We have already understood the topic of macular (central) retinal dystrophy, today we will talk about other types of retinal dystrophy, how to recognize and treat them. The expert who helps us in this matter is ophthalmologist at the SPECTRUM clinic Tatyana Timofeeva
.
Tatyana Aleksandrovna, let's define what retinal dystrophy is?
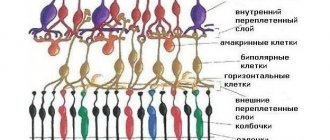
Retinal dystrophy is a deformation, a change in the cells of the retina of the eye. Dystrophy or, in other words, retinal degeneration is classified depending on the location of the lesion. Conventionally, they are divided into central
(macular) and
peripheral
zone.
Any age!
At what age do such diseases appear?
Dystrophy of various areas of the retina occurs in people of any age, regardless of visual acuity, lifestyle, or concomitant chronic diseases. For example, peripheral dystrophies occur even in people with 100% vision.
And what are the causes of degenerative changes?
The causes of retinal dystrophies are not yet fully understood. But still, factors predisposing to the occurrence of peripheral dystrophy have been identified:
high degree of myopia (from -6 and below), although there are cases of diagnosis with 100% vision; injuries; heavy physical activity (professional sports associated with intense physical activity), any sudden physical activity (sudden lifting of weights, strong fall).
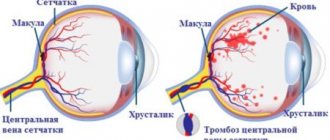
As a result of extreme activity or injury, a so-called vitreous shock occurs. The vitreous body is attached in several places (in the center and on the periphery) to the retina of the eye. During the concussion, the vitreous body moves along with the shock wave and can become detached from the retina. This can cause tears in the retina and damage it. Such injuries can even provoke such a serious condition as retinal detachment. The mechanism is that intraocular fluid leaks into the resulting gap and the retina detaches. This pathology needs to be operated on urgently, as it is a direct threat to vision.
What are the symptoms of dystrophies and retinal tears?
Detachment of the central zone of the retina is noticeable immediately. The patient feels discomfort associated with a decrease in visual acuity and sharpness.
Peripheral dystrophy, as a rule, is asymptomatic, which creates the danger of uncontrolled progression of the disease. The patient is usually not bothered by anything; extremely rarely a person may notice something like floating flies or sparkling flashes in the eye. In this case, visual acuity, as a rule, does not change. It changes for the worse when there is already a retinal detachment, when it reaches the central zone, then vision, of course, deteriorates greatly. This can happen quite abruptly. Even the patients themselves describe this condition as follows: “yesterday there were still flies floating, but today I see a swaying curtain that prevents me from seeing as before.”
Due to the asymptomatic course of various diseases, including peripheral retinal dystrophy, preventive examinations are so important once a year.
Diagnostics
What diagnostics are used to determine such conditions?
Different methods are used to diagnose central and peripheral retinal dystrophy. Optical coherence tomography of the eye determines central (macular) dystrophy, but is not informative in diagnosing peripheral changes in the retina.
To diagnose the periphery, the following studies are suitable: visometry - checking visual acuity, checking blood pressure; fundus biomicroscopy – examination of the fundus with a wide pupil.
And a little about secrets...
Have you ever suffered from HEART PAIN? Judging by the fact that you are reading this article, victory was not on your side. And of course you are still looking for a good way to get your heart functioning back to normal.
Then read what Elena Malysheva says in her program about natural methods of treating the heart and cleaning blood vessels.
Read the interview >>
Chorioretinal retinal dystrophy is a disease that causes irreversible destruction of the tissue of the vascular layers of the eyeball, during which vision significantly deteriorates. This is why it is so important to undergo annual examinations with an ophthalmologist to prevent or detect in the early stages the onset of destructive processes in the retinal tissue, which can develop with virtually no symptoms.
During the development of dystrophy, the level of central vision decreases significantly. However, the lesion does not affect the peripheral vision area, which continues to function stably. Thanks to this, even with severe forms of the disease, the patient will be able to navigate normally in a normal environment, although he will not be able to cope with activities such as driving or reading without additional devices that correct vision.
The standard examination procedure by an ophthalmologist does not allow us to examine the condition of the peripheral zone of the eyes. However, it is precisely in this area of the retina that the tissues most often succumb to degenerative processes. Since it is not possible to detect them and begin treatment immediately due to their practically asymptomatic course, the patient may face a number of additional complications, which ultimately lead to serious visual impairment, such as tissue rupture or detachment.
This disease most often occurs in older people with light pigmentation of the iris. The structure of their blood vessels is increasingly subject to age-related changes, as a result of which the retinal tissue begins to wear out intensively. In this case, the destruction process is significantly accelerated if the patient has bad habits (alcohol, smoking).
Chorioretinal retinal dystrophy
Based on type and development (pathogenesis), the following CCRDs are distinguished:
- Dry atrophic (non-exudative) is an early form of the disease in which decreased vision is accompanied by the death of the pigment epithelium. At the same time, you need to be prepared for the fact that in the next 5 years the lesion will begin to actively develop in the second eye.
- Wet (exudative). It is quite rare. It is complicated by detachments of various types of epithelium, hemorrhages in the area of affected tissues and cicatricial deformation.
As a rule, such changes can be observed even in people whose vision is normal.
Differences between wet and dry forms of pathology
Symptoms
Depending on the area in which retinal thinning develops, there are two types of disease:
- Central retinal dystrophy. Ophthalmologists deal with this form of the disease most often. The central part of the retina is affected, while peripheral vision remains normal. However, if adequate treatment for atrophy is not carried out, the patient still becomes unable to drive, read, or write.
- Peripheral retinal atrophy (PRAD). A person does not immediately detect changes in peripheral vision; it is quite difficult to detect them even with the help of special equipment. For this reason, this form of pathology remains undetected for a long time and is difficult to treat.
Depending on the location and extent of the lesions, the nature of the origin, and the clinical picture, several types of retinal dystrophy are distinguished. In addition, retinal atrophy can be congenital or acquired.
Acquired forms of pathology include macular degeneration, taperetinal retinal dystrophy and chorioretinal retinal dystrophy. They are usually accompanied by cataracts and are diagnosed in people over 60 years of age as a consequence of natural age-related changes.
With lesions of the macula, exudative or dry degeneration may develop. The latter is considered a safer form, but with the exudative form of the pathology, the patient requires special care and active medical intervention.
There are two types of pathology most often transmitted by heredity:
- pigmentary, in which the visual receptors responsible for twilight vision are affected. If the pathology is not treated, over time, peripheral vision completely disappears, the patient sees the world around him as if through a narrow tube;
- dotted white - this form of the disease is quite easy to diagnose in early childhood.
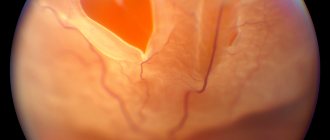
There is also Best's vitelline dystrophy, which occurs against the background of a cyst. First, a retinal cyst forms, then it ruptures, hemorrhage occurs, and then the tissue becomes scarred. With this form of pathology, the risk of retinal rupture is quite high.
But with lattice dystrophy of the eye, the retina exfoliates, but remains intact, without thinning or tears.
Thinning of the retina, as mentioned above, develops slowly, sometimes throughout life, so identifying pathology is often difficult and occurs only when a retinal tear has already occurred.
Important
Manifestations of the disease are directly related to its form. With peripheral retinal atrophy, there are often no symptoms, so the pathology is not detected at all if the patient does not get examined by an ophthalmologist for other reasons and complaints.
Blurred visual image, lack of peripheral vision, spots, lightning, foggy spots before the eyes - these signs can be used to recognize a progressive disease. Usually, a doctor is consulted already in the advanced stages of the disease, when depletion of the retina has led to its rupture. The patient's complaints in this case:
- “flies” before the eyes;
- bright flashes before the eyes;
- if the macula is affected in a form of the disease such as AMD - metamorphopsia or distortion of straight lines, central scotoma or loss of certain areas of the visual field;
- twilight blindness;
- impaired color vision;
- blurred vision.
But the main and common symptom, regardless of the type of disease, is a significant decrease in vision. Elderly people should not attribute this phenomenon to normal senile myopia; if vision deteriorates, they should definitely be examined by an ophthalmologist, especially if the patient is at risk.
Manifestations of the disease
As a rule, central chorioretinal dystrophy of the retina is classified as a multifactorial pathology that can be provoked by:
- bad heredity;
- various stages of myopia;
- disorders in the vascular system of the eyes;
- weakening of the immune system;
- intoxication with various chemicals or alcohol;
- vitamin deficiency;
- concomitant diseases, such as diabetes.
The disease can begin to develop after various eye injuries, including cataracts and surgery.
The causes of HDSH can be hereditary, and the pathology also appears with age or as a result of an unhealthy lifestyle. Pregnant women are also at risk
In the initial stages, tissue degeneration in the retina, as a rule, occurs without noticeable symptoms. The first of them appear only in the moderate or severe stages of the disease. Thus, in patients with a dry form of dystrophy, during the deterioration of vision, a veil, floaters or white flashes may periodically appear before the eyes.
The wet form of dystrophy is expressed by severe distortion or blurriness of surrounding objects, the development of color blindness (impaired color discrimination) and erroneous perception of objects in space.
If CCRD is not detected promptly and treatment is not started, tissues continue to deteriorate and vision deteriorates sharply. The disease can be detected by examining the fundus of the eye. For this purpose, a special three-mirror Goldmann lens is most often used, which allows you to see even the most extreme areas of the retina.
Additional diagnostic methods:
- conducting optical coherence and laser scanning tomography of the retina;
- implementation of computer perimetry;
- electroretinography;
- fluorescein angiography of retinal vessels.
In the early stages of diagnosing CCRD, the doctor can use a number of special tests that allow them to study how much the patient’s color rendition and contrast of vision are impaired.
Most drugs that help slow or stop the development of CCRD are taken in courses in accordance with doctor’s prescriptions:
| Antiplatelet agents | Eliminates the formation of blood clots in blood vessels. |
| Vasodilators and angioprotectors | Expand and strengthen the structure of blood vessels. |
| Lipid-lowering drugs | Reduces cholesterol. Prescribed exclusively to people with atherosclerosis. |
| Vitamins | Help stabilize vision. |
| Drugs whose action is aimed at stabilizing blood microcirculation in the retina | To achieve maximum results, they are injected directly into the eyeball. |
| Eye drops | Promotes tissue regeneration. |
Depending on the stage at which the disease was detected, drug treatment may be supplemented with physiotherapeutic procedures.
Types of pathology
Laser treatment is often used, which is a series of therapeutic techniques based on the effect of laser on the affected areas of the retina without affecting its healthy parts. The affected areas are irradiated to activate metabolic processes in them. In this case, the blood vessels are sealed, blood and fluid stop appearing under the retina, peeling it off, thereby stopping the development of the disease. The exposure procedure is painless and does not take much time.
During surgical laser intervention, the tissue in the affected area of the retina is glued (sealed) with a laser beam, which makes it possible to isolate them from healthy tissue and stop further development of the disease. It is worth noting that surgical intervention for CCRD is carried out if the disease takes a severe form, in which laser correction or special drugs do not produce results.
Causes of pathology
All operations are divided into two categories:
- revascularization - removal of damaged vessels and maximum opening of normal ones;
- vasoreconstructive - the microvascular beds of the eyes are restored using grafts.
The patient will definitely need to visit an otolaryngologist and dentist. These doctors will have to confirm the absence of chronic foci of infection and draw up appropriate conclusions, on the basis of which the ophthalmologist will give permission to perform the operation.
Retinal dystrophy before and after treatment
Classification
Central chorioretinal retinal dystrophy (CRRD, senile macular degeneration, central disciform dystrophy of the Kunt-Junius type) is a bilateral degenerative process in the retina, predominantly affecting the choriocapillary layer of the choroid or pigment epithelium, Bruch's vitreous membrane (the boundary membrane between the retina and the choroid).
It is not always possible to recognize CHRD immediately; moreover, it varies in shape. This:
- Non-exudative (dry, atrophic) dystrophy. Its occurrence may begin asymptomatically. Sometimes there may be slight curvature of straight lines. At the same time, visual acuity remains at the same level. Then the central image becomes blurry (the world is seen as if through a layer of water), and visual acuity begins to decrease, sometimes quite significantly. In some cases, this process may stabilize.
- Exudative (disciform) dystrophy. It goes through 5 stages of development:
- Detachment of the pigment epithelium. Visual acuity is maintained, but slight farsightedness or astigmatism may develop. Sometimes there may be curvature of straight lines, blurring of the image, a translucent single spot or several dark spots in front of the eyes, or light flashes.
- Neuroepithelial detachment. The above complaints + significant decrease in visual abilities. Neovascularization. It is characterized by a sharp decrease in visual acuity, up to the loss of the ability to read, write, and distinguish small details.
- Exudative-hemorrhagic detachment of neuro- and pigment epithelium. Low vision.
- Scar stage. Proliferation of fibrous tissue.
The diagnosis can only be made by a specialist. This is done on the basis of a person’s complaints, examination - checking visual acuity, campimetry, the “nine point” test or the Amsler test. Ophthalmoscopy and fluorescein angiography of the fundus are also performed.
Important
As a rule, central chorioretinal dystrophy makes itself felt after 60 years. It may develop first in one eye, then after a few years in the other. The disease has a chronic, slowly progressive course.
Severe changes in the retina seriously reduce the quality of life, as the ability to read and write, recognize faces, and do some homework is lost.
It is necessary to distinguish between dystrophy and retinal detachment - these are completely different diseases. And most often, after 60 years, it is dystrophy that develops - the replacement of the retina of the eye with fibrous tissue with the appearance of scars.
Why central retinal dystrophy (chorioretinal) occurs is not known for certain. As a rule, the culprits of its development are considered:
- Heredity.
- Violation of the vascular system of the eye.
- Weak immunity.
- Poor nutrition, bad habits.
- Moderate and high degrees of myopia.
- Old age.
- Diabetes.
- Hypertension.
- Atherosclerosis.
- Ultraviolet radiation and much more.
Treatment depends on the cause of retinal retinal dysplasia, its form and stage. It can be medicinal, laser, and sometimes surgical. The main goal of treatment is stabilization and compensation of the process, since it is impossible to completely restore vision.
For non-exudative CCRD, the following are prescribed: angioprotectors (Emoxifarm), disaggregants, antioxidants (Emoxipin) and vasodilators (Cavinton). Treatment takes place in courses (2 times a year) – in spring and autumn.
In case of exudative form, local and general treatment, laser coagulation (cauterization) of the retina is prescribed. Surgical treatment is aimed at improving blood supply to the posterior part of the eye. This is revascularization; in the non-exudative form, vasoreconstruction.
If the disease is accompanied by cataracts, then after removing the clouded lens, you can install a spheroprismatic lens, which will shift the image to a healthy area of the retina, or a bifocal lens, which will magnify the image.
When developing CCRD, it is important to seek medical help in time, since the prognosis for vision is unfavorable. Critical visual acuity for which treatment can help is 0.2 or more. But at the same time, dystrophy does not lead to complete blindness - peripheral vision remains, sufficient for orientation in space and self-care in everyday life.
A person with this disease may use a magnifying glass or special telescopic glasses that increase the size of the image on the retina. This way you can even read. Treatment must be continuous.
In this case, the patient needs to monitor blood pressure, protect his eyes from the sun, and be checked daily using an Amsler grid. These same actions should be a preventive measure for the development of CCRD for healthy people.
In addition to CCRD, there are genetic types of dystrophy - retinal pigmentary dystrophy and dotted white. At the initial stage, they are asymptomatic, especially if only one eye is affected. Sometimes “floaters” and lightning before the eyes may bother you.
In pigmentary dystrophy, the first sign is deterioration of vision in the dark (hemeralopathy). Another form of retinal dystrophy is lattice. It is most often asymptomatic. The following is possible:
- decreased visual acuity;
- deterioration of image contrast and color perception;
- undulation of straight lines.
Then dystrophy makes the visual impairment more noticeable: the ability to read, drive, and recognize faces is lost. In addition, it may become difficult or impossible to perform certain tasks, which in turn may lead to disability.
The risk group is myopic people, since the retina stretches along with the eyeball. This leads to thinning and even rupture of its affected areas.
There is a risk of retinal detachment if the vitreous body gets underneath it. But people with excellent vision can also get sick. For prevention, it is necessary to be examined by an ophthalmologist 2 times a year.
Possible complications
Even in severe form, chorioretinal retinal dystrophy does not cause blindness, therefore, even despite certain difficulties, a person will be able to determine the basic characteristics of objects and see their movement in space, if this occurs.
Particular attention to vision control should be paid to women who are in the second trimester of pregnancy. During this period, their blood pressure decreases significantly compared to normal, disrupting the stable functioning of the circulatory system.
As a result, the flow of blood and nutrients to the eye vessels in some women is disrupted, provoking the onset of degenerative processes. Moreover, the risk of their development increases significantly if a woman was treated for any eye disease before conception.
To avoid unforeseen complications, a pregnant woman should definitely be examined by an ophthalmologist. If the risk of instant dystrophy during childbirth is high, then a caesarean section will be performed to avoid fetal loss.
In addition, if a person is at risk, he must undergo an annual fundus examination by an ophthalmologist. We should also not forget about therapeutic courses aimed at stabilizing the functioning of the vascular system.
These procedures will improve peripheral blood circulation and stimulate metabolic processes in the retinal tissue, which will allow the patient to even read using special devices, such as a magnifying glass or telescopic glasses, which magnify the image transmitted to the retina.
In this case, it is imperative to exercise daily control over blood pressure levels and protect your eyes from exposure to ultraviolet rays. These same methods of protecting vision serve as the main preventive measures for healthy people.
Vascular disorder is a very general name. There are several varieties of the vessels themselves. By what signs can you understand that it’s time to run to the doctor or make a drastic lifestyle change?
The main danger to arterial vessels is atherosclerosis. The cause of its appearance is the so-called plaques that form under the thin inner lining of the arteries. Most of the “filling” of these plaques is cholesterol. How does this work? Primarily because excess cholesterol enters the body with food. At the same time, cholesterol synthesis in the liver increases. Thus, the cholesterol content in the blood increases, and its excess is deposited in the wall of the arteries. A growing atherosclerotic plaque narrows the lumen of the vessel - and this impairs blood flow. Over time, the organs supplied by this artery receive less and less oxygen and nutrients. Tangible manifestations of atherosclerosis depend on which organ is “starving”.
If it is the heart, then the person feels pain in the heart and shortness of breath during physical exertion.
If the legs - then after a short walk pain occurs like intermittent claudication.
If you have a headache, dizziness, deterioration of memory and thinking, and less often a headache will come to the fore.
How to recognize a vascular disorder? Unfortunately, a person begins to experience health problems already in the later stages of atherosclerosis, since the blood supply to organs suffers only when the lumen of the artery is blocked by plaque by more than three quarters. Unfortunately, with such a plaque size, only surgical or endoscopic intervention can help. Therefore, it is easier to prevent atherosclerosis. It is especially relevant for people whose immediate relatives had problems with the cardiovascular system.
What to do? Try to eat as much fresh vegetables, seafood, garlic and black currants as possible, use more vegetable fats than animal fats - this diet contains little cholesterol and maintains an optimal ratio of various lipids (fat) in the blood. After thirty years, periodically take a blood test for the lipid spectrum - this will help identify disorders that predispose to atherosclerosis. If there are any abnormalities, do not delay visiting your doctor - perhaps it is time to take medications that reduce the production of cholesterol in the body. If atherosclerosis is not treated, over time the plaque loses strength and breaks down, clogging the artery. This leads, depending on the location of the blockage, to such serious complications as myocardial infarction, stroke, gangrene, etc.
Another common and serious arterial disease that leads to vascular disorders is obliterating endarteritis. This inflammation of the inner lining of the artery most often affects the arteries of the legs, leading to narrowing of the vessel. The manifestations are similar to atherosclerosis, but develop faster. One of the main predisposing factors for endarteritis is constant use of nicotine. Therefore, the only prevention may be to give up any type of smoking - not just sit with a cigarette, you can’t even chew or snuff.
The most vulnerable part of the venous bed is the veins of the legs. For this injustice we have to thank upright walking. It is through these veins that blood flows from bottom to top, against gravity. To prevent blood stagnation, inside these veins there are valves - folds of the inner membrane that allow blood to pass only in the right direction. Blood flow is also facilitated by two natural ones, which performs this task only when walking and the diaphragm. A predisposition to weakness of the valve apparatus and venous wall is inherited. But that is not all. Excess weight, prolonged sitting and standing, physical inactivity, pregnancy all play a role - all this leads to the fact that the outflow of blood from the veins of the legs worsens even more.
The pressure in the veins increases and they begin to stretch, which further aggravates valve insufficiency and leads to even greater stagnation of blood. Varicose veins develop.
How to recognize a vascular disorder? The following signs will help you suspect the onset of the disease:
- after prolonged standing or sitting, a feeling of fatigue, aching and nagging pain in the legs appears;
- by the end of the day, swelling of the feet appears, which can spread to the legs;
- in the later stages of varicose veins, dilated tortuous veins are visible under the skin.
What to do? The first step is to pay attention to prevention. Especially if someone in the family has already suffered from varicose veins. The prevalence of this disease is high: every third woman and every tenth man over 40 years of age encounter it. Preventive actions include walking or leg exercises, resting while lying down, and losing weight.
Thrombophlebitis is dangerous because blood clots begin to grow on the inflamed inner lining of the venous vessel, sometimes reaching impressive sizes. The detached blood clot is carried into the blood vessels of the lungs, clogging them. This condition is called pulmonary embolism and is fatal in more than half of cases. Acute thrombophlebitis is treated only in a hospital setting. Often, with thrombophlebitis, surgery is needed to remove the blood clot or the entire inflamed vein. Unlike arteries, veins have many bypass paths. However, the matter does not end with one operation: after hospital treatment, it is usually recommended to wear compression stockings and take medications that reduce blood clots.
The reasons leading to disruption of blood flow through the capillary bed are diverse. Here are several direct mechanisms that impair microcirculation:
- various disorders of the autonomic nervous system,
- Raynaud's syndrome,
- with a lack of vitamins C and R,
- isolated microangiopathy (hereditary defects of capillary vessels),
- diabetes,
- arterial hypertension,
- autoimmune diseases.
How to recognize? A sign of impaired capillary blood flow is usually a feeling of chilliness in the toes and hands, rapid paleness of the fingers, ears and nose when going out into the cold or when washing with cold water. In areas of reduced microcirculation, trophic skin disorders are often observed: peeling, pigmentation, the formation of long-term non-healing ulcers, up to gangrene.
What to do? To dilate capillaries and improve blood flow, pentoxifylline, preparations of the ginkgo biloba plant, etc. are used. Vitamin C rutin is prescribed to reduce the fragility of blood vessels.
If you have previously performed any tests, be sure to take their results to a consultation with your doctor. If the studies have not been performed, we will do everything necessary in our clinic or with our colleagues in other clinics.
Do you have a vascular condition? It is necessary to take a very careful approach to your overall health. People do not pay enough attention to the symptoms of diseases and do not realize that these diseases can be life-threatening. There are many diseases that at first do not manifest themselves in our body, but in the end it turns out that, unfortunately, it is too late to treat them. Each disease has its own specific signs, characteristic external manifestations - the so-called symptoms of the disease . Identifying symptoms is the first step in diagnosing diseases in general. be examined by a doctor several times a year in order not only to prevent a terrible disease, but also to maintain a healthy spirit in the body and the organism as a whole.
If you want to see a doctor, use the online consultation section, perhaps you will find answers to your questions there and read tips on caring for yourself . If you are interested in reviews about clinics and doctors, try to find the information you need on the forum. Also register on the Eurolab medical to be constantly aware of the latest news and information updates on the site, which will be automatically sent to you by email.
Chorioretinal vascular disorders - what is it?
In the section Diseases, Medicines, the question is ophthalmology: chorioretinal disorders with ischemic components - what is it???What are the symptoms? asked by the author Alexey Zotov, the best answer is Choroid - choroid (The choroid itself lines the entire posterior part of the sclera from the dentate line to the point of exit through the cribriform plate of the optic nerve. Inside, the choroid is covered with pigment epithelium, which already belongs to the layers of the retina. Retina (retina) - the inner shell of the eye, which is the peripheral part of the visual analyzer; contains photoreceptor cells that provide the perception and transformation of electromagnetic radiation of the visible part of the spectrum into nerve impulses, and also provides their primary processing. Ischemia - local anemia, often caused by a vascular factor (narrowing or complete obstruction of the lumen arteries), leading to temporary dysfunction or permanent damage to tissue or organ. Depending on what causes this pathology, the forms and symptoms appear...
Treatment
Source: mgkl.ru The most informative methods for diagnosing retinal dystrophy are laser scanning of the retina using an optical tomograph, central computer perimetry, and fluorescein angiography of the blood vessels of the fundus.
They allow you to identify the earliest symptoms of retinal dystrophy. Additionally, at an early stage of diagnosing the disease, tests can also be used to check color perception, visual contrast, and the size of the central and peripheral visual fields.
In the treatment of chorioretinal retinal dystrophy, methods of photodynamic therapy, laser photocoagulation, and injections of Anti-VEGF drugs are used. The latter are a special protein that can stop degenerative processes in the macula of the eye.
Photodynamic treatment of retinal dystrophy involves intravenous administration of photosensitizer substances. They are able to bind proteins of pathological vessels and stop the development of dystrophy.
The photodynamic treatment regimen for retinal dystrophy is set individually, depending on the patient’s sensitivity to this type of therapy. Laser treatment of retinal dystrophy is based on the technique of cauterization of pathological vessels.
At the site of the burn, a scar forms on the tissues of the macula of the eye, and vision in this area of the eye is not restored. But this technique makes it possible to prevent the further spread of the process of retinal dystrophy.
In the treatment of retinal pigmentary dystrophy, mainly physiotherapeutic techniques are used: magnetic and electrical stimulation of eye tissue. Unfortunately, their effectiveness is not high. Vaso-reconstructive surgeries aimed at improving the blood supply to the retina also have a limited effect.
Prevention of retinal detachment in peripheral retinal dystrophy is carried out using laser coagulation. This minimally invasive, non-contact method for treating retinal dystrophy avoids surgical opening of the eyeball. The procedure is performed on an outpatient basis and requires virtually no recovery period.