Dilated pupils in a child are the result of various influencing factors. After all, the apple changes its size many times during the day. Its mobility is a normal condition of the human eye, and may not indicate danger. For example, the reasons are dim lighting or cloudy weather outside. In such cases, large pupils in a child become a natural reaction of the organ of perception. This helps to see objects better, that is, the eye adapts to the surrounding conditions.
However, there are conditions where this effect is present throughout the day. The reasons may be related to pathologies of internal organs, physical injuries. It is necessary to understand this issue in more detail and consider all the reasons for pupil dilation, as well as the significance of this effect for health.
What is the pupil and what are its main functions
A double pupil (pupula duplex) is an ophthalmopathology in which two or more holes are located in the iris.
This disease is extremely rare. The number of people suffering from polycoria does not exceed 40 thousand people. Most often, this condition is detected in the first year of a child’s life, but there are also cases of acquiring such a pathology. There are no differences in the distribution of double pupils based on gender or geography: this developmental defect can occur in a child of any race or gender.
Eyes without pupils are completely blind, devoid of functionality, since light and, with it, the image of the surrounding world do not enter them. The pupil is an opening in the iris of the eye of all vertebrates. This large class of creatures includes us, humans.
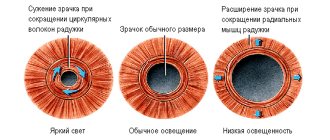
The pupils in both eyes work synchronously, letting in a dosed amount of light, this is called the friendly reaction of the pupils to light. When the light flux weakens, the pupils enlarge, that is, they dilate to let in more light.
In strong light, the pupils constrict, protecting the eye from damage from too much light. Thus, healthy pupils react to light and dilate in the dark.
An old method of diagnosing a person’s health is based on this ability: with very serious injuries, especially to the brain, the pupil does not react to light or the reaction is inadequate, for example, one pupil dilates and the other does not.
Measuring the size of the pupil in response to light in presbyopia is one of the first signs of natural aging of the body and is manifested by the inability to focus on small objects located close to a person.
There are many natural visual impairments associated with the pupil. Persistently circulating rumors about double pupils require a detailed explanation.
Classification of pathology and its causes
There are several main causes of anisocoria, which involve dozens of different diseases and conditions. In 20% of cases, anisocoria in infants is a consequence of a genetic defect. The child most often does not have any other symptoms, and the pathology of the pupil does not exceed 0.5-1 mm. In such cases, anisocoria may disappear by 5-6 years.
Types of anisocoria
- Congenital. This type of pathology is often the result of a defect in the eye or its individual elements. The reason affects the muscular apparatus of the iris and causes asynchrony in the reaction of the pupils to light. It happens that congenital anisocoria is a symptom of underdevelopment of the nervous apparatus of one eye or both, but in almost all cases the pathology is complemented by strabismus.
- Acquired. There are many reasons that can cause anisocoria throughout life.
One of the most common causes of pupillary mismatch is injury. There are several types of injuries that can cause anisocoria. First of all, these are eye injuries. Often the synchrony of pupil reactions is disrupted due to damage to the iris or ligamentous apparatus of the eye. With an eye contusion, when there are no visible injuries, paralysis of the muscular structure of the iris may develop, and the pressure inside the eye will increase.
When a head injury occurs, there is always a risk of injury to the skull or brain. Anisocoria may be the result of impaired functionality of the nervous system of the eyes or visual centers in the cerebral cortex. When the visual centers are damaged, strabismus often develops. Disturbance in the functioning of the optic nerves often leads only to one-sided dilation of the pupil. Distinctive feature: the pupil dilates in the eye on the side of the injury.
Eye diseases also often manifest themselves through anisocoria. Such ophthalmological disorders can be inflammatory or non-inflammatory in nature. Iritis and iridocyclitis (isolated inflammation of the iris) can cause spasms of the iris muscles. As a result, the eye stops responding to changes in light, which is expressed by mismatch of the pupils. Glaucoma often provokes a narrowing of the pupil in the affected eye (permanent): this makes the outflow of intraocular fluid faster and easier.
The growth of neoplasms and tumors in the head leads to a weakening of the connection between the eyeballs and the visual centers. As a result, the functionality of the iris is impaired. Such pathologies include malignant brain tumors, neurosyphilis, and hematomas in the brain after a hemorrhagic stroke.
Anisocoria can occur when exposed to certain inorganic substances: belladonna, atropine, tropicamide. When these compounds affect the nerves and muscles of the eye, pupil misalignment may occur.
Diseases of the brain and visual nerve pathways are also at risk. Among the main diseases of the central nervous system that can cause anisocoria are neurosyphilis and tick-borne encephalitis, meningitis and meningoencephalitis.
Types of anisocoria
- Caused by eye pathologies. The condition occurs due to disturbances in the elements of the eye.
- Caused by other pathologies.
According to the degree of involvement, unilateral and bilateral anisocoria are distinguished. In 99% of cases, a unilateral eye pathology is diagnosed, that is, one normal eye reacts to changes in light, and the pupil of the second either does not react or functions late.
Bilateral anisocoria is a fairly rare occurrence. The condition is characterized by an uncoordinated and inadequate response of the iris to changes in the visual regime. The degree of pathology may be different for each eye.
Eye defects
In fact, there is such an anomaly as “ polycoria”
«, when there are two pupils in the iris
, and it looks something like this:
With this disorder, there are several holes in the iris. In true polycoria, there are many pupils, each of which has a sphincter that is capable of contracting.
In most cases, pseudopolycoria
, in which only one pupil is true with a working sphincter - the muscle that contracts the pupil.
There are also other vision defects that can create the illusion of multiple pupils. For example, heterochromia
, in which the iris of the eyes is different.
Or, for example, coloboma
- a birth defect that causes a hole in the iris. People with coloboma are also blind.
Proptosis
- a condition in which the eyeball protrudes greatly.
The pupil is located in the middle of the eye, has a round shape and a complex reflex mechanism of action.
A hollow hole surrounded by muscle tissue is what the pupil is.
Pupil close up: photo
The work of this organ is aimed at dosing the flow of light from the external environment. With the help of its own micromusculature (sphincter, which constricts the pupil and dilator, which dilates it), the eye transmits the amount of light that is necessary for a clear perception of the image from the outside. Therefore, the normal diameter of the pupil, taking into account its ability to change its size, ranges from 3 to 9 mm
.
These natural reactions of the pupil to changes in lighting occur unconsciously, replacing each other thousands of times during a normal day. Insufficient lighting causes an increase in diameter
, and its excess means a decrease
.
An artificial change in the size of the pupil is used by ophthalmologists for detailed purposes; for this purpose they are used to dilate the pupils (mediatics)
. They are also used for the treatment of infectious and inflammatory diseases of the eyes, and for performing operations for the purpose of deeper penetration of drugs into the tissues of the visual organ.
Video:
Structure
The element has a variable diameter; its size changes depending on the brightness of the lighting. What is a pupil? This is a kind of diaphragm of the visual apparatus. Accordingly, the definition of “structure” is not entirely appropriate. After all, the pupil is not an anatomical element, but an ordinary hole in the center of the iris.
The iris itself is the anterior part of the choroid, located between the anterior chamber of the eye and the lens. It contains pigment cells that determine the color of the organ of vision.
| At the heart of the iris are two groups of muscle fibers that provide changes in the size of the pupil. The first is located in the shape of a concentric circle along the diameter of the hole and is responsible for its narrowing. The muscles of the second group diverge radially from the sphincter and provide pupil dilation. |
Under normal lighting conditions, the hole diameter is approximately three millimeters. However, depending on the brightness of the light flux, it varies in the range from two to eight millimeters. In infants, the hole size is about 2 mm; the level of illumination has virtually no effect on it (the diameter remains static).
Constricted pupils: reasons
Short-term or long-term dilation of the pupils is caused by natural and pathological reasons.
1. Physiological reactions of the body that occur with the expansion of this zone of the eye:
- strong excitement;
- pain;
- sexual arousal;
- intense sports activities;
- fright, anxiety, fear;
- overheating of the body;
- drinking alcohol;
- use of medications.
2. Diseases, the symptom of which is a dilated pupil:
- Pupils become smaller when people feel lethargic, are very tired, or want to rest or sleep. Constriction of the pupil for natural reasons occurs as the body ages.
- Pathological causes of constriction of the pupils lie in disruption of the nervous system (optic, trigeminal nerve), inflammation of the iris, decreased intraocular pressure, atherosclerotic changes, strokes, organic brain lesions, hypothyroidism, comatose or fainting states.
- Chronic alcoholics and smokers often have narrow pupils. The reasons for this phenomenon are hidden in the disturbance of peripheral circulation and insufficient supply of oxygen to the eye tissues, as well as their premature wear.
Functions
It is no coincidence that the pupil of the eye is located in the center; this location helps the rational distribution of solar and artificial lighting over the entire surface of the retina. This hole in the eye ensures sharpness and clarity of human perception of the world.
Its dysfunctions lead to deterioration of vision, “blurring of the picture,” and “blurring” of surrounding objects.
Thanks to the correct functioning of the pupil, people can perceive reality both during daylight hours and in the dark. This is why a person's pupils dilate at night and he can navigate quite well in low light conditions. During the day, by narrowing, the pupil reduces the intensity of sunlight, allowing you to see the surrounding space and objects in it without irritation.
Not only the muscles of the eye, but also retinal cells (cones and rods), as well as the nerve plexuses of the autonomic and parasympathetic systems, and neurons of the brain are actively involved in the work of healthy pupils. In addition, the pupil carries out the processes of accommodation
(a natural mechanism that ensures stability of vision when looking from a distant object to a near one, and vice versa). Therefore, a person easily and smoothly switches his attention to any near or distant objects.
The internal tension of the pupillary muscles (convergence reaction), which is necessary for the normal functioning of the lens and retina when fixing gaze at a close distance, is also provided by the pupil.
Pupil examination
- Pupil reaction to light
- OAZD
The pupils are examined separately in dim light. The patient should look at a distant object. If the reaction of the pupils to light is alive, then there is no need to check the reaction to accommodation, since the absence of the latter does not occur with a preserved reaction to light. Therefore, the widespread standard conclusion - “the pupils are of the correct shape, the reaction to light is lively” - does not need to be supplemented regarding the pupillary reaction at close distances.
However, if the reaction to light is weakened or absent, it is necessary to examine the reaction to accommodation and the reaction to convergence.
Purpose: to recognize the pathology of pupillary reactions and differentiate afferent and efferent damage. In an awake patient sitting quietly in room lighting, spontaneous fluctuations in pupil size are observed. This phenomenon, known as hippus , reflects spontaneous fluctuations in the tone and activity of the parasympathetic and sympathetic divisions of the autonomic nervous system. Supranuclear stimuli, such as fear or pain, activate the sympathetic nervous system and inhibit the parasympathetic nervous system, leading to pupil dilation. On the contrary, drowsiness gives rise to increasing miosis.
The absence of a reaction to light with a preserved reaction to close distances is observed when
- neurosyphilis (Argyll Robertson's symptom),
- lesions of the midbrain roof (obstructive hydrocephalus, pineal tumors),
- due to aberrant regeneration after oculomotor nerve palsy (Argyll Robertson pseudosymptom)
- with a tonic reaction of the pupil (Holmes-Adie syndrome).
If the eye's ability to perceive light is completely lost, then there is no direct reaction of the pupil to light. With partial damage to the retina or optic nerve, the direct reaction of the pupil (when the affected side is illuminated) will be less than the conjugate reaction (caused by illumination of the other eye). This relative defect in the afferent pupillary response can be detected by alternating illumination of one eye and then the other. This is a very useful sign, sometimes it is the only one that objectively indicates retrobulbar neuritis and other lesions of the optic nerve.
A small difference in pupil diameter (up to 0.5 mm) is quite common among healthy people (essential, or physiological, anisocoria). However, the relative asymmetry of the pupils should remain constant with changes in lighting.
An increase in anisocoria in twilight lighting indicates paresis of the dilator muscle as a result of damage to the sympathetic nerve.
Horner's syndrome includes unilateral miosis, ptosis, and facial anhidrosis (the latter is often absent). In most cases, it is an idiopathic disorder, but it can be caused by a brainstem stroke, carotid artery dissection, or a tumor compressing the sympathetic trunk.
An increase in anisocoria in bright light indicates damage to the parasympathetic nerves, and primarily to the parasympathetic fibers of the oculomotor nerve. The latter can be excluded if eye movements are preserved in full and idylopia ptosis is not observed.
A sharp dilation of the pupil can develop when the ciliary node located in the orbit is damaged. This is usually due to infection (shingles, influenza), ocular trauma (blunt, penetrating, surgical) or ischemia (diabetes, giant cell arteritis). After denervation of the iris, the pupillary sphincter reacts poorly to light, but the reaction to accommodation often remains relatively intact. At the same time, the dilation of the pupil when the object moves away is slowed down - this is the so-called tonic reaction of the pupil.
With Holmes-Eydie syndrome, this reaction is combined with weakened or absent tendon reflexes in the legs. It is a benign condition observed primarily in young, healthy women and is thought to indicate a mild functional disorder of autonomic regulation.
Tonic pupil reaction is also observed in Shy-Drager syndrome, segmental hypohidrosis, diabetes mellitus and amyloidosis. Sometimes it is accidentally detected in healthy people. To confirm the diagnosis, a drop of diluted (0.125%) pilocarpine is injected into each eye. The pupil of the affected eye narrows (a phenomenon of increased sensitivity of denervated structures), while the pupil of the normal eye does not respond.
Drug mydriasis can occur with accidental or intentional injection of M-anticholinergic drugs (atropine drops, scopolamine) into the eye. In such cases, pilocarpine in normal concentration (1%) does not cause pupil constriction.
Narcotic analgesics (morphine, heroin) and M-cholinergic stimulants (pilocarpine, demecarium and other drugs prescribed for glaucoma) cause constriction of the pupils, M-cholinergic blockers (scopolamine) cause dilation.
If pupils change for an unknown reason, a slit-lamp examination is necessary to rule out
- surgical trauma of the iris,
- hidden foreign body in the eye,
- penetrating eye injuries,
- intraocular inflammatory process,
- adhesions of the iris (synechia),
- angle-closure glaucoma,
- rupture of the pupillary sphincter as a result of blunt trauma to the eye.
Pupil reaction to light
Direct reaction. Instruct the patient to fix his gaze on a distant object in a dark room. Shine a bright beam of light directly into the pupil for three seconds and note the amplitude and speed of constriction of the illuminated pupil. Do this for each pupil twice or three times to calculate the average.
Friendly reaction. Sometimes it is important to examine conjugal pupillary response, the reaction of one pupil to light from another. The study of friendly reactions is not a standard test; it is not easy to determine, because the friendly pupil remains in the dark while the other eye is lightly illuminated. If one pupil consistently shows a weak or sluggish direct reaction to light, you should check its cooperative reaction (direct the light to the other pupil while observing the first). If the conjugate reaction of such a pupil is weak or sluggish, this indicates an efferent defect, either in the parasympathetic pupilloconstrictor pathways or in the iris sphincter muscle. At rest, anisocoria, more noticeable in bright light, is also present. Simply noting that the pupillary response to light is “sluggish” is not sufficient to differentiate between efferent and afferent pupillomotor defects.
- A pupil with an efferent defect does not respond correctly to any afferent stimulus—direct or ambient light, or convergence—until aberrant regeneration of damaged axons occurs.
- A pupil with damage to the afferent part of the pupillary reflex to light (relative afferent pupillary defect - RAPD) reacts weakly only to direct stimulation with light. It retains the ability to perform normal "live" contraction under the influence of other stimuli, such as friendly illumination or convergence. An afferent defect (AAD) is not the cause of anisocoria. compare the direct and cooperative reaction of this pupil to light. The reactions should be equal if the afferent functions of both eyes are intact.
OAZD
Relative afferent pupillary defect (RAPD).
Diagnosis of a relative afferent pupillary defect (RAPD or Marcus Gunn pupil) consists of examining the pupil, measuring its size and shape in diffuse light, observing the contraction of the pupil when the eye is illuminated with bright light, and then observing the return of the pupil size to its previous size when the light is removed . For all examinations, each eye is checked separately. Skill in performing a pulsed light test is required. Both pupils should contract equally to the light and maintain this contraction when the light source is smoothly but quickly moved from one eye to the other (swinging flashlight test). Dilation of one pupil when light shines on it indicates a relatively afferent pupillary defect in that eye.
A relatively afferent pupillary defect can be diagnosed in cases of iris trauma by observing the intact pupil during a pulsed light test. This maneuver is called the reverse afferent pupillary defect test and also relies on the concomitant pupillary response to light. During the test, if the intact pupil paradoxically dilates when light hits the injured eye, a relatively afferent pupillary defect in the injured eye can be diagnosed.
A relatively afferent pupillary defect is usually graded on a scale of 1 to 4, with “1” being mild and “4” being severe. Injuries to the optic nerve, such as tears, transections, traumatic contusions and large retinal detachments, usually manifest as a pronounced relatively afferent pupillary defect. Pathological processes such as sphincter and iris root tears, as well as third cranial nerve palsy, can cause anisocoria or irregular pupils, so be sure to accurately describe the size and shape of the pupil. A “pointed” pupil is often associated with anterior penetrating injuries or scleral tears complicated by entrapment of the choroid (iris).
Conditions in which there is no relative pupillary defect:
- Refractive errors (even high degrees)
- Cloudiness of the optical media (sufficiently bright light will reveal the absence of a relative pupillary defect):
- Cataract (even in the case of a completely cloudy lens)
- Corneal scars
- Hyphema (blood in the anterior chamber)
- Vitreous hemorrhage
- Previous eye surgery (in the absence of complications, previous diseases, and in the absence of new diseases)
- Strabismus
Conditions with efferent pupillary defect:
- Third cranial nerve palsy
- Eidy's pupil
- Horner's syndrome
- Moderate retinal pathology:
- Moderate underlying diabetic retinopathy
- Central serous chorioretinopathy
- Non-ischemic retinal vein occlusions
- Moderate macular degeneration
- Conditions that are usually bilateral and symmetrical will not be accompanied by a relative afferent pupillary defect:
- Bilateral retinitis pigmentosa
- Bilateral metabolic or nutritional neuroopticopathy
- Strokes are not usually accompanied by a relative afferent pupillary defect
Types of double pupil
Depending on the time of occurrence of the anomaly, polycoria can be:
- Congenital: incomplete fusion of the iris due to intrauterine exposure to damaging factors;
- Acquired: a consequence of trauma and tissue necrosis or surgery to remove an iris tumor;
In both cases, the presence of a double pupil can be observed only in one eye or in both.
There are also:
- True polycoria: all two or more pupils are controlled by a muscle and are able to react to light by changing their width;
- False polycoria: only one real pupil reacts to light, the size of the others remains unchanged;
True polycoria is usually a congenital anomaly, while false polycoria is acquired during life.
Treatment and prevention
Treatment methods for anisocoria are selected depending on the origin of the disease. If the problem lies in the field of ophthalmology, and the disease is accompanied by an oculosympathetic complex of symptoms, treatment will most likely include neurostimulation or replacement therapy with hormonal drugs.
If indications arise, the attending physician will suggest surgical correction of ptosis or dissection of the posterior synechiae. If the constriction of the pupil is caused by inflammation, the problem can be solved with anti-inflammatory and antibacterial drugs. In other words, when anisocoria is confirmed in a child, it is not the dilation or constriction of the pupil itself that needs to be treated, but the pathology that caused the problem.
Pupils of different sizes most often do not affect vision
Note! Since differences in pupil diameters are often caused by serious systemic diseases, self-medication and ignoring the problem are unacceptable. The child must be shown to a specialist, the sooner the better.
Preventive measures to prevent the development of anisocoria in an infant involve the following actions:
- Timely visit to an ophthalmologist or neurologist when the first symptoms appear.
- Monitoring your child’s indicators such as blood sugar, blood pressure and cholesterol.
It was not possible to come up with a method that would completely guarantee protection against changes in pupil size. It is quite possible to reduce the likelihood of a problem occurring.
The birth of a child is a significant event in any family. Particular attention should be paid to maintaining his health. Even a seemingly insignificant symptom such as slightly different pupils in size should make parents worry and take the baby to the doctor. The specialist will decide whether in a particular case you should worry about anisocoria or not. Parents who underestimate the dangers associated with anisocoria risk the health of their own baby. This is unacceptable under any circumstances.
Pupils of different sizes
There are cases when one pupil is larger than the other, the reasons in adults and children lie in defects in the functioning of the nervous system, traumatic injuries, vascular disorders, infections of brain tissue or tumors.
This pathology is called -. It can also be caused by taking medications, inflammation of the optic nerve, or become a long-term consequence of a concussion or bruise of the brain.
Children and adults have different pupil sizes (the difference between one and the other is 2-3 mm) - this is an alarming sign in which it is necessary to consult a specialist and begin a course of therapy. Treatment is complex, both conservative and surgical.
It happens that different pupils are a manifestation of heredity at the level of their cellular structure, which is passed on from generation to generation. This type of anisocoria does not require correction.
An eye with a tumor caused by two teeth
This Indian woman had... two teeth removed from her eye. Doctors operating on a tumor on Nagabhushanam Siva's left eye were stunned when they discovered two fully formed teeth in the woman's eye.
Doctors at a government hospital in Chennai (South India) diagnosed the woman with orbital teratoma (a rare embryonal tumor consisting of tissue growing in an attempt to form an organ). The tumor was pushing her eye outward and protruding heavily from the skin, interfering with normal vision and causing significant damage to the optic nerve.
The growth of the tumor provoked the development of a condition in which the woman could not move her eyeball, which caused the appearance of lazy eye syndrome. Doctors say that several times they encountered teratoma involving dental tissue embedded in the tumor, but they were extremely rarely able to find fully formed teeth.
Removing the tumor caused serious damage to the woman's optic nerve, who unfortunately became blind. The first case of this disease was recorded 149 years ago.
Only 70 people worldwide have since been affected by the disease.
Complications and pregnancy after varicocele
Carrying out manipulation to remove varicocele does not always solve the problem of male infertility. Its results, attempts to get pregnant, can be assessed only after 3-6 months. The possibility of pregnancy after the procedure is influenced by numerous factors and accidents:
- The quality of the intervention performed, the correct determination of indications for surgery.
- No postoperative complications.
- A man's correct attitude towards his health.
READ MORE: How long can you wear lenses? Long-term wear contact lenses, weekly and daily || How many days can you wear daily contact lenses?
If the operation is performed using a simple vein ligation method, there is a high probability of developing a relapse of the disease in the next year (from 20%). There may be no recovery of male fertility. Even a serious microsurgical intervention by a respected, competent specialist does not guarantee a 100% positive result.
The occurrence of complications after manipulation in the form of bleeding and inflammation does not improve the prognosis of subsequent pregnancy. These complications can affect the development of sclerotic changes in the testicle with a complete cessation of spermatogenesis. This possibility makes you think about refusing surgery and looking for other options to solve the problem of male infertility.
After the intervention, the patient must observe a regime of physical rest for 3-6 weeks; sexual activity is not recommended. Time is necessary for complete healing of the surgical wound and restoration of blood circulation to the testicle. Long-term abstinence worsens the state of blood circulation in the genital organs and reduces sperm count fertility rates. Subsequently, 3-6 months of active sexual activity are required to restore these indicators when pregnancy spontaneously develops. Treatment with medications to help get pregnant is less commonly added.
A man's fertility is affected by his diet.
Principles of treatment
The choice of treatment tactics is based on the severity of symptoms, the number of pupils and their sizes, and the age category of the patient. Getting rid of an ocular abnormality at its early stage will prevent the development of concomitant visual reflex disorders (spasm of accommodation, amblyopia).
Based on the diagnostic results, the ophthalmologist chooses the current method of treating polycoria:
- The iridoplasty method allows you to restore the anatomical structure of the iris with centralization of the pupil. In case of extensive damage to the iris or multiple defects, the operation is combined with implantation of an iridolens type diaphragm.
- Surgery is indicated if a pathology with a pupil diameter greater than 2 mm is detected in a newborn. The intervention is performed using tissue suturing technology; sutures are used to form a single pupillary opening.
- The choice of optics for the eyes is justified when surgery is refused or there are contraindications to its implementation. To mask the problem and correct visual acuity, the doctor selects the required option of contact lenses or glasses.
If, against the background of polycoria, the patient suffers from rapid eye fatigue, symptomatic therapy is prescribed - instillation of drugs that imitate natural tears. Radical correction of the organs of vision can only be achieved by surgical intervention, the result of which will be the restoration of the correct shape of the iris and getting rid of the double eye phenomenon.
Sources used:
- Eye and image / N.N. Blinov. - M.: Medicine, 2004.
- The world of our eyes (popular science essay on vision) / G.G. Demirchoglyan, V.I. Yankulin. - M.: Hayastan, 1978.
- Clinical atlas of fundus pathology / L.A. Katsnelson. - M.: GEOTAR-Media, 2013.
- Hofeldt, Gregory T.; Simon, John W. (2002-10-01). "Polycoria, miosis, and amblyopia". Journal of American Association for Pediatric Ophthalmology and Strabismus.
Symptoms of pathology
A double pupil, the photo of which is so popular on the Internet due to its unusual appearance, in addition to an aesthetic defect, can be accompanied by other symptoms. For example, visual discomfort associated with the inability to limit the amount of light falling on the retina.
If there are defects not only in the iris, but also in the ciliary body, there will be a violation of accommodation and, as a result, a decrease in visual acuity. Often, patients with congenital double pupils also have other anomalies of facial development (cleft lip, hard and soft palate).
Symptoms of the disease are associated with difficulty perceiving light in the affected eye. The most pronounced symptoms of the disease are with false polycoria, since in this case not all pupils are able to react by constriction to light.
The main complaints of patients with polycoria are:
- discomfort and pain when performing work that requires visual attention;
- fear of light (photophobia);
- difficulties in working at the computer, watching TV, visiting cinemas and light shows;
- the need to squint the affected eye to reduce its contribution to vision;
- difficulty in socialization due to an aesthetic defect.
The phenomenon of multiple pupils in medicine
Science classifies the fact of diagnosing two or more pupillary holes on the iris as congenital defects not associated with mystical phenomena. A characteristic feature of the pathology, called polycoria, is associated with the presence of visual discomfort, accompanied by a decrease in visual acuity. The distribution of the anomaly does not depend on gender, and the frequency of occurrence is not related to geographical features. There are no statistics on the overall prevalence of eye disease.
Features of vision with polycoria
Ophthalmic pathology is manifested by unequal sizes and shapes of the pupils, noticeably different from the standard version. This disrupts the normal functioning of the iris openings, which forms an inadequate reaction to the action of light. As a result, the patient suffers from deterioration in visual acuity and has problems recognizing colors.
Under unfavorable circumstances, polycoria is accompanied by the development of the following complications:
- amblyopia (lazy eye syndrome) is signaled by incorrect perception of shades, a characteristic tilt and turn of the head, and deviation of one eye to the side;
- Diplopia is accompanied by double vision of visible objects due to deviation of the visual axis of the organ, which leads to disruption of orientation in space and damage to the rectus muscles.
The consequences of polycoria are manifested by the development of an inability to read and work with small objects. Sometimes patients suffer from signs of photophobia - a painful reaction of the visual organs to a light source.
Interesting fact. The medical literature describes cases of exacerbation of visual ability with polycoria. If focusing improves and the ability to see far away objects appears, vision correction is not required, but medical supervision is necessary.
Classification of ocular abnormality
Polycoria is not an aesthetic defect. The pathology is recognized as a congenital defect of the ocular membrane at the embryonic stage. Impaired tissue development leads to a malfunction in the formation of the optic cup; the problem does not allow the eyeball to form correctly. The additionally formed pupils retain their reaction to light thanks to their own circular muscles (sphincters), which regulate their diameter depending on the level of illumination.
According to the clinical picture, ophthalmologists have adopted the following classification system for polycoria:
- The true form is recognized by the presence of several pupils equipped with their own sphincters. For this reason, the reaction to light remains.
- False polycoria, called pseudopolycoria, is not difficult to diagnose. The reason for zero reaction to light is the absence of a sphincter.
The true form of the disease with a completely unknown mechanism of development is rarely diagnosed. Ophthalmologists call the most likely cause of this type of disease a failure of the membrane formation process at the embryonic stage. As a result, the shape of the double pupil is similar to an hourglass.
Causes
Doctors find it difficult to identify the main causes of the pathology, but they are sure that true polycoria is associated with a gene mutation during the intrauterine formation of the fetus. Common causes of eye defect include:
- teratogenic effect on the fetus during pregnancy of the mother’s addictions (alcohol, drugs), as well as exposure to ionizing radiation;
- formation of coloboma (splitting) of the iris at the embryonic stage, which leads to partial closing of the gaps by tissue structures;
- viral infections suffered by the mother (cytomegalovirus, herpes, toxoplasma, rubella), which affected the intrauterine formation of the visual organs;
- the start of atrophic and dystrophic processes affecting the membrane of the eye, which leads to its thinning (false polycoria);
- secondary pseudopolycoria associated with the consequences of iridoplasty - mechanical damage, incorrect choice of laser power.
Other causes of pseudopolycoria include a progressive form of corectopia (displacement of the pupil from the center) or surgical intervention on the pupillary membranes. The formation of several holes on the eye shell prevents the full functioning of the sphincter, resulting in the development of accommodation and visual dysfunction.
Trauma or burns to the organs of vision also lead to the formation of several pupillary holes, similar to a false form of ocular pathology. Intracranial tumors, swelling of the muscular system of the eye, diabetes mellitus or aneurysm are considered to be the causes of the anomaly with the symbolic name pupula duplex.
For your information. Polycoria can be caused by iris hypoplasia, which develops due to the rare Axenfeld-Rieger syndrome. The essence of the pathology is that congenital underdevelopment of the iris with displacement of the pupil is accompanied by defects in the dentition and problems with the peritoneal organs.
What are the symptoms of polycoria?
Polycoria is detected during an external examination of the patient - several pupillary holes are clearly visible on the iris. Traditionally, one pupil dominates, its size is larger than the others. Additional holes often have an irregular shape, and broken symmetry causes a malfunction of the sphincter. This leads to the development of an inadequate reaction to light, depending on the form of the disease:
- a clear sign of true polycoria is the location of additional pupils separately from the main one while maintaining the reaction to light;
- pseudopolycoria is accompanied by pathological changes in the iris with corneal edema and the development of secondary type glaucoma.
The appearance of negative signals of the disease is recorded when the pupil diameter decreases to 1.5 mm or less. In this case, patients complain of deterioration in the quality of vision, which manifests itself:
- limitation of the field of view with decreased visual acuity;
- blurring of the picture, impaired accommodation;
- incorrect color perception;
- increased fatigue of the visual organs, photophobia;
- development of strong protrusion of the eyeball.
When performing work that requires visual attention, adult patients suffer from severe discomfort, and children suffer from symptoms of iris perforation, forcing them to close their eyes. According to medical practice, it has been established that signs of reduced visual acuity are observed only on the affected organ. Despite the unequal functioning of the pupils, polycoria of the eye does not signal pain, and the person is only concerned about aesthetic discrepancy with the norm.
Diagnostic methods
The congenital form of ocular pathology is diagnosed at birth; the appearance of the pupula duplex anomaly after injury requires contacting an ophthalmologist. After an external examination, the doctor evaluates the reaction to the light flux. The normal variant indicates the true type of the disease, the immobility of the pupils indicates pseudopolycoria. Performing a test with mydriatics, which dilate the pupils, also allows you to determine the type of pathology.
To clarify the extent of visual impairment, a number of additional studies will be required:
- the degree of reduced visual acuity is assessed using visometry;
- thanks to perimetry, the boundaries of the field of view are established;
- based on the results of biomicroscopy, changes in the eyeball are judged;
- Ultrasound of the eye allows you to visualize the sphincter muscles or confirm its absence.
Interesting fact. In most cases, polycoria is diagnosed in one eye. The anomaly is manifested by 2-3 additional pupillary holes in the iris. In the practice of medicine, phenomena with several pupils in both eyes have been encountered.
Other solutions to the problem
A woman can become pregnant if her husband has a varicocele without surgery if the risk of complications is high. Not every man can decide to intervene with minimal risk. You should not stop trying to get pregnant if you have a problem with varicose veins of the spermatic cord. After an examination, contacting a reproductive specialist will determine whether it is possible for a particular married couple to conceive a child, and how one can become pregnant. Several options for assisted reproductive techniques may be offered when a normal pregnancy develops:
- Insemination.
- IVF (in vitro fertilization).
- Preservation of viable sperm by freezing.
It is recommended to preserve viable sperm before surgery if there is no certainty about its outcome. This procedure can be offered to a man who plans to have children at an older age in the future. There are many other situations where sperm may be needed; the married couple themselves decide on the need to preserve reproductive material. The problem of combining varicocele and normal pregnancy in a married couple exists, and there are ways to solve it (it is possible for a woman to become pregnant).
Examination and treatment
As a rule, diagnosing a double pupil does not cause difficulties. An external examination is sufficient to identify an anomaly. Sometimes eye biomicroscopy is used to record smaller, externally invisible defects in the membrane.
Treatment for polycoria is required if it causes progressive vision loss. In the first year of a child’s life, immediately after detection of an anomaly, the defect can be eliminated surgically by suturing the iris or using collagenoplasty. In adulthood, patients use darkened lenses or mesh glasses to eliminate visual discomfort and psychological complexes.
Two pupils in one eye
A similar phenomenon is described in ancient Greek, Indian and Chinese manuscripts, with the statement that in history there were people with two irises and two pupils. However, there is not a single confirmed case in official medicine.
Science talks about another disorder - polycoria
. Outwardly, it looks like two pupils in one iris.
Two pupils: photo
The disease is real
and false:
- with the first, several pupils function, and therefore the perception of light is disrupted and vision changes;
- with the second, only one of the many pupils works, so visual functions are completely preserved and the pathology requires only cosmetic treatment.
Polycoria is based on genetic disorders. The disease has not been sufficiently studied and the search for effective methods of treating it continues.
This pathology scares people, although the vast majority of us have never encountered it in our lives and will never encounter it. The imagination pictures an eye with two full pupils. Nowadays, numerous images created with the help of photo editors have come to the aid of imagination - when you search for “pupula duplex”, the Internet returns hundreds of terrifying “photos”.
Is there a pupula duplex?
There are no comprehensive medical descriptions of patients with double or multiple full pupils in one eye. Discussions about this are based on mythology and legends.
The most famous owner of double pupils (in both eyes) was a high-ranking courtier in Ancient China. It is interesting that, in general, in the Chinese tradition, mutations and imperfections (for example, birthmarks) were considered a very bad sign, a sign of damage to the personality itself (“God marks the rogue”). But in the case of this official, the doubling of the pupils was perceived as enhanced vision, vigilance in business. Most likely, the connection here is the opposite: the imagery characteristic of the East turned a very shrewd, perspicacious minister into a “four-eyed one.” Since he lived a thousand years BC. – there is no way to establish the truth.
Modern medicine describes a similar condition with the term polycoria - “polycoria”.
Myths
The strange phenomenon of pupula duplex was first described by the ancient Roman writer Ovid. For people of the Middle Ages, the fact of double pupils caused fear; they explained the phenomenon as a magical effect. The treatises of the Roman writer and scientist Pliny the Elder provide information about women with “double eyes” who, in anger, could kill with just one look. According to the ancient Roman orator and philosopher Cicero, people with the “eye of the devil” were the cause of misfortune.
The most famous carrier of the defect is the Chinese Liu Chong. Ancient legends say that a minister who lived in the 10th century BC. e., double pupils were in both eyes. It was this appearance that the sculptor gave to the wax figure of the legendary personality, exhibited at the Tussauds Museum.
Interesting fact. The Slavs represented demons in the form of a many-eyed creature. They were often depicted as having four eyes; double eyes allow one to better see the dual essence of the world.
Description of the disease
This innate feature immediately attracted the attention of many scientists. A person has two pupils in one eyeball. One has the usual dimensions, and the second is much smaller. More often, this disease occurs only in a unilateral form. It turns out that it is almost impossible to meet a person with four symmetrical pupils.
However, there were cases when the number of pupils was more than three, while their sizes did not exceed two millimeters. This pathology significantly affects the perception of the environment. For example, the reaction to light will not only be slow, but also insignificant.
Double pupil disease is accompanied by:
- visual discomfort;
- aesthetic inconsistency;
- improved vision;
- good focusing on objects.
Symptoms indicating diplopia
The location of the images of forked objects is influenced by which eye muscles have lost their functions. In the case when the work of the oblique muscles is disrupted, the images, when looking at them, overlap each other. If the functions of the rectus muscles are impaired, then the bifurcated images appear parallel to each other. They can be located at an angle, can be shifted horizontally or vertically, and have different color effects in the form of brightness and contrast.
Symptoms of diplopia can be expressed:
- Double vision for a long time.
- It is a habit to tilt your head to the side to improve the clarity of images.
- Strabismus, which can be clearly and imperceptibly expressed. In this case, one pupil is motionless, the second is shifted towards the nose.
- Loss of orientation and feeling of dizziness.
- Impact on human performance.
Polycoria
This is a congenital defect in which there are several pupillary holes in the iris. It may be present in one or both eyes. As a rule, this disorder is combined with other defects and accompanies congenital syndromes.
True polycoria:
There are true and false polycoria:
- True polycoria - when all the pupils have sphincters and react to light, dilate when appropriate drugs are instilled;
- Pseudopolycoria - when “false” pupils do not respond to light and mydriatic medications, lacking a sphincter;
Visual acuity in such patients depends on the diameter of the pupillary openings - the smaller it is, the worse the vision.
Treatment of polycoria can be surgical. Patients are also prescribed contact lenses, which correct the appearance of the eye and correct vision.
Wikipedia about pupula duplex
The extensive virtual encyclopedia does not contain individual materials about this condition. There is a short article about polycoria here.
Modern medicine clearly distinguishes between an anomaly of a double pupil and the formation of two irises of the eye.
Treatment of anisocoria
For anisocoria that is not caused by pathology of the iris, treatment should be aimed at eliminating the underlying disease. Pupillary mismatch will disappear on its own after successful therapy.
If the cause lies in an inflammatory disease of the brain (meningitis, meningoencephalitis), broad-spectrum antimicrobial agents, detoxification therapy, and measures to correct the water-salt balance are needed.
In case of head injuries, you need to act quickly: lack of synchrony in the pupils is a bad symptom. Surgery to the skull is often required to eliminate the dangerous consequences of the injury.
If pupil misalignment is caused by injury or disease of the eye, therapy is more clear-cut. It is necessary to eliminate the pathology and correct the muscle activity of the iris. The doctor prescribes medications that directly affect the processes of dilation and constriction of the pupils. For iritis and iridocyclitis, anticholinergic drugs are needed that relax the muscles of the iris. Long-term use of such drugs can lead to permanent dilation of the pupils. Ophthalmologists also prescribe medications to eliminate inflammation.
With congenital anisocoria, the question of treatment will depend on the degree of the disorder. Most often, several operations are required to correct the eye defect. It is rare, but it happens that surgery is impossible (0.01% of all cases of congenital anisocoria). In this case, patients are prescribed eye drops for life.
Sources used:
- Morozov, V.I. Pharmacotherapy of eye diseases / V.I. Morozov, A.A. Yakovlev. - M.: Medicine, 2004.
- Rational pharmacotherapy in ophthalmology. - M.: Litterra, 2011.
- D. Hubel. Eye, brain, vision. — ed. A. L. Byzova. - M.: Mir, 1990.
- E. Fuchs Textbook of eye diseases. Volume I / E. Fuchs. — M.: State Publishing House of Medical Literature, 2021.
- Wikipedia article
Causes of diplopia of the eye
Double pupil occurs as a result of diseases that, one way or another, affect the motor function of the eye. Objects can double for a number of reasons:
- past infections such as diphtheria, rubella, mumps, tetanus;
- as a result of traumatic brain injuries;
- meningitis infection of the tuberculosis type;
- multiple sclerosis;
- neoplasms in the form of tumors in the head;
- endocrine dysfunction of the thyroid gland, diabetes mellitus;
- the walls of the carotid artery are dilated.
Also, the causes of diplopia lie in injuries to the eye orbit or a situation where the nerve is compressed and defects in the brain stem are formed.
In everyday life, extreme alcohol intoxication or excessive injection of Botox during cosmetic procedures can lead to diplopia.
If surgical operations were performed to cure the retina, strabismus or cataracts, then double image is a complication.