately performs surgery to eliminate opacities in the vitreous body:
- Vitreolysis. This is a laser procedure that is aimed at eliminating vitreous opacities. The technique is used for patients who have severe myopia and a high risk of retinal detachment. Anesthetics are first instilled into the patient's eyes. The entire procedure is performed without general anesthesia. Using a laser, areas of accumulation of fractions of various substances are removed. But the technique is applicable only if the clouding does not form strongly and is focally distributed throughout the vitreous body.
- Vitrectomy. This is a major surgical procedure in which the vitreous humor is removed completely or partially. The first option is suitable for those people whose clouding has spread throughout the entire structural element of the eyes. The internal structure of the vitreous body is easily replaced by an artificial environment that fully corresponds to its own element. Partial removal of the vitreous is only suitable if the clouding has developed in a certain area and greatly reduces visual acuity. With partial removal, the doctor does not need to replace the fluid with an artificial medium; it will recover on its own, since the eye medium circulates constantly.
Most often, silicone oil, saline solution, and gas elements are used to replace the structure of the vitreous body. They are identical in composition and do not form a negative reaction of the immune system, which can lead to an inflammatory condition.
Gradually, the fluid necessary to replace the internal component of the vitreous body is replaced by the eye’s own secretion. This is due to the fact that fluid in the organs of vision constantly circulates. But the effect is observed only when using saline solution or gas bubbles. If the doctor chose silicone oil, the patient will need a second operation after 5 years.
Anatomy of the vitreous
- Structure
- Pathologies
- Diagnosis of vitreous diseases
The vitreous body is a complexly organized tissue structure of viscoelastic consistency with the presence of an exchange-transport system, 99% consists of water and 1% is vitrosin and mucin. The vitreous body does not regenerate and, if partially lost or surgically removed, is replaced by intraocular fluid.
Functions
- giving the eye the correct (spherical) shape;
- conduction and refraction of incoming light onto the retina of the eye;
- maintaining intraocular pressure levels
- ensuring the incompressibility of the eye.
- ensuring the normal location of intraocular structures, including the retina and lens
- compensation for changes in intraocular pressure due to sudden movements or injuries due to the gel component
This substance is necessary already in the prenatal period - the hyaloid artery passes through it, which nourishes the lens and part of the anterior segment of the eye. With age, in the final phase of lens formation, this artery spontaneously disappears, although sometimes in adults its remains are found in the form of tender cords. The vitreous plays a leading role in the maturation of the retina and the organization of its blood supply.
There are no vessels or nerves in the vitreous body. The vital activity and constancy of its environment is ensured by osmosis and diffusion of nutrients from the intraocular fluid through a vitreous membrane with directional permeability. The vitreous body has low bactericidal activity; leukocytes and antibodies are detected in it only some time after infection.
The vitreomacular interface is the area of contact between the vitreous and the retina. The pathology of the vitreomacular interface is of no small importance in the development of various diseases of the posterior segment of the eyeball. The vitreous body (VF) structures have the greatest influence on the state of the vitreomacular interface.
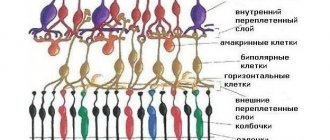
Structure
The volume of the vitreous body is only 3.5-4.0 ml, the vitreous body is somewhat flattened in the sagittal direction, depending on the general shape of the eyeball. It is located behind the lens and ligament of cinnamon and makes up the majority of the contents of the eyeball (65%), coming into external contact with the flat part of the ciliary body, and throughout the rest of the length with the retina; posteriorly, the vitreous body is in contact with the optic disc.
The ST structure includes:
- Zones, ligaments – areas of increased density;
- Gaps are areas of low density;
- The cortex is a zone of compaction; it is a condensation of fibrils with cells.
The vitreous body is a conductor of the intraocular fluid produced by the ciliary body during its outflow. Part of the fluid into the vitreous body comes from the posterior chamber, being absorbed further, directly into the vessels of the retina, as well as the optic nerve head.
On the anterior surface of the vitreous body there is a depression (fossa patellaris) corresponding to the location where the posterior surface of the lens adjoins it. The edges of the recess form a low shaft and are connected by a fibrous ligament (lig. hyaloideum) with the lens capsule along its equatorial part.
The connection between the vitreous body and the membranes of the eye is strongest anterior to the dentate line, along the flat part of the ciliary body. This area is called the base of the vitreous. When the vitreous body is detached, it takes the ciliary epithelium with it.
Another place of the tightest connection between the vitreous body and the retina is the periphery of the optic nerve and the area of the macula. With limited detachment of the vitreous, the internal limiting membrane is often separated along with it.
Three zones are topographically distinguished in the vitreous body:
- retrolenticular part (pars retrolenticularis); - capillary gap between the lens and the vitreous body
- ciliary part (pars ciliaris);
- back part (pars posterior).
Scheme of the topography of the tract system 1 - Cloquet's canal, 2 - extralental part of the PGM, 3 - posterior zonular fibers, 4 - anterior base of the CT, 5 - lens, 6 - posterior chamber of the eye, 7 - preoral ciliary epithelium, 8 - retina, 9 - optic disc , 10 - Weger's hyaloid-capsular ligament, 11 - Salzmann's zonular fissure, 12 - retrolental part of the PGM, 13 - upper wall of the CC, 14 - lower wall of the CC, 15 - angle of the inferior fold, 16-18 - vitreal tracts
With careful separation of the membranes of the eye, the exposed vitreous body does not spread, but retains its shape even when a load is placed on it. This indicates the presence of its own outer shell.
The delicacy of the structure of the vitreous body has until now created a number of difficulties in its microscopic study: the vitreous body, easily wrinkled during fixation, produced significant deformation that distorted its true structure. Modern intravital methods of studying the vitreous body (using a phase-contrast microscope, ultramicroscope and electron microscope) have made it possible to establish with certainty the fibrillar structure of the vitreous body.
Interfibrillar spaces are filled with liquid, viscous, amorphous content. The peripheral condensed layers of the vitreous consist of long, very thin and delicate submicroscopic transparent fibrils. In the area of the base of the vitreous body they are located more densely, which corresponds to the posterior boundary layer, which gradually thins posteriorly.
In front, the vitreous body is also compacted, which corresponds to its anterior boundary layer. It also forms the limiting membrane (membrana hyaloida). The latter, towards the lens in the center, becomes very thin and disappears almost to nothing, corresponding to the posterior pole of the lens. With age, the boundary layer becomes increasingly denser.
The membrane limiting the vitreous body is divided into posterior (posterior to the dentate line) and anterior (anterior to it). The anterior hyaloid membrane is divided into retrolental and zonular regions, the border between them is the Viger's ligament, which runs from the membrane to the lens capsule. The posterior hyaloid membrane is tightly fused to the retina along the edge of the optic nerve head, as well as at the dentate line; it is less tightly attached to the blood vessels in the retina.
Inside, the vitreous body is divided by the so-called funnel-shaped complexes, or vitreal tracts - preretinal, median, coronary and hyaloid. The coronary and median tracts arise from the zonular region of the anterior hyaloid membrane, which stabilizes the anterior region of the vitreous during movement of the eyeball. All tracts are curved in an S shape, with the exception of the preretinal one.
The cortical layer of the substance contains cells - hyalocytes, which synthesize reticulin and hyaluronic acid, necessary to maintain the constituent vitreous body. Certain cavities can form in the cortical layer, which, when the retina breaks, also easily rupture, contributing to the further development of detachment.
Somewhat nasally from the central axis of the eye, the so-called Cloquet canal (canalis liyaloideus Cloquet) passes through the vitreous body, which contained a. hyaloidea. This is the largest central S-shaped canal connecting the retrolental space (Berger's space) with the prepapillary space (Martegiani's space). Its ending is located slightly closer to the nose from the posterior pole of the lens. The cloquet canal is better expressed in children. Its presence in adults is disputed by some authors. However, the appearance of exudate on the optic nerve nipple during iridocyclitis can only be explained by the presence of the Cloquet canal.
Through the Petri canal and Hanover canal, which are located in the zonular part of the anterior cortical layers of the CT, aqueous humor enters the retrolental space into the posterior chamber of the eye.
According to Worst JGF. (1975) on both sides of the central canal are the lenticomacular and optociliary canals. The lenticomacular canal connects the retrolental space with the premacular bursa, and the optociliary canal connects the prepapillary region with the retrociliary cisterns of the CT. The channels communicate at the level of the premacular bursa and prepapillary space through a connecting canaliculus. Valve mechanisms in the optociliary canal provide directional movement of aqueous humor from the anterior sections of the ST to the optic nerve head.
According to Abdullin E.A. (2008) and Baranova E.V. (1987) systems of retrociliary, equatorial and petaliform cisterns provide the metabolism of the vitreous itself and the intraocular structures in contact with it. Retrociliary cisterns are cylindrical cavities that communicate with each other and form a ring in the projection of the ciliary body. The retrociliary cisterns are located in the form of a ring on the anterior, somewhat concave surface of this dense frame; the equatorial and petaliform cisterns are located in its thickness, oriented around the central cone of the vitreous body formed by the canals.
A thin layer of the vitreous cortex is tightly adjacent to the surface of the retina, which thickens with age. In front of it, above the macula, there is a liquefied layer (precortical vitreal pouch), followed by the vitreal gel itself. The precortical vitreal recess (premacular bursa) is a closed cup-shaped cavity that looks like a truncated oval from the retinal side, the anterior wall of which is formed by an intravitreal membrane pierced by multiple holes. The posterior wall of the bursa is formed by a thin membrane of the CT, which is covered from the inside by a layer of spongy substance (vitreal cortex) with the exception of the area corresponding to the foveal zone of the retina
Changes with age
In newborns, the vitreous body is a homogeneous gel. With age, for reasons not fully known, degeneration of the vitreous body occurs, leading to the clumping of individual molecular chains into large clusters. Homogeneous in infancy, the vitreous body is divided into two components with age - an aqueous solution and clusters of chain molecules. In the vitreous body, water cavities and floating clusters of molecular chains, visible to the person himself in the form of “flies,” are formed. Ultimately, this process causes the posterior surface of the vitreous to detach from the retina. This can lead to a sharp increase in the number of floating clouds - floaters. In itself, such a vitreous detachment is not dangerous, but in rare cases it can lead to retinal detachment.
Modern research
Currently, methods for culturing hyalocytes have been developed, which they hope to use to create an artificial vitreous body, devoid of the disadvantages of silicone and other fluids currently used after vitrectomy.
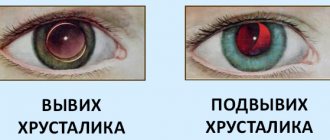
Pathologies
Vitreous opacities can be divided into: pretrolental (behind the lens), central, combined and preretinal.
Genetically determined pathologies:
- Remains of an embryonic artery that supplied the lens with blood during the prenatal period.
- Primary persistent vitreous.
Acquired pathologies:
- Liquefaction of the vitreous body.
- Destruction of the vitreous body.
- Vitreous opacification.
- Vitreous hernias.
- Hemorrhages into the vitreous body (hemophthalmos).
- Inflammatory changes in the vitreous body (endophthalmitis or panophthalmitis).
- Posterior vitreous detachment, in which the membrane is disrupted at the attachment sites, with liquid vitreous spreading into the area between the posterior hyaloid membrane and the retina; the appearance of a tight junction of the membrane in the macula area with the development of retinal traction, leading to decreased vision.
As a rule, most pathologies of the vitreous body manifest themselves as floating opacities in the form of dots, blots, threads of various sizes, etc. A decrease in visual acuity can occur with severe hemorrhage or severe inflammation, as well as traction in the macular zone.
Diagnosis of vitreous diseases
- Visometry
- Biomicroscopy – assessment of the condition of the anterior segment of the vitreous body under a microscope.
- Ophthalmoscopy - detection of changes in the preretinal sections and the posterior segment of the vitreous body.
- Optical coherence tomography - search for changes in the relationship of the retina in the area of the macula and the posterior hyaloid membrane for retinal traction.
- Ultrasound diagnostics
Prevention
There are many different prevention methods that can be used to prevent the formation of cloudiness in the optical media of the eye:
- timely treatment of viral, infectious, fungal diseases of the eyeball;
- timely treatment of systemic diseases that can lead to complications for the eyes, causing visual impairment due to the accumulation of insoluble substances;
- normalization of nutrition, which should include all useful substances, and also reduce the amount of insoluble proteins;
- treatment of endocrine diseases through hormone replacement therapy;
- taking medications prescribed by a doctor;
- In case of mechanical eye damage, consult a doctor and avoid self-medication, which may worsen the situation.
The preventive measures used will not completely eliminate the risk of developing vitreous opacities. This is due to the fact that the pathological condition may be a consequence of the physiological process that forms aging in people after 50 years of age. But the use of preventive measures will significantly reduce the possibility of complications.
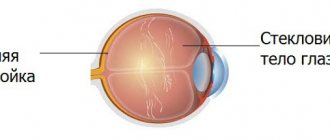
Structure
Externally, the vitreous body of the eye resembles a thick gel. It is located behind the lens, being part of the eyeball. There are numerous channels and blood vessels inside it. The protective membrane lining the outside of the organ protects it from injury or other external influences.
The vitreous body contains an artery that supplies the retinal tissue. It is formed during the prenatal period of a child’s life, and is located in the cloquet canal, which externally resembles a microscopic tube.
It is through the cloquet canal that the artery that supplies the retina passes. Among other things, the gel-like substance contains hylauronic acid, which maintains moisture balance and fibrils.
Method of performing vitreolysis
In case of destruction of the vitreous body, vitreolysis is performed on an outpatient basis after preliminary drip anesthesia. This helps to avoid additional stress on the heart and blood vessels. Drops are also used to dilate the pupil. Next, a three-mirror Goldmann lens is placed on the eye, which focuses the laser beam in a given area of the vitreous. During the treatment, no incisions are made, and there is no blood loss or pain. The patient hears the doctor's work and feels the touch, but nothing more. After vitreolysis, the doctor observes the patient for some time and then sends him home.
Eyeball
The eyeball occupies the main place in the orbit or orbit, which is the bony seat of the eye and also serves to protect it. Between the orbit and the eyeball there is fatty tissue, which performs shock-absorbing functions and contains blood vessels, nerves and muscles. The eyeball weighs about 7 grams.
Eyeball
is a sphere with a diameter of about 25 mm, consisting of three shells.
The outer, fibrous membrane consists of an opaque sclera
about 1 mm thick, which passes into the cornea in front.
On the outside, the sclera is covered with a thin transparent mucous membrane - the conjunctiva.
.
The middle layer is called choroid
. From its name it is clear that it contains a lot of vessels that nourish the eyeball. It forms, in particular, the ciliary body and the iris. The inner layer of the eye is the retina.
Eye muscles
The eye also has an appendage
, in particular, the eyelids and lacrimal organs.
Eye movements are controlled by six muscles
- four rectus muscles and two oblique muscles. In terms of their structure and functions, the eyes can be compared to the optical system of, for example, a camera. The image on the retina (analogue of photographic film) is formed as a result of the refraction of light rays in the system of lenses located in the eye (cornea and lens) (analogue of a lens). Let's look at how this happens in more detail.