Total information
Angular conjunctivitis is diagnosed in 5-7 patients out of a hundred who have been diagnosed with inflammatory damage to the mucous membrane of the eye. Acute forms are rare - about four-fifths of all patients with angular conjunctivitis suffer from chronic pathology.
This disorder is detected at any age, but more often in middle and old age. The incidence begins to increase after 40 years, after which its peaks are not observed. Complications are also more common in older age, when involutive tissue changes begin.
Males and females get sick with approximately the same frequency - this pattern applies to both young and elderly patients.
Differences between bacterial and viral conjunctivitis
Bacterial and viral conjunctivitis have a number of differences:
- Conjunctival injection in the bacterial form is pronounced, while in the viral form it is minimal.
- Exudate. With bacterial - from moderate to profuse. With a virus, minimal.
- The bacterial form is characterized by glued edges of the eyelids and eyelashes, but the viral form does not stick together.
- Also, with the viral form, there are no papillae, and the effect of antibacterial therapy is absent, but, unlike the bacterial form, follicles appear.
- The viral form is cured faster than the bacterial form.
Causes
It was previously assumed that angular conjunctivitis is caused by staphylococci and streptococci. But the direct cause of the development of the described disease turned out to be Moraxella lacunata (Morax-Axenfeld diplobacillus).
The pathogen consists of short rods, which are arranged in twos - in turn, such pairs make up short chains. This is a gram-negative rod - it does not stain when stained with Gram (one of the most informative ways in microbiology to distinguish pathogens).
Diplobacillus Morax-Axenfeld belongs to the category of strict aerobes - that is, those bacterial pathogens that need to be in an environment with free molecular oxygen to survive. It is required for processes that release the energy required for the reproduction and pathogenic activity of the pathogen.
This infectious agent is immobile - due to the specific structure and energy processes, it is not endowed with the ability to move independently in tissues.
note
Among other representatives of the genus, the causative agent of angular conjunctivitis is distinguished by its high virulence (the ability to cause a pathological process).
Diplobacillus Morax-Axenfeld lives on the mucous membranes of the human body - namely:
- on the conjunctiva (most often);
- among the epithelial cells of the paranasal sinuses;
- in the superficial layer of the endocardium (inner layer of the heart).
This means that signs of conjunctivitis, inflammation of the mucous membrane lining additional nasal cavities, and endocarditis may simultaneously appear.
Diplobacillus Morax-Axenfeld is an opportunistic microorganism. This means that normally it can inhabit the mucous membranes of a healthy person without harming him and living his life. But under certain conditions, the pathogen exhibits aggressive properties and provokes the development of the disease - in this case, angular conjunctivitis. These conditions are:
- decreased immunity due to congenital and acquired immunodeficiencies;
- condition after previous operations - especially protracted abdominal operations (on the abdominal or thoracic cavity);
- early period after injury or critical condition (coma);
- chronic, long-term somatic pathologies - coronary heart disease (oxygen starvation due to atherosclerotic damage to the heart vessels), bronchial asthma (damage to the bronchi with their periodic narrowing and the occurrence of asthma attacks), peptic ulcer of the stomach and duodenum (the occurrence of single or multiple defects in the wall of the stomach or intestines), diabetes mellitus (impaired carbohydrate metabolism due to lack of the hormone insulin);
- psychological exhaustion – due to stress, inappropriate moral conditions in the family, at work and/or in society;
- heavy physical labor for a long time;
- poor nutrition with insufficient intake of proteins, fats, carbohydrates, and minerals;
- following exhaustive diets;
- conscious (if you want to reduce your own weight) or forced fasting (for example, with cancer of the esophagus or stomach, which interferes with the normal process of digestion and the flow of nutrients into the tissues);
- inappropriate living conditions or lack of a specific place of residence;
- lactation;
- older age. The bacillus can live on the mucous membranes of some people for a long time, without causing any problems, and then become active only when the person ages.
Diplobacillus Morax-Axenfeld can exist for some time outside the human body. Thus, thanks to its resistance to adverse environmental conditions, it is able to support life at temperatures from 10 degrees below zero Celsius and up to 55 degrees above zero, as well as at a certain level of humidity. The temperature conditions of the human body are optimal for the reproduction, growth and vital activity of this infectious agent.
The pathogen is a representative of non-fermenting bacilli (those that do not cause fermentation processes in the body).
Methods of infection
This diplobacillus, when found on towels, napkins, cosmetics, and cosmetic instruments, can live for a day in a dried state. It is resistant to elevated (+55 degrees C) temperatures, viable in water at 10 degrees C for 5 days, which increases the risk of infection when swimming in ponds, pools, baths and saunas.
At risk are older people with weakened immune systems, people who have suffered from various infectious diseases (acute respiratory infections, acute respiratory viral infections, measles). Microtrauma of the eye, diseases of the nasopharynx, hypothermia or overheating of the conjunctiva contribute to the occurrence of diseases. Diplobacillus can be found in the nasal cavity and, when it comes into contact with the conjunctiva (for example, when sneezing), cause inflammation.
The diplobacillus that causes angular conjunctivitis can cause inflammation in cases of weakened immunity or the presence of microtrauma to the eyeball.
That is, this bacterium can be found in any healthy organism, and under favorable conditions cause disease.
Development of pathology
Diplobacillus Morax-Axenfeld is transmitted from a sick person to a healthy person, usually through contact and household contact - this is:
- use of personal items - gloves, mittens, towels, handkerchiefs, cosmetic devices;
- touching the eyes with hands that have received bacilli - for example, after shaking hands with a sick person;
- performing procedures in a cosmetology salon using instruments that have not been properly processed;
- performing medical procedures under the same circumstances;
- washing the face with water contaminated with Morax-Axenfeld bacilli.
The development of pathology is facilitated by trauma to the eyeball. These do not necessarily have to be severe injuries - microdamage to the mucous membrane of the eye is enough for the bacillus to enter the conjunctival tissue through such a “gap”.
When it comes into contact with the mucous membrane of the eye, the pathogen adapts to the new conditions of a particular organism in a fairly short time - the incubation period is only 4 days. Next, the diplobacillus is activated and releases waste products onto the conjunctiva.
An inflammatory process develops, with changes in the corners of the eyes being especially pronounced. In this case, classic signs of an inflammatory lesion are observed: redness, swelling, and a slight increase in local temperature. It is also possible for pinpoint hemorrhages to occur in the mucous membrane of the eye.
If left untreated, the inflammatory process transforms into an ulcerative one, and then into a necrotic one (death), which is prone to progression. Due to the reflex narrowing of small vessels and capillaries, tissue microcirculation (blood supply) is disrupted, they do not receive oxygen and nutrients. First, small erosions form in the conjunctiva, which, due to progressive tissue hypoxia (oxygen starvation), develop into deeper ulcers - this type of inflammation is called destructive.
note
With further progression of hypoxia with angular conjunctivitis, foci of necrosis are formed, which spreads to the cornea with the development of necrotic keratitis (its inflammation with the formation of areas of necrosis).
What it is?
The development of angular conjunctivitis is provoked by the Morax-Axenfeld bacillus (Moraxella lacunata). The stick gets into the eyes through household contact. Normally, tear fluid contains antimicrobial substances that act as a protective barrier against bacteria. Therefore, with good immunity, this microorganism does not cause disease.
Angular conjunctivitis is usually a chronic process with periodic exacerbations. Therefore, it is important to maintain immunity to prevent relapses.
Symptoms of Morax-Axenfeld angular conjunctivitis
Due to the peculiarities of its life cycle, the diplobacillus provokes a cyclical course of angular conjunctivitis - in the form of alternating periods of subsidence of the clinical picture and its increase. Symptoms develop equally on both sides.
Signs of angular conjunctivitis are:
- burning sensation;
- itching;
- pain;
- pain;
- discharge;
- crusts;
- skin cracks;
- blurred vision.
As a rule, it is from the sensation of burning and itching that the clinical picture of angular conjunctivitis begins. Unpleasant sensations are localized in the area of the orbit (the depression in the skull in which the eye is located) - the patient regularly rubs this area.
Pain in the eyes appears due to inflammatory damage to the conjunctiva, which, having become thicker, literally sticks out and is irritated by the eyelid that covers it.
The characteristics of pain are as follows:
by localization - around the eye socket;- in terms of distribution - irradiation as such is not typical;
- by nature - cutting and aching;
- in terms of intensity – average severity;
- by occurrence - they do not appear immediately, but as the pathology progresses, they can intensify when blinking.
With further progression of the disease, the inflamed conjunctiva begins to produce discharge.
Their characteristics are as follows:
- by type - mucus in the form of colorless transparent or slightly cloudy foam;
- by quantity - in a small volume, sometimes in the form of traces;
- the consistency is liquid, then after 1-3 days it becomes thick and viscous;
- by localization - it accumulates mainly in the corners of the eyes.
Thickened mucus hardens and turns into elastic crusts. The accumulation of mucus and crusts in the corners of the eyes (as well as the predominant localization of burning and cutting) gave rise to the terminological designation of pathology (“angulus” is translated from Latin as “corner”).
The discharge leads to maceration of the skin (wet corrosion), and then to the appearance of cracks - first microscopic, then more pronounced.
note
With the long-term development of angular conjunctivitis, regular visual impairment is observed - but it is temporary and manifests itself in the form of a “veil”, “fog” or “film” before the eyes. In some patients, such a disorder is not observed at all, in others it can interfere with reading, work and, in general, the normal rhythm of life.
Morax-Axenfeld angular conjunctivitis rarely manifests itself as an acute process - exacerbations and remissions (subsidence of clinical symptoms) are observed quite often, the pathology becomes chronic and can be observed for many years.
Clinical picture of the disease
Let us consider the complex of manifestations of the disease and the features of its course.
- Redness of the eyes is observed, but only in the corners of the eyes, both external and internal.
- The mucopurulent discharge is usually not abundant and is also located in the corners of the eyes.
- In the morning, crusts may form that prevent you from opening your eyes.
- There may be a decrease in visual acuity that goes away after recovery.
- The inflammatory process usually first involves one eye, then the infection attaches to the second.
Diagnostics
The diagnosis of conjunctivitis in general is not difficult to make - for this, the patient’s complaints, anamnesis (history) of the disease and examination results are sufficient. More significant is the determination of the nature of the described pathology - namely, the statement of Morax-Axenfeld angular conjunctivitis. This will require additional research methods.
From the anamnesis, it is important to visit a sauna or bathhouse, use personal hygiene items that belong to other people, and have close contact with them of a different kind.
The results of the physical examination will be:
- upon examination - redness of the skin around the eye socket, cracks in the corners of the eyes, mucus discharge, accumulation of crusts that are easily separated with little mechanical force, redness of the mucous membrane of the eyes;
- upon palpation (palpation) – sensitivity or slight pain when pressing on the eyeballs and on the area of the corners of the eyes.
Changes that can be detected by examination and palpation are more pronounced in the lateral (inner) corners of the eye, less pronounced in the lateral (side) corners. Redness is detected not only from the mucous membrane covering the eyeball, but also from the one that lines the inside of the eyelid (this is the so-called palpebral conjunctiva).
Of the instrumental research methods in the diagnosis of Morax-Axenfeld angular conjunctivitis, the following are used:
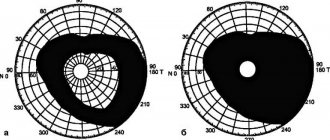
- biomicroscopy of the eye - study of fragments of the eyeball using a clinical microscope. In this case, congestion of small capillaries of the conjunctiva with blood is detected, as well as swelling of the mucous membrane of the eye. Biomicroscopy of the eye also helps to identify thickening of the cornea, its erosions, ulcers and necrotic lesions with further progression of angular conjunctivitis. Also, the redness of the conjunctiva, which covers the eyeball and lines the inside of the eyelid, is analyzed in more detail;
- Determination of visual acuity is carried out using special Sivertsev tables, “built” from lines of letters or figures. If only the conjunctiva is affected, then vision is impaired slightly; if the cornea is affected, it is significantly impaired;
- optical coherence tomography of the cornea (OCT) - using scanning, the superficial and deep layers of the cornea are studied. The method is used to determine progressive changes in the cornea that may occur when a pathological process spreads to it from the conjunctiva;
- computer keratometry – computer study of the main parameters of the cornea. It is used to assess its condition in case of secondary damage against the background of angular conjunctivitis;
- computer keratotopography – assessment of corneal curvature using a computer program. It is used in advanced cases of damage to the cornea when the pathological process spreads from the conjunctiva;
- Diaphanoscopy of the eye - study of the condition of the eyeball by transilluminating the tissues of the eye with transmitted light. It has a wide purpose, but in this case it is used to evaluate ulcerative and necrotic lesions of the cornea;
- microscopy of the cornea - its microscopic study. Allows you to identify microerosions and small necrotic foci during the progression of angular conjunctivitis.
Among the laboratory research methods used in the diagnosis of the described disease are:
general blood test - this determines nonspecific signs of inflammation in the form of an increase in the number of leukocytes (leukocytosis) and ESR;- serological tests - they are used to determine antibodies to the antigens of the Morax-Axenfeld bacillus, which can be used to indirectly judge the presence of an infectious agent;
- bacterioscopic examination - a smear-imprint of the conjunctiva is studied under a microscope, the pathogen is identified in it;
- bacteriological examination - a scraping or smear from the conjunctiva is inoculated onto special nutrient media, colonies are expected to grow, and the bacillus is identified from them. The method is also used to determine the sensitivity of the pathogen to antibiotics, which is important for subsequent treatment.
Diagnostic measures
Diagnosis of pathology begins with collecting anamnesis and examining the patient by an ophthalmologist .
Most often, a specialist uses biomicroscopy - using a slit lamp to examine the mucous membrane, cornea, iris, lens and anterior chamber of the organ of vision.
This optical device provides a large amount of information about the degree of damage to the structures of the eye, and with its help various pathologies are diagnosed.
It is worth noting! To clarify the nature of conjunctivitis, additional techniques are used:
- Bacterial culture of discharge from a diseased eye . This is necessary in order to determine the type of pathogen and select the optimal treatment regimen with antibacterial drugs.
- Cytology of scrapings from the conjunctiva.
Since the results of bacterial culture will be known only in a week, the doctor , based on the patient’s complaints, prescribes broad-spectrum antibiotics .
This is done in order not to waste time and to alleviate the patient’s condition as soon as possible.
If the test results show that the pathogen is resistant to the prescribed treatment, the therapy will be adjusted.
Complications
Angular conjunctivitis is most often complicated by the following diseases and pathological conditions:
- keratitis - damage to the cornea of inflammatory, and then ulcerative and necrotic nature;
- blepharitis – inflammation of the skin of the eyelids;
- dacryocystitis - an inflammatory process in the walls of the lacrimal sac;
- scarring of the eyelids is a connective tissue degeneration that can lead to their fusion;
- sinusitis - inflammatory damage to the mucous membrane lining the inside of the maxillary sinuses;
- frontal sinusitis is an inflammatory process that develops in the mucous membrane of the frontal sinus;
- ethmoiditis - inflammation of the mucous membrane lining the cells of the ethmoid bone;
- endocarditis is an inflammatory lesion of the inner lining of the heart, which in this case develops due to the migration of the pathogen with the bloodstream into the heart cavity;
- disruption of the structure of the heart valves and valvular insufficiency, which can lead to significant hemodynamic disorders.
Treatment of Morax-Axenfeld angular conjunctivitis
Treatment of angular conjunctivitis is carried out using conservative methods - general and local.
General purposes are as follows:
- antibacterial agents - first, broad-spectrum drugs are prescribed, and upon receipt of the results of bacterioscopic and bacteriological examinations, those antibiotics to which the pathogen is sensitive are prescribed. It responds to macrolides, tetracyclines, aminoglycosides and fluoroquinolones, but before prescribing in a particular case, its resistance (insensitivity) to antibiotics should be checked;
- non-steroidal anti-inflammatory drugs (NSAIDs);
- immunostimulating drugs - in this case biologically active peptides, drugs made from extracts from the thymus gland, interferons and interleukins are used;
- general strengthening agents - in particular, vitamins. They are prescribed in the form of pharmaceutical complexes for oral use or injection;
- Desensitizing drugs – they reduce the body’s sensitivity to pathogen toxins.
The following are used as local treatments:
- regular (up to 4-6 times a day) washing the eyes with antiseptic solutions;
- eye drops with an antiseptic effect - usually zinc sulfate. The treatment is long-term - the drug is instilled after washing the eyes 4-6 times a day for at least 1 month (often up to 1.5);
- zinc ointment - it is used to treat the edges of the eyelids;
- non-steroidal drugs in the form of eye drops. Good results are observed with instillation of diclofenac sodium;
- glucocorticosteroid drugs - they are prescribed for severe pathology and/or ineffectiveness of NSAIDs. The duration of treatment is determined by the ophthalmologist.
In general, Morax-Axenfeld angular conjunctivitis is difficult to treat. Often, when seemingly good results are achieved, a repeated “outbreak” of the disease is observed. Sometimes treatment helps stop the development of this pathology, but its regression is not observed.
The treatment of angular conjunctivitis may also involve surgery - namely, scarring and fusion of the eyelids. During the operation, the bridges are separated, the scars are excised, and, if necessary, eyelid surgery is performed.
How is the disease diagnosed?
When visiting a local clinic, the patient is referred to an ophthalmologist. The doctor conducts a standard history taking, eye examination, and makes a preliminary diagnosis. To confirm it and detect Morax-Axenfeld rods, a full diagnostic examination is required:
- general blood test - helps to assess the condition of the body, identify the presence of inflammatory processes;
- taking secretions from the corners of the eyes for bacterial culture - confirms the presence of bacteria and allows us to identify their resistance to antibacterial drugs;
- cytological examination - scraping from the mucous membrane is used to assess the cellular and microbial composition.
Therapy begins before receiving the results of bacteriological culture. The ophthalmologist prescribes antibacterial agents based on clinical symptoms and examination of the patient. Subsequently, the treatment regimen is adjusted.
Prevention
Measures to prevent angular conjunctivitis are:
- use only personal items - handkerchiefs, towels, gloves, cosmetics;
- strict adherence to the rules of personal hygiene - washing hands when in contact with objects and people outside the home;
- avoiding touching eyes with unwashed hands;
- strengthening the immune system using various known methods;
- identification of chronic foci of infection in the body, against the background of which the Morax-Axenfeld diplobacillus becomes more active.
Prevention
Important! To avoid getting angular conjunctivitis, you need to follow generally accepted hygiene measures, lead a healthy lifestyle and strengthen the immune system in every way.
Hygiene rules:
- use only your own personal towel;
- do not touch or rub your eyes with dirty hands;
- do not swim in dirty waters;
- all cosmetic procedures must be carried out only in proven salons, where all rules of sanitation and hygiene are observed;
- Do not use other people's cosmetics.
To avoid relapse of the pathology, after treatment the body must gain strength and recover .
Therefore, at this time you need to pay more attention to maintaining immunity , and also to avoid hypothermia, limit visits to swimming pools, saunas, baths , and try to have less contact with sick people.
Consequences of Morax-Axenfeld angular conjunctivitis
The prognosis for angular conjunctivitis varies. With timely diagnosis and adequate treatment, recovery occurs. But the disease is prone to recurrence - acute symptoms disappear with treatment, angular conjunctivitis becomes chronic.
The prognosis worsens with the development of cicatricial adhesions, which lead to deformation of the eyelids.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
3, total, today
( 45 votes, average: 4.53 out of 5)
Retinal detachment: symptoms, treatment and causes of pathology
Eye pain: possible causes and treatment