Classification of the disease
The disease is classified depending on the extent of the lesion, its severity, and also on anatomical grounds.
Based on anatomical characteristics, they are distinguished:
- anterior scleritis;
- posterior scleritis.
Anterior scleritis is the most common type of disease, which, in turn, can be necrosing or non-necrosing. The non-necrosing form (85% of cases) is divided into diffuse or nodular; the rarer necrosing form can occur with or without inflammation.
Damage to the posterior sclera is diagnosed in only 2% of cases. Most often it is unilateral, in contrast to anterior necrotizing scleritis, in which both eyes are affected in 60% of cases.
General pathology
Histologically, the appearance of scleritis is expressed by:
- Hyperemic superficial tissue edema.
- Infiltration of tissue.
- Vascular dilations with congested blood, vascular network.
Histologically, there is a chronic and non-granulomatous infiltrate of lymphocytes and plasma cells.
With scleritis, swelling and inflammation are present in all forms of the disease. The inflammation has a granulomatous reaction zone, which can be of two types:
- localized (spot) - can lead to complete loss of vision, near the sclera in this area;
- diffuse (extensive) - the most common course of the disease, inflammation begins in one area and spreads around the circumference until the entire anterior segment is involved in the process.
According to the course of the disease, scleritis can be divided into two types:
- non-granulomatous process (lymphocytes, plasma cells, macrophages)
- granulomatous process (multinucleate giant cells) with or without associated scleral necrosis.
Clinical picture
Symptoms depend on the form, location of the disease, the nature of vascular changes, and the development of the inflammatory process.
With damage to the anterior sclera
Despite the similarity of the clinical picture with other inflammatory diseases (episcleritis), anterior scleritis symptoms are characteristic of various forms of the disease, which help differentiate it from other eye pathologies.
In the non-necrotizing diffuse form, the discomfort is more pronounced than in episcleritis, the inflammatory process affects the entire anterior sclera, and the vascular pattern is distorted. With nodular scleritis, the nodule does not move with the conjunctiva, unlike episcleritis.
The necrotizing form without inflammation is characterized by the following symptoms:
- yellow spots on the sclera that tend to enlarge and merge;
- bilateral damage to the organs of vision;
- thinning of the sclera with subsequent protrusion of the choroid;
- less commonly, the formation of staphyloma (protrusion of the posterior surface of the sclera) and its perforation with increased intraocular pressure.
Most patients with the inflammatory necrotizing form have a history of systemic diseases of the cardiovascular system. This is the most severe form of pathology, which gradually affects both eyes in more than half of the cases, and is characterized by the following symptoms in increasing order:
- redness of a limited area of the sclera;
- pain with increasing intensity that cannot be relieved with medications;
- radiating pain to the temple, eyebrows, jaw;
- injection of deep plexus scleral vessels;
- decreased conductivity of blood vessels as a result of their pathological tortuosity;
- formation of zones with insufficient blood circulation (avascular);
- tissue death (necrosis) of the sclera with expansion of the necrosis zone.
Complications are possible in the form of staphyloma, perforation of the sclera as a result of increased intraocular pressure, secondary cataracts, damage to the macula, which is dangerous due to significant deterioration or loss of vision.
Posterior scleritis
A difficult to diagnose form of inflammatory pathology, for which the characteristic symptoms are pain in the eyeball and limitation of its mobility, swelling of the eyelids, and blurred vision. Hardware examination (CT, MRI, echography) can reveal swelling of the optic nerve and retinal detachment.
Signs (symptoms)
External symptoms
External symptoms of anterior scleritis include:
- local or general redness of the section of the sclera accessible for inspection;
- increasing dull pain;
- manifestation or intensification of pain when touched through the eyelid;
- spread of pain from the eye to the jaw, temples, eyebrows;
- photophobia (in some cases);
- decreased vision (if inflammation has affected other membranes of the eye).
Posterior scleritis is not obvious. You can suspect the presence of this disease if the following signs appear:
- limitation of eyeball mobility;
- pain that increases with eye movement;
- visual impairment.
Complications
It is necessary to realize that scleritis is a disease with dangerous complications that can lead not only to deterioration or complete loss of vision, but also to death. In the absence of treatment or self-medication, the following complications may develop:
- keratitis – inflammation of the cornea, its ulceration;
- clouding of the cornea and vitreous body;
- iridocyclitis – inflammation of the iris;
- thinning of the fibrous tissue of the sclera with subsequent stretching, protrusion, perforation, scarring;
- astigmatism;
- swelling and abscess of the sclera;
- secondary glaucoma with damage to the venous circular vessel in the thickness of the sclera and the middle membrane of the eye;
- retinal detachment;
- purulent inflammation of the inner membrane (endophthalmitis) or all tissues (panophthalmitis) of the eyeball.
Pathophysiology
Pathophysiological signs are also varied. Scleritis associated with autoimmune disease is characterized by necrosis of the scleral region surrounded by granulomatous inflammation and vasculitis.
There may be a fibrinoid-eosinophilic course with the formation of a granuloma in the center of the inflammatory process.
Also, infectious scleritis is characterized by fibrinoid-exhibition necrosis with deep damage to the walls of blood vessels.
All types of this disease are characterized by an increase in inflammatory T cells, including all types and macrophages. T cells and macrophages infiltrate deep episcleral tissues with B cell clusters in perivascular areas. There may develop a cell-mediated immune response to T cells, both from HLA-DR as well as from IL-2 receptor overexpression.
Diagnosis and treatment of scleritis at NEARMEDIC
The NEARMEDIC network of multidisciplinary clinics has all the conditions to provide highly qualified services for accurate diagnosis and treatment of scleritis.
At the initial consultation, the ophthalmologist will conduct a physical and instrumental examination. If there are systemic diseases, he will prescribe consultations with related specialists.
To clarify the initial diagnosis and differentiate the disease from other inflammatory eye pathologies, and determine the etiology of the disease, diagnostics are carried out using various methods of laboratory and instrumental examinations. An ophthalmologist will issue a referral to the NEARMEDIC Diagnostic Center, where you can undergo the following tests:
- CT, MRI, ultrasound, echography;
- perimetry;
- ophthalmoscopy;
- tonometry;
- fluorescein angiography;
- visometry;
- biomicroscopy;
- virological and cytological examination of conjunctival scraping;
- immunological tests;
- blood tests;
- bacteriological examination;
- allergy tests.
Treatment is prescribed based on the results of all examinations and consultations with the development of an individual treatment plan for each individual patient.
If scleritis is diagnosed, treatment may include drug therapy, physical therapy, and surgery.
Causes of scleritis
In modern medicine, there are a large number of reasons for the occurrence of scleritis:
- rheumatism;
- various types of arthritis;
- relapsing polychondritis;
- Wegener's granulomatosis;
- general infections (streptococcus, pneumococcus, syphilis, tuberculosis);
- metabolic disorders (diabetes, gout);
- systemic inflammatory processes in the body;
- decreased immunity;
- chemical and mechanical eye injuries;
- treatment using beta-ultraviolet light and mitomycin-C;
- drug allergy.
In 50% of cases, scleritis occurs against the background of systemic diseases.
Benefits of treating eye diseases in the NEARMEDIC network
We have all the capabilities to provide effective medical care for ophthalmological diseases:
- a staff of qualified ophthalmologists and doctors of other expert specialties;
- Diagnostic center equipped with high-tech equipment;
- providing our patients with access to international medical services.
In the NEARMEDIC network you will receive a full range of medical services, which includes an initial consultation, consultation with related specialists, laboratory and hardware diagnostics, various types of therapy (drug, surgery, physical and dietary therapy, etc.), outpatient or inpatient treatment with placement in comfortable rooms and professional patient care.
NEARMEDIC's staff includes ophthalmologists with many years of practice, experience in foreign clinics, scientists and specialists of the highest and first qualification categories. If you seek help in a timely manner, they will do everything possible to save your vision.
Sign up for a consultation through the website services or by calling our Contact Center.
Objective data
Scleritis occurs with the manifestation of a characteristic violet-blue hue of the sclera. Swelling and stretching of the eyeball are also noted.
Examination in natural light differentiates the subtle color differences between scleritis and episcleritis.
Slit lamp biomicroscopy of the sclera shows inflamed vessels.
The visibility of blood vessels and wounded capillaries is also emphasized. Finally, shallow affected vessels can be palpated on the conjunctiva and superficial vessels in advanced stages.
Treatment
Drug therapy
To treat this disease, NSAIDs are prescribed - non-steroidal anti-inflammatory drugs, which are the first-line agents for mild to moderate scleritis.
Non-selective cyclooxygenase inhibitors or selective inhibitors such as flurbiprofen, indomethacin and ibuprofen may be used as adjunctive therapy.
Indomethacin can be prescribed at a dosage of 50 mg, three times a day. Ibuprofen at a dosage of 600 mg, three times a day.
The use of oral NSAIDs is not advisable, and patients are warned about gastrointestinal (GI) side effects (stomach bleeding).
Patients with impaired renal function should be warned about the toxicity of the drug.
Corticosteroids may be prescribed to relieve ocular inflammation if the patient does not respond to COX inhibitors. A typical starting dose may be 1 mg/kg/day of prednisone. An intravenous bolus of 0.5-1 mg methylprednisolone may initially be required for severe scleritis. Side effects of steroids include: decreased resistance to infection, stomach irritation, increased eye pressure, osteoporosis, weight gain, hyperglycemia and mood changes.
In addition to the main treatment, consultation with a rheumatologist is strongly recommended. Patients with rheumatoid arthritis are additionally prescribed methotrexate.
Patients with Wegener's granulomatosis may require cyclophosphamide or mofetil. Cyclosporine is nephrotoxic and, thus, can be used as an adjuvant therapy to relieve the inflammatory process with fewer side effects. Nevertheless, the risk of hematological complications is quite high, therefore, in parallel with the treatment of the underlying disease, it is necessary to take hepatoprotective drugs (Esensiale, Gepobene, etc.).
Also, all patients on therapy should take immunomodulatory drugs and closely monitor the development of systemic complications.
Surgery
Clinical examination is usually sufficient to make a diagnosis. A formal biopsy may be performed to rule out a neoplastic or infectious cause. Small corneal perforations can be repaired with contact lenses or surgical glue.
Primary indications for surgery include scleral perforation or the presence of excessive thinning of the sclera with a high risk of rupture.
Diagnostics
The doctor can determine the presence of scleritis during a visual examination, vision test and interview with the patient. Fundus examination and intraocular pressure measurement are also performed. To find out the root cause of scleritis, it is necessary to undergo tests to identify systemic diseases. The composition of tear fluid is being studied.
Hardware diagnostic methods:
- Ultrasound;
- ophthalmoscopy;
- MRI;
- biomicroscopy;
- CT scan.
Some symptoms of inflammation of the sclera are similar to other eye diseases (conjunctivitis, iritis, choroid, trauma, etc.), therefore differential diagnosis of scleritis is carried out to exclude them.
Characteristics of the disease
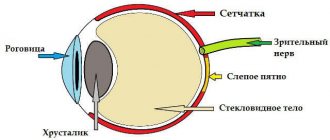
The densest layer of the eye, formed by collagen fibers, is the sclera, or the white layer of the eye. This is a kind of frame of the eyeball, consisting of three layers: outer, middle (most voluminous) and inner.
Inflammation of the sclera, affecting its layers, is called scleritis. The disease occurs more often among women than among the stronger sex. Age category. The age category most susceptible to the development of scleritis is people 40-50 years old.
The disease has several varieties, depending on the involvement of specific layers in the inflammatory process (anterior, posterior, etc.) and on localization (nodular and diffuse forms).
Prevention
- To prevent scleritis, you should take care of your immune system, strengthen it with the help of immunostimulating drugs, a balanced diet and vitamin therapy.
- If you have infectious diseases, make sure that the infection does not get into your eyes. Metabolic failures and serious disturbances in the functioning of the immune system are subject to timely treatment. Treatment of chronic illnesses and regular medical supervision are important.
- Periodic visits to the doctor and examination of the eyeball allow you to notice the presence of pathological changes in time and begin treatment.