Why does anisometropia develop?
Anisometropia is a visual impairment in which the clinical refraction of the two eyes does not match, and the power of the optical lenses of one eye is significantly greater or less than the other.
Predisposing factors
Anisometropia can be congenital or acquired .
The most common form is the congenital form, which can be detected already during a medical examination of the child a year. But often low-grade anisometropia is ignored by doctors and patients due to the lack of complaints, until they appear in adulthood.
Acquired anisometropia can appear after an eye disease, surgical treatment or severe trauma.
Immediate causes
In childhood, the immediate cause of anisometropia is the uneven development of the two eyes relative to each other or a lag in the development of one eye against the background of the normal development of the other.
Normally, a child is born with large hypermetropic refraction (farsightedness), which decreases significantly by the end of the first year of his life (down to 1-2 diopters) and turns into normal zero refraction (emmetropia) by about 6-8 years.
If at any stage of development of the organ of vision an error occurs, and one eye begins to grow faster or slower than the other, their length and optical power cease to be the same, they refract the light beam differently, and anisometropia occurs.
If eye development occurs normally, and during routine examinations by an ophthalmologist no difference was detected in the two eyes, then in adulthood anisometropia can develop only after an injury or disease, for example, unilateral cataracts.
Causes
The disease can be congenital or acquired.
In the first case, the pathology is associated with a hereditary predisposition. The most common cause of anisometropia in this form is considered to be congenital unilateral myopia. After the development of the visual organ in children is completed, the symptoms usually disappear on their own.
In the case of the acquired form, the main causes of the disease are considered to be:
- Development of cataracts: light rays do not pass through the cloudy environment of the optical system, causing vision impairment in the affected eye.
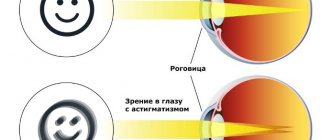
- Astigmatism: occurs due to abnormal shape of the cornea or lens and increases blurred vision.
- The appearance of high degree of farsightedness in 1 eye: this condition is typical for older people who have already developed glaucomatous disorders in the organ of vision.
- The development of complications after eye surgery: as a result of interventions performed on the retina, vitreous body or lens in the postoperative period, a violation of the refractive ability of the eye appears.
What happens to the organ of vision with anisometropia?
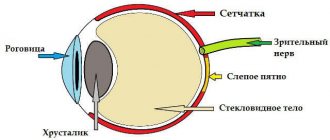
What happens next? Due to the fact that the optical power of the two eyes differs from each other, ametropia of the eye occurs - a condition in which the image does not fall on the retina, but is projected in front of or behind it. Because of this, the image becomes blurry, without clear contours.
The retina processes the image data into a nerve impulse, which travels along the optic nerve to certain areas of the brain, and there the resulting material is carefully processed.
Normally, the brain should combine pictures from the right and left eyes into a single image. And since the retinas of our eyes receive different images during anisometropia - one is bright, the other is blurry, one is large, the other is smaller, the brain is not able to combine these pictures into one. Then he “selects” the image that is clearer and brighter, and does not use the other, low-quality image at all.
Gradually, the connection with the worse-seeing eye is lost, and it will not be possible to restore it in the future. Therefore, it is important to timely identify this pathology and correct it.
Symptoms of macular degeneration
Patients often ask how to recognize the approach of a dangerous illness in time. This, indeed, poses a particular problem since each form of macular degeneration has its own characteristics. The dry form is more common, but is more difficult to diagnose as its clinical picture is characterized by the absence of pain. The disease is rarely accompanied by an acute and violent onset; the classic development of the disease occurs slowly and is initially unnoticed by the person.
Ophthalmologists advise not to ignore the following signs, which are the first symptoms of macular degeneration:
- The appearance of difficulties when reading, writing, performing delicate work with small details in the previous glasses or lenses. For example, women find it difficult to thread a needle.
- Decreased visual acuity at distance and near.
- The appearance of dark spots with unclear boundaries before the eyes.
- Difficulty recognizing faces.
- Poor orientation in poor lighting conditions.
- Distortion of the contours of objects and printed text.
- Deterioration of color perception.
- Feeling of insufficient lighting.
The higher the stage of the disease, the more pronounced the symptoms. Sometimes such manifestations affect only one eye, while the entire visual load falls on the healthy eye and sometimes the patient does not notice any changes, this distorts the clinical picture and complicates the diagnosis.
If macular degeneration of the eye is suspected, each person can perform a self-diagnosis using the Amsler test. The essence of the test for macular degeneration of the retina is to examine an image in the form of a grid of straight lines with a black dot at the intersection. If a healthy person sees straight lines, then a patient with retinal dystrophy sees straight lines as broken, blurry, wavy, and dark spots appear in the perimetry. This effect is explained by the accumulation of fluid under the macula, as a result of which it rises and causes distortion of the contours of objects.
The wet form of macular degeneration is characterized by more pronounced symptoms:
- Rapid loss of central vision.
- Enlargement of the blind spot in front of the eyes.
- Distortion of straight lines and outlines of objects.
During a comprehensive examination in the ophthalmologist’s office, to confirm the patients’ complaints, the detection of yellow deposits under the retina, in other words, drusen, is added. A relationship has been established between the number and size of drusen and the degree of dry or wet macular degeneration.
Classification
Due to development, there are three types of anisometry.
- Axial anisometry , in which the optical power of the two eyes is the same, but the length of the anteroposterior axis of the eyeball differs.
- Refractive anisometropia , in which the sizes of the eyes do not differ from each other, but the degree of refraction and optical power are different.
- Mixed anisometropia , in which both refractive power and anteroposterior ocular size differ greatly in the two eyes.
There are three degrees of anisometropia:
- weak, in which the difference in refraction between the two eyes is less than 3 diopters;
- average, when the difference between the right and left eyes is a total of 3 to 6 diopters;
- high, in which the refraction of the eyes differs by more than 6 diopters.
Symptoms of anisometropia
Most often, a doctor may suspect anisometropia when the patient complains of:
- rapid eye fatigue;
- discomfort while reading;
- pain in the eyes and headaches with prolonged visual stress.
It is worth contacting an ophthalmologist if you have the above complaints or:
- ghosting;
- unclear boundaries of surrounding objects;
- if you yourself notice that one eye sees worse than the other.
In young children, it is quite difficult to independently suspect different vision in their eyes. You should immediately contact an ophthalmologist if parents begin to notice that:
- the child brings toys close to his eyes;
- does not notice planes flying in the sky;
- one eye begins to squint towards the nose or temple.
Clinical manifestations
Otohematomas form quickly or enlarge within a few days. They are located at the top of the ear, on the outside. Neoplasms can occupy the entire surface of the outer ear.
Typical symptoms of otohematoma:
- the appearance of a round protrusion under the skin;
- redness of the skin over the damaged area, there is a bluish tint;
- if the formation is filled with lymph, the skin retains its natural color;
- thickening, swelling of the auricle, smoothing of the contours.
Important: Hematomas of traumatic origin are painful, and the pain worsens when palpating the ear. Spontaneous hemorrhages do not cause discomfort.
Diagnostics
Anisometropia code according to ICD 10 – H52.3
Diagnosing anisometropia at the moment does not present any particular difficulties. It is enough for an ophthalmologist to check the patient’s vision and conduct a special computer examination - autorefractometry, which will indicate the refraction of the right and left eyes. In children, due to the complexity of computer studies, retinoscopy or skiascopy is performed.
After the diagnosis, the doctor will select various spectacle lenses that will increase visual acuity in the worse-seeing eye and decide whether permanent optical correction (glasses or contact lenses) is needed or whether another method of treatment is possible.
If spectacle lenses do not improve vision, then the range of studies is expanded to include ultrasound of the organ of vision and orbit, examination of the fundus (ophthalmoscopy), and study of visual fields (perimetry).
Treatment
Treatment. For mild and moderate myopia, as a rule, full or almost complete optical correction for distance and weaker (by 1 - 2 diopters) lenses for working at close distances are used. With a high degree of myopia, constant correction is required, the amount of which for distance and near is determined according to tolerance. If glasses do not sufficiently improve visual acuity, contact correction is recommended. Exercises for the ciliary muscle to improve accommodative ability. Careful observance of visual hygiene at school and at home (sufficient lighting of the workplace, correct posture when reading and writing, etc.), systematic physical education and sports (as prescribed by a doctor!), correct daily routine, frequent alternation of visual stress with rest for the eyes (every 30 - 40 minutes of exercise, 10 - 15 minutes of rest, preferably in the fresh air). As myopia progresses, drug treatment is prescribed: calcium gluconate 0.5 g 3 - 6 times a day for 10 days, ascorbic acid 0.05 - 0.1 g 2 - 3 times a day for 3 - 4 weeks, nicotinic acid 0.005 - 0.05 g 3 times a day for 20 days, halidor 0.05 - 0.1 g 2 times a day for 2 - 3 weeks. For chorioretinal complications - nigexin 0.125 - 0.25 g 3 times a day for a month, tren-tal 0.05 - 0.1 g 3 times a day after meals for a month, riboflavin 0.002 - 0.005 g 2 - 3 times a day for 1 - 1.5 months, subconjunctival injections of 0.2% ATP solution, 0.2 ml daily or every other day, 10 - 12 injections; theophylline 0.05 - 0.1 g with nicotinic acid 0.02 - 0.1 g 2 - 3 times a day 2 - 3 days in a row with a break of 2 - 3 days, for a total of 10 - 15 days; tissue preparations, preferably a suspension of the placenta, 1 ml subcutaneously, once every 7 - 10 days, for a course of 3 - 4 injections (tissue preparations should not be prescribed during puberty). For the prevention and treatment of hemorrhage - rutin 0.02 g with ascorbic acid 0.05 - 0.1 g 2 - 3 times a day or ascorutin 0.05 g 2 - 3 times a day for 3 - 4 weeks; aminocaproic acid 0.5 g 2 - 3 times a day for 3 - 5 days, vikasol 0.01 - 0.02 g 2 times a day for 3 - 4 days. If opacities appear in the vitreous body, intravenous infusions of 20 ml of 40% glucose solution with 2 ml of 5% ascorbic acid solution (20 infusions), then sodium iodide 0.3 - 1 g 3 - 4 times a day for 10 - 15 days . With rapid progression of myopia - sclera-strengthening operations or SSI (sclero-strengthening injection). For myopic astigmatism and anisometropia (when optical correction cannot be tolerated), refractive surgery on the cornea is possible.
Forecast. With stationary uncomplicated myopia, vision is well corrected with glasses. The visual prognosis worsens as myopia progresses and complications occur.
Prevention. General strengthening of the body. Limitation of visual work at close range. Compliance with all visual hygiene requirements. Training the ciliary muscle with weakened accommodation. Elimination of pseudomyopia.
Diagnosis code according to ICD-10 • H52.1
Approaches to the treatment of anisometropia. Correction methods
It is worth understanding that anisometropia itself needs to be corrected, not treated . It will not be possible to change it or completely get rid of it, since it is not exactly a disease, but rather a condition, and only its consequences and complications can be treated.
If anisometropia is detected in childhood, treatment should not be delayed indefinitely. The sooner the correction is prescribed, the greater the chance that visual acuity will improve.
The selection of spectacle or contact correction for children under 16-18 years of age must be accompanied by cycloplegia - the instillation of special drops that dilate the pupil and allow the degree of change in refraction to be assessed most accurately.
If a patient has completely different vision in his eyes, the best method of correction in this case is contact lenses or refractive surgery . Glasses can help only with a weak degree of anisometropia, since with a large difference in the glasses, the frame is poorly and awkwardly positioned on the face, and it warps. At the same time, the optical center of the glass lens shifts, and there is no longer any sense in wearing glasses.
Contact lenses cannot move enough without the patient noticing. In addition, a contact lens can be worn only on one eye, which is important if there is no disease in the other eye.
Laser vision correction or other refractive surgery is allowed from the age of 18, since it is believed that until this time the eye continues to grow and a change in refraction is possible. In some situations, with high degree anisometropia, ophthalmology clinics undertake this operation in children, but for this a number of conditions must be met.
Anisometropia :: Symptoms, causes, treatment and code according to ICD-10
Title: Anisometropia.
Anisometropia
Anisometropia.
This is a pathology of clinical refraction of the eye, in which the difference in refractive power between the eyeballs exceeds 2 diopters. The disease is manifested by diplopia, blurred images before the eyes, decreased visual acuity, and rapid fatigue when performing visual work.
To make a diagnosis, visometry, ultrasound, computer refractometry, perimetry, biomicroscopy, ophthalmoscopy, and skiascopy are used.
Treatment tactics boil down to correction of visual dysfunction using contact lenses, glasses, or the use of surgical methods (excimer laser intrastromal keratomileusis, IOL implantation).
Anisometropia refers to a group of refractive errors. According to statistics, the prevalence of pathology in the structure of all diseases of the organ of vision is 17%. It has been proven that differences in the refractive power of the eyes are more common in children than in adults.
At the age of seven, the disease is diagnosed in 8% of schoolchildren; by the age of ten, this figure reaches 17%. During the process of refractogenesis, only in 38.2% of children the clinical manifestations remain stable, in 25.5% of patients there is a regression of symptoms, in 36.3% the severity of symptoms increases.
In European countries, 1.5% of the population suffers from this disease, in China – 4%.
Anisometropia
In most cases, anisometropia is based on organic pathology of the organ of vision. Functional changes lead to a slight increase in the refractive difference, which is not accompanied by clinical manifestations. The main causes of the disease: • Cataract.
The cause of the pathology is clouding of the lens, which is associated with disruption of the passage of light rays through the optical system and visual dysfunction of only one eye. • Congenital unilateral myopia.
Myopia is the most common cause of anisometropia in children.
In some cases, after the formation of the eyeball is completed, the symptoms disappear on their own. • Astigmatism.
The development of this pathology is often caused by a violation of the shape of the lens or cornea in the case of asymmetric changes.
• Unilateral high degree of hyperopia.
Asymmetrical farsightedness is more often detected in patients over 40 years of age due to the development of glaucomatous changes. • Iatrogenic effects.
Clinical refractive errors occur in the postoperative period, which is caused by surgical interventions on the lens, vitreous body, and retina.
It has been proven that implantation of intraocular lenses (IOLs) before the age of 18 leads to ametropia and anisometropia in adulthood.
When the difference in refractive power of both eyes exceeds more than 2 diopters, binocular vision disorders occur. With a long course of the disease, the clinical picture of secondary strabismus increases.
Normally, the image is formed as one whole with the participation of the retina of the two eyes and the brain. Different refraction causes the image on the retina to become deformed and the patient sees it “blurry”.
In this case, the patient compensatory limits the participation of the less visually impaired eye in the act of vision. If the size of the longitudinal axis is abnormal, the accommodative ability is impaired.
If the symptoms are caused by a pathology of refraction, then the position of the nodal points changes, which also complicates the formation of an image on the inner shell. The decrease in visual acuity is reversible, as it is caused by a spasm of accommodation.
There are congenital and acquired anisometropia. The disease can develop independently or be a manifestation of other ophthalmic pathologies. According to the clinical classification, the following forms of the disease are distinguished: • Axial.
The reason for the occurrence of this variant is a pathological change in the long axis of one of the eyeballs, subject to the same refraction.
• Refractive.
With this form, the longitudinal axis is normal, but the clinical refraction of one eye is 2 or more diopters greater than the other.
• Mixed.
It is characterized by a combination of manifestations of the axial and refractive variants of the disease. There are three degrees of severity of anisometropia:
• Weak degree.
Up to 3 diopters.
• Medium degree.
3 – 6 diopters.
• High degree.
More than 6 diopters.
The main clinical manifestations of anisometropia are caused by impaired binocular vision. Differences in the refractive power of the eyes of less than 2 diopters are mild and in rare cases can lead to minor visual discomfort. The use of spectacle correction ensures normal visual acuity.
With a moderate degree of the disease, patients complain of double vision, blurred contours of images before the eyes, and decreased visual function. Anisometropia is characterized by the disappearance of symptoms when one eye is closed.
Parents often note that their child squints when reading, watching TV or working at the computer.
An earlier complication of anisometropia is amblyopia, which is caused by a deliberate restriction of the affected eye's participation in vision. In the absence of timely diagnosis and treatment, convergent or divergent strabismus develops.
Long-term wearing of contact lenses leads to microdamage to the cornea, keratitis, epithelial edema, iris rubeosis and corneal neovascularization. There is an increased risk of developing infectious and inflammatory diseases of the anterior part of the eyes (conjunctivitis, blepharitis, iritis).
A specific complication of the pathology is anisoaccommodation, which is characterized by different accommodative abilities of the eyes.
Often, objective signs of anisometropia are detected accidentally during an ophthalmological examination. Patients seek help from a specialist only with moderate and severe disease. The diagnostic plan includes: • Computer refractometry.
The technique is used to determine the type of clinical refraction and study the ratio of refractive power to the longitudinal axis. • Visometry.
Allows you to determine the degree of decrease in visual acuity.
• Ultrasound of the eye.
Used to measure the anteroposterior axis of the eyeball.
Ultrasound examination is necessary for opacified optical media to visualize the vitreous body, retina and optic nerve. • Ophthalmoscopy.
During the examination of the fundus, you can study the condition of the inner membrane, the optic nerve head.
• Perimetry.
An additional research method that allows you to identify asymmetrical narrowing of the visual field according to the concentric type. • Biomicroscopy of the eye.
Examination of the anterior part of the eye is informative for determining the etiology of the disease, identifying the first signs of secondary inflammation of the cornea and bulbar conjunctiva.
• Skiascopy of the eye.
The shadow test is an alternative method for studying clinical refraction, which makes it possible to measure the ratio of the anteroposterior size to the refractive power of the optical system. In individuals with anisometropia, the darkening moves in the direction of rotation of the ophthalmoscopic mirror.
Etiotropic therapy is reduced to eliminating the manifestations of the underlying disease. Conservative methods for correcting visual acuity are used in patients with mild to moderate pathology. If the difference in the corrective glasses should exceed 2.5 diopters, surgical intervention is indicated.
The following methods are used to treat anisometropia: • Correction of visual acuity.
To correct visual functions, special telescopic glasses can be used, the optical system of which consists of collecting and diverging lenses. The indication for their use is organic damage to the visual analyzer.
For high-grade anisometropia, iseikonic glasses are prescribed. Symptomatic therapy is based on the selection of contact lenses. In childhood, they are used only if there are contraindications to surgical treatment and spectacle correction. • Surgical correction.
In the absence of lesions of the cornea, excimer laser intrastromal keratomileusis is effective. An alternative option for keratorefractive surgical correction is the implantation of an additional IOL.
In this case, the density of endothelial cells should not be lower than the minimum limits corresponding to age standards. In patients with high myopia, laser coagulation of the retina is performed a month before surgery.
The prognosis for life and work ability is favorable.
Specific methods of prevention have not been developed. Nonspecific preventive measures are limited to monitoring visual acuity and clinical refraction.
Persons who have undergone eye surgery over the past 2 years are advised to consult an ophthalmologist once every 6 months with mandatory refractometry and visometry.
When diagnosing clinical refractive errors in children over 1 year of age, it is necessary to carry out timely correction of visual dysfunction in order to prevent the development of strabismus. In patients younger than 12 months, the use of special treatment methods is not indicated.
42a96bb5c8a2ac07fc866444b97bf1 Content moderator: Vasin A.S.
Source: https://kiberis.ru/?p=33054
Complications of anisometropia
If left untreated, especially in early childhood, anisometropia can lead to serious consequences. Since the part of the brain responsible for vision receives a sufficient amount of information from one eye, and a blurred picture comes from the second, the brain gradually “turns off” the poorly functioning eye, the nerve connections between them are functionally lost, and vision continues to deteriorate.
Because of this, strabismus and amblyopia occur, known to us as “lazy eye,” and this is a more serious disease. The sooner treatment is started, the greater the chance that vision will be restored, and strabismus will not have to be corrected surgically.
In adult patients, anisometry can lead to diplopia - double vision of surrounding objects, which can be accompanied by dizziness, headache and eye pain. The presence of complaints will be affected by the degree of ametropia, but even with a slight blurring of the incoming information, discomfort in the eyes is possible. After prescribed optical vision correction, in the absence of concomitant pathology, the complaints cease to be a concern.
Otohematoma - treatment and diagnosis
To diagnose an otohematoma, examination is sufficient, since the formation is visible to the naked eye. However, the doctor takes a puncture of the contents to determine the presence of pus. In addition, additional examinations for spontaneous hematomas are indicated to determine the cause.
The following methods are used to treat otohematoma:
- compression bandage – worn for minor hemorrhages;
- puncture of the contents - prescribed to remove fluid from formations that arose less than 3 days ago;
- surgical opening of the hematoma;
- Antibiotic therapy is necessary if there is a risk of bacterial infection.
Antibiotics are indicated for any treatment option for auricular hematomas. They are prescribed in the form of tablets, and are also added to preparations for treating the cavity after removing the contents.