The lens is a transparent and flat body that is small in size, but not likely important. This round formation has an elastic structure and plays an important role in the visual system.
The lens consists of an accommodative optical mechanism, thanks to which we can see objects at different distances, regulate the incoming light and focus the image. In this article we will take a detailed look at the structure of the human eye lens, its functionality and diseases.
What does the lens of the human eye consist of?
Small size is a feature of the lens.
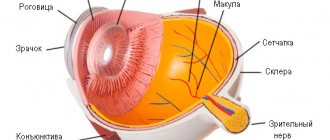
The main feature of this optical body is its small size. In an adult, the lens does not exceed 10 mm in diameter. When examining the body, it can be noted that the lens resembles a biconvex lens, which differs in radius of curvature depending on the surface. In histology, the transparent body consists of 3 parts: the ground substance, capsule and capsular epithelium.
Main substance
Consists of epithelial cells that form filamentous fibers. Cells are the only components of the lens that are converted into a hexagonal prism. The main substance does not include the circulatory system, lymphatic tissue and nerve endings.
Epithelial cells, under the influence of the chemical protein crystallin, lose their true color and become transparent. In an adult, nutrition of the lens and the main substance occurs due to moisture transmitted from the vitreous body, and in intrauterine development, saturation occurs due to the vitreous artery.
Capsular epithelium
A thin film covering the base substance. Performs trophic (nutrition), cambial (cell regeneration and renewal) and barrier (protection from other tissues) functions. Depending on the location of the capsular epithelium, cell division and development occur. As a rule, the growth zone is located closer to the periphery of the main substance.
Capsule or bag
The upper part of the lens, which consists of an elastic membrane. The capsule protects the body from harmful factors and helps refract light. Attached to the ciliary body with a belt. The capsule walls do not exceed 0.02 mm. They thicken depending on their location: the closer to the equator, the thicker.
Causes of cataracts
The lens, like any other part of the body, receives nutrients and releases waste, which occurs through the capsule. There are no capillaries or nerves in the lens itself, and lymph does not flow.
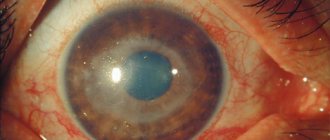
A certain composition of the liquid washes the lens. If the chemical indicator of this composition changes, the lens will not be able to receive the elements it needs and the oxidative reaction will slow down. As a result, it turns out cloudy. Doctors call this disease cataracts. Unfortunately, it is very common. It mainly appears after 50 years. It can also be congenital or acquired as a result of injury.
Atrophy
A decrease in organ volume due to lack of nutrition is called atrophy. That is, a dystrophic process. A lack of nutrients threatens the reduction of cells and tissues. Cells can slow down or even die if they don't get enough oxygen. Then they are excreted from the body, having previously broken down into molecules.
This happens, but under good conditions the cells are renewed. But with dystrophy, new cells do not appear. And in order for the organ to remain at its normal size, the remaining cells expand. The disease affects the entire eyeball or individual structures. It does not affect the size of the lens, but optical function may disappear.
This may happen due to:
- genetics
- due to injury or inflammation of the brain, eyes, skull
Ophthalmologists treat the disease with medication or surgery. The main thing is to treat the main cause, because problems in the visual organs are a consequence. Often the results of therapy are not positive and the lens is replaced with an IOL.
Functions of the lens
Pathology of the eye lens
Thanks to the unique structure of the transparent body, all visual and optical processes occur.
There are 5 functions of the lens, which together allow a person to see objects, distinguish colors and focus vision at different distances:
- Light transmission. Light rays pass through the cornea, enter the lens and easily penetrate the vitreous body and the retina. The sensitive membrane of the eye (retina) already performs its functions of perceiving color and light signals, processes them and sends impulses to the brain using nervous stimulation. Without light transmission, humanity would be completely blind.
- Light refraction. The lens is a lens of biological origin. Light refraction occurs due to the hexagonal prism of the lens. Depending on the state of accommodation, the refractive index changes (from 15 to 19 diopters).
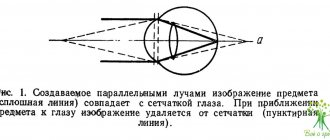
- Accommodation. This mechanism allows you to focus your vision at any distance (near and far). When the accommodative mechanism fails, vision deteriorates. Pathological processes such as farsightedness and myopia develop.
- Protection. Due to its structure and location, the lens protects the vitreous body from bacteria and microorganisms. The protective function is triggered through various inflammatory processes.
- Separation. The lens is located strictly in the center in the anterior part of the vitreous body. The thin lens is located behind the pupil, iris and cornea. Due to its location, the lens divides the eye into two parts: the posterior and anterior sections.
Due to this, the vitreous body is retained in the posterior chamber and is not able to move forward.
Types of intraocular lenses
The following types of artificial lenses are distinguished:
- “Rigid” - have an inflexible, permanent shape. Their implantation requires large surgical incisions, followed by suturing the patient and a long rehabilitation period.
- “Soft” - made of elastic synthetic polymers. They are implanted through a self-sealing micro-incision approximately 2.5 mm long. They can be placed inside the eye when folded, they unfold themselves and are securely fixed. Soft lenses do not require sutures.
There are also six main types of lenses for cataracts:
- monoblock;
- with yellow filter;
- aspherical;
- toric;
- multifocal;
- accommodating.
The aspherical shape of the lenses means that when light hits any point, the refractive power will be the same: both in the center and at the edges of the lens. This is important in the dark, when the pupil dilates.
Among the advantages of such soft lenses is minimal “glare” from light sources in the dark and twilight. So, they are comfortable when driving a car when there is light from oncoming cars. In addition, such lenses have good color rendering and contrast.
Spherical artificial lenses for the eyes refract light with different strengths, which creates a light scattering effect, contributes to the appearance of glare and flare, as a result of which the quality of vision deteriorates.
The next type of lens is toric. If during his life the patient suffered from astigmatism (an irregular shape of the cornea that distorts the image), he wore special glasses with cylinders. Modern artificial eye lenses have learned to cope with this problem. If a person with astigmatism is given a regular lens, the astigmatism will remain the same and he will have to resort to cylindrical glasses again. It is better to install toric IOLs: the necessary cylinder is already built into them, so the person will receive normal vision, without image distortion.
It is worth noting that this type of artificial lens for cataracts is selected for each patient individually; before the operation, complex calculations are made to determine which lens is best to install for cataracts. This is due to their higher cost, however, according to reviews, toric lenses give better results.
Multifocal lenses for the eyes have several optical foci, due to which they can provide maximum visual acuity both near and at long distances. Thanks to this, patients can forget about glasses. When installing a standard (monofocal) lens, the patient must use glasses for visual activity at close range.
Diseases and pathologies of the eye lens
Lens disease: aphactia
All pathological processes and diseases of the biconvex body appear against the background of the proliferation of epithelial cells and their accumulation. Because of this, the capsule and fibers lose elasticity, chemical properties change, cell clouding occurs, accommodative properties are lost, and presbyopia develops (eye abnormality, refraction).
What diseases, pathologies and anomalies can the lens encounter?
- Cataract. A disease in which clouding of the lens occurs (either complete or partial). Cataracts occur when the chemical composition of the lens changes, causing the epithelial cells of the lens to become cloudy rather than clear. When the disease occurs, the functionality of the lens decreases and the lens stops transmitting light. Cataracts are a progressive disease. In the first stages, the clarity and contrast of objects is lost, in the later stages there is a complete loss of vision.
- Ectopia. Displacement of the lens from its axis. It occurs against the background of eye injuries and with enlargement of the eyeball, as well as with overripe cataracts.
- Deformation of the lens shape. There are 2 types of deformation - lenticonus and lentiglobus. In the first case, the change occurs in the anterior or posterior part, the shape of the lens takes on the shape of a cone. With lentiglobus, the deformation occurs along its axis, in the equator region. As a rule, deformation causes a decrease in visual acuity. Myopia or farsightedness appears.
- Lens sclerosis, or phacosclerosis. Compaction of the capsule walls. Appears in people aged 60 years and above against the background of glaucoma, cataracts, myopia, corneal ulcers and diabetes.
Schlemm's canal
A gap inside the sclera, characterized as circular. Named after the German doctor Friedrich Schlemm. The anterior chamber, in the part of its angle where the junction of the iris and cornea forms, is a more precise area of the location of Schlemm's canal. Its purpose is to drain aqueous humor and ensure its subsequent absorption by the anterior ciliary vein.
The structure of the canal is more closely related to what the lymphatic vessel looks like. Its inner part, which comes into contact with the produced moisture, is a mesh formation.
The channel's capacity to transport fluid ranges from 2 to 3 microliters per minute. Injuries and infections block the functioning of the canal, which provokes the appearance of a disease in the form of glaucoma.
Diagnosis and lens replacement
To identify pathological processes and anomalies in the biological lens of the eye, ophthalmologists resort to six research methods:
- Ultrasound diagnostics, or ultrasound, is prescribed to diagnose the structure of the eye, as well as to determine the condition of the eye muscles, retina and lens.
- Biomicroscopic examination using eye drops and a slit lamp is a non-contact diagnostic that allows you to study the structure of the anterior part of the eyeball and establish an accurate diagnosis.
- Ocular congerence tomography, or OCT. A non-invasive procedure that allows you to examine the eyeball and vitreous body using x-ray diagnostics. Conherence tomography is considered one of the most effective methods for identifying lens pathologies
- Visometric examination, or assessment of visual acuity, is used without the use of ultrasound and X-ray machines. Visual acuity is checked using a special visualization table, which the patient must read at a distance of 5 m.
- Keratotopography is a unique method that studies the light refraction of the lens and cornea.
- Pachymetry allows you to examine the thickness of the lens using a contact, laser or rotary apparatus.
The main feature of the transparent body is the ability to replace it.
Nowadays, lens implantation is performed through surgery. As a rule, the lens requires replacement if it becomes cloudy and the light refractive properties are impaired. Lens replacement is also prescribed for deteriorating vision (myopia, farsightedness), lens deformation and cataracts.
Principle of operation
The lens of the eye is the anatomical structure of the anterior segment of the eye; normally it should be perfectly transparent. The principle of operation of the lens is to focus light rays reflected from an object into the macular zone of the retina. For the image on the retina to be clear, it must be transparent. When light hits the retina, an electrical impulse is generated that travels through the optic nerve to the visual center of the brain. The brain's job is to interpret what the eyes see.
Still have questions? Contact us:
Phacoemulsification is the most advanced treatment!
— How is cataract surgery performed?
The microsurgical method for removing cataracts is called phacoemulsification. In the classic version, i.e. when this is an operation for ordinary, uncomplicated age-related cataracts, it takes an experienced specialist from 7 to 10 minutes.
The operation is performed without anesthesia and is absolutely painless. Drops are used as anesthesia; only in rare cases are any injections required. A very small puncture is made in the patient's eye, 1.8 mm. Through this puncture, a tip with a special ultrasonic needle is inserted - a phacoemulsifier. This needle simultaneously destroys the lens, i.e. turns into an emulsion and is aspirated, i.e. absorbed. When the lens is completely removed and all its remains are washed out of the eye, an artificial lens is implanted through the same small puncture. This is done using an injector (the lens is inserted in a folded state, through a thin tube, like from a syringe). In the eye, the lens unfolds and is placed in the place where it should be. Moreover, the puncture is so small that no stitches are required, it closes itself. Thus, at the end of the operation the eye remains sealed.
After the operation, a special antiseptic ointment is placed in the eye, a bandage is applied on top, and the patient can immediately go home. The bandage is applied mainly to prevent the patient from accidentally rubbing the eye and introducing dirt into it. The next day it is removed and the patient begins to drip anti-inflammatory drops, which are prescribed for a period of about two weeks, a maximum of a month.
The day after surgery
You can now walk without a bandage, go to work, and even drive if your vision is normal. However, in the first week after surgery it is still advisable to reduce visual stress. For the first three days, it is recommended to wash your eyes only with drops and not to visit the pool or open bodies of water for a week, so as not to introduce dirt into the operated eye.
— How long does an artificial lens last?
All life. The lenses of good, respected companies from American, German, and English manufacturers do not become cloudy, do not deteriorate, and do not need to be replaced with others. The operation is performed once.
— Do I need to undergo examination after surgery?
You should definitely come to see the doctor the next day after surgery, because the first day is the most important. The doctor should conduct an examination and make sure that the eye is healing normally and there is no inflammation. The next visit to the doctor should be made in 3-5 days, then after 2 weeks, and come for the final examination in a month. Then all the drops are definitely stopped, reading glasses are selected if necessary, and the person can be free until the next preventive examination in six months. Further, a visit to an ophthalmologist is recommended for a general medical examination once a year.
A little history...
— Are there other types of operations?
If you go deeper into history, cataract surgery dates back to around the 5th century BC, when healers in India used a needle to pierce the eye and recess the diseased (clouded) lens into the fundus of the eye. Due to this, the pupil opened, light entered the retina through the pupil, and the person began to see something. But, of course, no artificial lenses were implanted, and the person saw quite poorly. Well, he could only see with glasses of approximately +12, but there were no glasses then.
The risk of such operations was enormous. Due to the lack of sterile instruments and good antiseptics, patients often developed acute purulent inflammation (endophthalmitis), due to which the eye stopped seeing completely. In a number of cases, during the operation, the lens capsule was disrupted, which also led to inflammation, secondary glaucoma (i.e., increased intraocular pressure), and from this the optic nerve died, the person completely lost his vision.
By comparison, today we can say that the risk of complications after standard phacoemulsification is much less than one percent.
In some clinics, however, another type of operation is still performed. Fortunately, these technologies are becoming a thing of the past, but not so long ago, intercapsular and then extracapsular extraction were mainly used. During these operations, a very large incision of about 9 mm is made in the cornea of the eye and the lens is removed through it in one block. Using this approach, the eye, of course, does not remain sealed, requiring sutures, which leave significant astigmatism.