The main goal of any surgical intervention in aesthetic surgery is the correction of defects that distort a person’s appearance, including age-related changes. The aging process on the face is clearly reflected, primarily in the eye area. Delicate and thin skin, easily susceptible to various factors, such as mechanical damage and age-related gravitational changes, begins to lose its properties quite early and succumb to various changes. Drooping of the eyelid crease is one of the earliest signs of this process. What methods of surgical modeling of the eyelid fold are used today - read on estet-portal.com.
Why does the skin of the eyelids age so quickly?
The structural features of this area of the face influence the appearance of wrinkles in young women. There are almost no sebaceous glands in the eyelid area, the skin of the eyelids is very thin and delicate, 4 times thinner than the skin of the face or the skin of the wrist, the elastic fibers around the palpebral fissure are weakly expressed. Rapid aging of the skin of the eyelids depends on the functioning of cellular organelles, which provide the cell with energy, are responsible for hereditary information, regulate the flow of nutrients into the cell and the transmission of signals.
The skin of the eyelids does not have the ability to absorb excess moisture due to the absence of fat cells. The skin of the eyelids is susceptible to swelling, which has a negative effect - it stretches and causes sagging of the skin. A large number of facial muscles around the eyes also contributes to the formation of wrinkles - any manifestations of emotions, bright sun and other factors cause contraction of the facial muscles and the appearance of small folds of skin, which subsequently turn into wrinkles.
The human eye is surrounded by periorbital fatty tissue; it plays the role of protection during pressure on the eyeball, running, and jumping. Young muscle tissues hold the eye well on the periorbital fatty tissue; with age, the ligamentous apparatus weakens, the fatty tissue penetrates into the skin of the eyelids - a hernia of the upper and lower eyelids forms.
External signs of skin aging (wrinkles, age spots, sagging and dry skin) are always associated with processes that occur in the epidermis and dermis.
LiveInternetLiveInternet
Quote from Irzeis' message
Read in full In your quotation book or community!
Facial anatomy: area around the eyes, upper and lower eyelids
The key to a good result when performing facial gymnastics and massages is an accurate knowledge of the anatomy of the face.
The fight against aging for a woman usually begins with the skin around the eyes, since this is where the first age-related problems appear: the skin loses its freshness, swelling and fine wrinkles appear.
And no wonder: in the eye area the layer of epidermis is very thin - only half a millimeter. In addition, there are almost no sebaceous glands around the eyes, a “soft pad” of subcutaneous fat, and very little muscle to maintain its elasticity. Collagen fibers (the “reinforcement” of the skin) are arranged here in the form of a mesh, so the skin of the eyelids is easily stretchable. And due to the looseness of the subcutaneous tissue, it is also prone to swelling. In addition, she is constantly in motion: her eyes blink, squint, and “smile.” As a result, the skin around the eyes is particularly stressed. Therefore, let's start understanding the structure of the face from this area.
The eyelids and periorbital region are a single complex consisting of many anatomical structures that undergo changes during surgical manipulation
| 1 - Upper eyelid fold 2 - Upper eyelid groove 3 - Internal canthus 4 - Nasolacrimal groove 5 - Eyelid-cheek division | 6 - Lower eyelid fold 7 - Horizontal axis of the eye 8 - Lateral canthus 9 - Upper eyelid |
The skin of the eyelids is the thinnest on the body. The thickness of the eyelid skin is less than a millimeter.
Unlike other anatomical areas where fatty tissue lies under the skin, just under the skin of the eyelids lies the flat orbicularis oculi muscle, which is conventionally divided into three parts: internal, median and external. The internal part of the orbicularis oculi muscle is located above the cartilaginous plates of the upper and lower eyelids, the middle part is above the intraorbital fat, the external part is located above the bones of the orbit and is woven above into the muscles of the forehead, and below into the superficial musculofascial system of the face (SMAS). The orbicularis oculi muscle protects the eyeball, performs blinking, and functions as a “tear pump.”
| 1 - Frontalis muscle 2 - External part of the orbicularis oculi muscle 3 - Median part of the orbicularis oculi muscle 4 - Internal orbicularis oculi muscle 5 - Internal canthus 6 - Nasalis muscle, 7 - Levator labii muscle | 8 - Levator labii superioris muscle 9 - Depressor nasal septum muscle 10 - Zygomatic major muscle 11 - Zygomatic minor muscle 12 - Infraorbital nerve 13 - External canthus |
The musculoskeletal system of the eyelids performs a supporting function and is represented by thin strips of cartilage - tarsal plates, lateral canthal tendons and numerous additional ligaments. The superior tarsal plate is located on the lower edge of the upper eyelid under the orbicularis oculi muscle, and is usually 30 mm in length and 10 mm in width, it is firmly connected to the inner part of the orbicularis oculi muscle, the aponeurosis of the levator superioris palpebral muscle, Müller's muscle and the conjunctiva. The inferior tarsal plate is located on the upper edge of the lower eyelid, is usually 28 mm long and 4 mm wide, and is attached to the orbicularis muscle, capsulopalpebral fascia and conjunctiva. The lateral canthal tendons are located under the orbicularis oculi muscle and are firmly connected to it. They connect the tarsal plates to the bony edges of the orbit.
| 1 — Müller’s muscle 2 — Internal canthus 3 — Lacrimal sac 4 — Ligaments | 5 - Inferior tarsal muscle 6 - Lockwood's ligament 7 - External canthus |
Under the orbicularis muscle also lies the orbital septum - a thin but very strong membrane; one edge is woven into the periosteum of the bones surrounding the eyeball, and the other edge is woven into the skin of the eyelids. The orbital septum retains the intraorbital fat within the orbit.
| 1 - Orbital septum 2 - Internal canthus 3 - Intraorbital fat - central portion 4 - Ligaments | 5 - Intraorbital fat - external portion 6 - External canthus 7 - Lacrimal gland |
Under the orbital septum there is intraorbital fat, which acts as a shock absorber and surrounds the eyeball on all sides. Portions of the upper and lower intraorbital fat are divided into internal, central and external. Next to the upper outer portion is the lacrimal gland.
| 1 - Intraorbital fat - central portion 2 - Dividing septum 3 - Intraorbital fat - internal portion 4 - Internal canthus 5 - Intraorbital fat - internal portion | 6 - Intraorbital fat - central portion 7 - Ligaments 8 - Intraorbital fat - outer portion 9 - External canthus 10 - Intraorbital fat - outer portion 11 - Lacrimal gland |
The muscle that lifts the upper eyelid opens the eye and is located in the upper eyelid under the cushion of fat. This muscle is attached to the superior tarsal cartilage. The skin of the upper eyelid is usually attached to the levator palpebrae superioris muscle. At the site of attachment of the skin to this muscle, when the eye is open, a fold forms on the upper eyelid. This supraorbital fold varies greatly from person to person. In people from Asia, for example, it is weakly expressed or not at all; in Europeans, it is well expressed.
| 1 - Muller's muscle, 2 - Levator superioris muscle 3 - Superior rectus muscle 4 - Inferior rectus muscle 5 - Inferior oblique muscle 6 - Orbital bones 7 - Orbital margin 8 - SOOF - infraorbital fat 9 - Orbital ligament 10 - Orbital septum 11 - Intraorbital fat 12 - Capsulopalpebral fascia | 13 - Inferior pretarsal muscle 14 - Inferior tarsal plate 15 - Superior pretarsal muscle 16 - Superior tarsal plate 17 - Conjunctiva 18 - Ligaments 19 - Levator palpebrae superioris 20 - Orbital septum 21 - Intraorbital fat 22 - Eyebrow 23 - Eyebrow fat 24 - Bones of the eye socket |
Behind these structures is the eyeball itself, which is supplied and innervated through the posterior part of the orbit. The muscles that move the eye are attached at one end to the eyeball and lie on its surface, and at the other end they are attached to the bones of the orbit. The nerves that control the muscles are small branches of the facial nerve and enter the orbicularis oculi muscle on all sides from its outer edges.
The anatomical structures of the lower eyelid and midface are closely related, and changes in the anatomy of the midface affect the appearance of the lower eyelid. In addition to portions of periorbital fat, two additional layers of fatty tissue exist in the midface.
Beneath the outer part of the orbicularis oculi muscle lies the infraorbital fat (SOOF). The greatest thickness of SOOF is on the outside and sides. The SOOF is deep to the superficial musculoaponeurotic system of the face (SMAS) and envelops the zygomatic major and minor muscles. In addition to SOOF, malar fat pad is an accumulation of fat in the form of a triangle or so-called. “painting” fat is located under the skin, above the SMAS.
Aging of the midface is often accompanied by sagging of the malar fatty tissue, which results in noticeable zygomatic or so-called “painting” bags on the face.
| 1 - Orbital septum 2 - Orbital ligament 3 - SOOF - infraorbital fat 4 - Zygomatic ligament | 5 - Prezygomatic space 6 - Zygomaticus major muscle 7 - Subzygomatic space |
The main supporting structure of the midface is the orbitozygomatic ligament, which runs from the bones almost along the edge of the orbit to the skin. It contributes to the formation of the zygomatic “painting” bag and the eyelid-cheek separation visible with age.
| 1 — Fatty “hernia” 2 — Painter’s “bag” 3 — Nasolacrimal groove | |
As a rule, a good aesthetic result is obtained only when the proportions of the eye and eyelids are in accordance with the proportions of the face. Outside, the eyelids and paraorbital region are represented by many anatomical structures.
| 1a - Iris 1b - Limb (circular line separating the iris from the white sclera) 2 - White sclera 3 - Inner canthus 4 - Outer canthus 5a - Lower eyelid | 5b - Edge of the lower eyelid 6a - Upper eyelid 6b - Edge of the upper eyelid 7 - Fold of the upper eyelid 8a - Inner third of the eyebrow (head) 8b - Middle third of the eyebrow (body) 8c - Outer third of the eyebrow (tail) |
The palpebral fissure is formed by the edge of the upper and lower eyelids. If you measure the eye, it usually measures 30-31 mm horizontally and 8-10 mm vertically.
| 1 - Upper eyelid fold 2 - Upper eyelid 3 - Lateral canthus 4 - Horizontal axis of the eye 5 - Lower eyelid fold | 6 - Eyelid-cheek division 7 - Nasolacrimal groove 8 - Internal canthus 9 - Upper eyelid groove |
The outer canthus is usually located 2 mm above the inner canthus in men and 4 mm in women, forming an inclination angle of 10-15 degrees, i.e. the palpebral fissure is slightly inclined from outside to inside and from top to bottom. However, the position of the outer corner of the eye may change due to age and may be influenced by heredity, race, and gender.
The edge of the upper eyelid usually covers the iris by approximately 1.5 mm, and the lower eyelid begins just below the lower edge of the iris.
The normal position (protrusion) of the eyeball relative to the bony walls of the orbit is noted in 65% of the population, and it ranges from 15 to 17 mm. Deep-set eyes have a projection of less than 15 mm, and protruding eyes have a projection of more than 18 mm.
The size of the iris is approximately the same in all people, but the shape of the scleral triangles (the white triangles between the iris and the corners of the eye) may vary. Typically, the nasal scleral triangle is smaller than the lateral one and has a more obtuse angle. With increasing eyelid laxity and age, these triangles lose shape, especially the lateral scleral triangle.
The horizontal fold in the upper eyelid is formed by the aponeurosis of the levator palpebrae superioris muscle, which is woven into the skin, passing through the orbicularis oculi muscle. Excess skin and muscle hangs over the crease, which is a fixed line. Both upper eyelid folds and the amount of skin overhanging them vary between people of different races and are influenced by gender and age.
The fold of the upper eyelid in Europeans is approximately 7 mm above the edge of the eyelid along a line drawn through the center of the pupil in men and 10 mm above the edge of the eyelid in women. In the lower eyelids, there are similar folds that are located 2-3 mm below the edge of the eyelids. Typically, lower eyelid folds are more noticeable at a young age and less noticeable as you age. In Asians, the fold of the upper eyelid is either lower - no more than 3-4 mm above the edge of the eyelid or is absent.
Differences between the female and male eyes also appear in several other points: the inclination of the palpebral fissure (from the outside in and from top to bottom) in men is less pronounced than in women, the bone structures above the eye are more full and the eyebrow itself is usually wider, located lower and less curved.
The main features of young eyelids are a smooth contour extending from the eyebrow to the upper eyelid and from the lower eyelid to the cheek and midface. The eyelid-cheek division is located at the edge of the orbit and is usually 5-12 mm below the edge of the lower eyelid, the skin is taut and the tissues are full. From the inner canthus to the outer canthus, the horizontal axis of the eye has an upward slope.
In contrast, with age, the eyes appear hollow, with a clear boundary between the eyebrow and the upper eyelid, the lower eyelid and the cheek. In most people, the palpebral fissure becomes smaller and/or rounded with age due to the downward displacement of both the upper and lower eyelids. The eyelid-cheek division is located significantly below the edge of the orbit, 15-18 mm from the edge of the lower eyelid, and the slope from the inner canthus to the outer canthus becomes downward. Which gives the eyes a sadder look.
| 1 — Drooping of the eyebrow 2 — Drooping of the upper eyelid 3 — Sagging of the lower eyelid 4 — Fatty “hernias” 5 — Malar (zygomatic) “bag” | 6 - Zygomatic groove 7 - Zygomatic groove 8 - Lacrimal groove 9 - Nasolacrimal groove 10 - Orbital fat atrophy |
A youthful upper eyelid usually has minimal excess skin. Dermatochalasis, or excess skin, is a cardinal feature of the aging upper eyelid.
Constant contraction of the muscles surrounding the eyes, the creep of sagging forehead tissues and loss of elastic properties of the skin lead to the formation of the so-called. “crow's feet” - fan-shaped wrinkles located at the outer corner of the eye and fine wrinkles under the lower eyelid.
| 1 - Hypertrophy of the frontalis muscle 2 - Descent of the frontal fat 3 - Descent of the temporal fat 4 - Descent of the brow fat 5 - Protrusion of the orbital fat 6 - Lengthening and stretching of the muscle surrounding the eye | 7 - Hypertrophy of the proud and corrugator muscles 8 - "Bags" of the upper eyelid 9 - Wrinkles at the outer corner of the eye 10 - Drooping of the upper eyelid 11 - Drooping eyebrows 12 - Horizontal forehead wrinkles |
The youthful lower eyelid has a smooth, continuous transition zone between the eyelid and cheek without bulging orbital fat, indentation, or pigmentation. With age, progressive skeletonization of the orbit occurs (the relief of the bones around the eye becomes more visible), as the subcutaneous fat covering the orbital frame atrophies and migrates downward. This downward displacement of fat results in loss of cheek convexity. Also, pigmentation (darkening of the skin) or the so-called may appear on the lower eyelid. "circles under the eyes" with or without infraorbital depressions. Eyelid bags or hernias can be caused by orbital weakening of the orbital septum, which stretches and causes orbital fat to protrude.
♦ Increase in length (height) of the lower eyelid
The nasolacrimal groove and zygomatic groove, which appear with age, can give the eye area an unaesthetic appearance. Atrophy of intraorbital fat associated with aging can make the eyes appear sunken and skeletal. Many wrinkles around the eye may reflect loss of skin elasticity.
The main causes of age-related changes in the eyelid area are stretching and weakening of the ligaments, muscles and skin of the face under the influence of gravitational forces - attraction. The elasticity of the facial ligaments weakens, they lengthen, but remain firmly fixed to the bones and skin. Consequently, in the most mobile areas with minimal fixation of the ligaments to the skin, gravity pulls the tissue downward with the formation of protrusions. They are filled with deep fatty tissues, such as “fatty hernias” of the lower or upper eyelid. Where the ligaments hold the skin and muscles more firmly, depressions or grooves appear - relief folds.
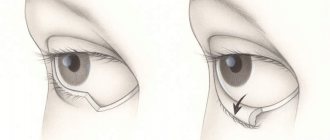
In the area of the upper eyelids, these changes may look like overhang of skin and fatty tissue in the area of the outer corners of the eye (outer “bags” - Fig. 1) and inner corners of the eye (inner “bags” - Fig. 2), overhang of only the skin over the entire eyelid gap or only from the outside (dermatochalasis - Fig. 3), drooping of the entire upper eyelid (ptosis - Fig. 4).
In the area of the lower eyelids, these changes may look like drooping of the lower eyelid (exposure of the sclera - Fig. 5), an increase in the lower portion of the muscle surrounding the eyes (hypertrophy of the orbicularis oculi - Fig. 6), the appearance of “bags” under the eyes when intraorbital fat is no longer retained inside the orbit by the orbicularis oculi muscle and the orbital septum, losing their tone (“fatty hernias” - Fig. 7, Fig. 8).
♦ Classification of age-related changes in the eyelids
Age-related changes in the lower eyelid area develop over time and can be classified into the following four types:
| Type I - Changes are limited to the lower eyelids; weakening of the muscle tone surrounding the eye and bulging of orbital fat may be observed. |
| Type II - Changes extend beyond the boundaries of the lower eyelids; weakening of the tone of the muscles surrounding the eyes, weakening of skin tone and the appearance of excess skin, slight drooping of the cheek tissue and the appearance of eyelid-cheek separation may be observed. |
| Type III - Changes affect all tissues bordering the eyelids, lowering of the tissues of the cheeks and zygomatic region, increasing the separation of the eyelid-cheek, skeletonization of the orbit - the bones of the orbit become visible, the nasolabial folds deepen. |
| Type IV - Further lowering of the eyelid-cheek separation, deepening of the nasolacrimal grooves, the appearance of the so-called. “malar” or zygomatic “bags”, drooping of the outer corners of the eye and exposure of the sclera. |
This classification helps solve problems characteristic of each type of age-related changes in the eyelid area.
| 1 - Minimal aging of the lower eyelid 2 - Minimal drooping of the eyelid-cheek separation 3 - Moderate aging of the upper eyelid with drooping of the eyebrow 4 - Eyelid-cheek separation descending below the edge of the orbit 5 - Nasolabial fold | 6 - Marked aging of the upper eyelid with drooping eyebrow 7 - Sagging edge of the lower eyelid, “rounding of the eye”, exposure of the sclera 8 - Nasolacrimal trough 9 - Painter's pouch 10 - Tear trough |
The classification demonstrates that the aging of the lower eyelid area and the midface area is inherently related to each other, and rejuvenation of one area without the other, in some cases, can lead to insufficient or unsatisfactory results. It is important to note that one of the cornerstones of these changes is the real and obvious loss of tissue volume in the eyelids and cheeks, and only its restoration can sometimes improve the situation. Source
See also:
Facelifting from Galina Dubinina: Strengthening the lower eyelid and removing bags under the eyes
How to remove wrinkles around the eyes
Swelling of the eyelids and how to deal with it
Factors that cause premature aging of the eyelid skin
There are many theories explaining the mechanisms of skin aging depending on the influence of various factors. These factors include:
- Hereditary predisposition to early skin aging.
- Difficult environmental situation.
- Stress.
- Passion for tanning.
- Poor nutrition.
- Bad habits.
- Constant lack of sleep.
There are a number of factors that accelerate skin aging due to improper use of cosmetics:
- Cleansing facial skin with soap. The skin of the eyelids does not have sebaceous glands, except for a small number of glands that are located along the growth of the eyelashes. Soap and other hygiene products dry out the skin and cause the destruction of its protective barrier.
- Poor quality cosmetics. Low-quality cosmetics often contain substances that can cause allergies, irritation, and skin damage. The skin dries out and the acid-base balance is disturbed.
- Incorrect application of cosmetics. Applying a cosmetic product against the direction of the elastic fibers leads to stretching of the skin and its sagging. When applying cosmetics, do not put pressure on the skin, pull or rub the skin of the eyelids. Cosmetics are applied in the direction of the elastic fibers, the cream is applied with light movements of the fingertips, and makeup removal should be carried out with light, blotting movements. Do not apply cosmetics to the skin of the eyelids. Due to the lack of subcutaneous fat, delicate skin becomes swollen, the eyelids become heavier, and the skin stretches. Apply cream or serum to the skin of the face without crossing the border of the edge of the orbit.
- Avoiding sunglasses in sunny weather leads to the formation of wrinkles due to constant squinting of the eyes and exposure to ultraviolet radiation on the delicate and thin skin of the eyelids. Sunscreens should not be applied to the skin around the eyes, so sunglasses become the only protection against dry skin and expression lines.
Features of the kinematics of the palpebral fold of the eyelid
Due to the dispersion of the aponeurosis fibers, which are woven into the skin, and the gradient distribution of forces on them, the fold of the eyelid responds well to the action of the levator, being pulled up and completely smoothed out when it relaxes. The palpebral fold of the eyelid reacts very actively to eye movements:
- if the gaze goes up, the fold of the eyelid deepens, lengthens, the eyelashes rise and the fold becomes clear;
- when looking down, the fold almost completely disappears and the eyelid becomes smooth;
- with an excited look, the palpebral fold is sharply expressed;
- with a dull look, the fold weakens and the eyelashes lower.
Preventive eyelid skin care
Aging cannot be stopped, but it can be delayed and you can have beautiful, soft and youthful skin for a long time thanks to proper eyelid and facial skin care and aesthetic cosmetology procedures. A correct attitude towards your own health, giving up bad habits, controlling sun exposure, a balanced diet, and physical exercise will help you look younger than your age. The correct choice of facial skin care cream plays an important role; good results are achieved by the methods of hardware cosmetology and physiotherapy:
- Light peeling (enzyme) – thanks to this procedure, the skin of the face and eyelids are quickly renewed.
- Myostimulation – helps to increase the tone of the periocular muscles. It is carried out by impulse action on the muscles.
- Lymphatic drainage acupressure (hardware lymphatic drainage) – promotes the outflow of fluid from the soft tissues around the eye, improves the condition of the skin of the eyelids, and prevents venous stagnation.
The processes taking place in the skin do not change with age, but the speed of these processes changes. Processes in young skin occur quickly; it takes 2.5 times less time to neutralize negative factors than processes in the skin of an elderly person.
Surgical modeling of the palpebral fold of the eyelid
Each stage of surgical modeling of the palpebral fold of the eyelid has its own important features:
- making a cut: it is most convenient to make a cut along the line of the intended fold;
- skin: skin resection is performed if there is an excess of it and a free flap is transplanted if there is a deficiency;
- layers of loose connective tissue: the excess layer in front and behind the orbicularis muscle makes the palpebral fold heavier, so it needs to be thinned. The lack of a loose layer is compensated with the help of fillers or orbital fiber;
- orbicularis muscle: resected in cases where there is excess thickness and area, decreased tone, or absence of high fibers of the levator aponeurosis intertwined into the skin. The resection area should be above the crease line;
- levator aponeurosis: to reduce the high fold, its upper fibers are cut, to form a high fold, the tarso-orbital fascia is cut off from the aponeurosis, and the fold is fixed at the desired height;
- fixation of the eyelid fold is the main element of surgical intervention. In the standard version, dermal-aponeurotic fixation is performed with U-shaped sutures through the mobilized orbicularis muscle. If necessary, suturing is supplemented with deep fixation and an increase in the number of sutures.
Share:
Aesthetic cosmetology methods (procedures)
There are various methods for rejuvenating the skin of the eyelids. To combat wrinkles around the eyes, they use hardware cosmetology, chemical peeling, Botox or Dysport, injection methods - mesotherapy and contouring. For older women, when other rejuvenation methods do not produce a pronounced effect, surgical lifting is recommended.
Hardware cosmetology includes several non-surgical blepharoplasties:
- Fractional photothermolysis. This type of procedure is carried out on separate areas of the skin; by heating the skin with laser energy, focal tissue destruction is achieved. Skin rejuvenation occurs after its negative stimulation (burn). Due to the impact only on small areas of the skin, the procedure is less traumatic, the recovery process occurs quickly, collagen and elastic fibers are actively formed. Fractional photothermolysis is used to smooth out wrinkles, stimulate aging skin, treat certain types of scars, correct stretch marks, and treat focal pigmentation.
- Laser resurfacing is a fractional laser resurfacing procedure that straightens wrinkles around the eyes (crow's feet), stimulates the restoration of elastic fibers, and the renewal of skin cells.
- Microdermabrasion, dermabrasion, is the resurfacing of facial skin using aluminum oxide microcrystals or diamond crystals. Crystals exfoliate facial skin cells well, polish, even out and smooth the skin. The method refers to soft and painless mechanical peelings of the face. Contraindications for the procedure are the active stage of dermatosis, rosacea, and high skin sensitivity.
Eyelid skin rejuvenation using surgery
Types of blepharoplasty:
- Laser blepharoplasty.
- Transconjunctival blepharoplasty.
- Scalpel blepharoplasty (upper, lower) and circular eyelid lift.
Laser blepharoplasty is a method with minimal trauma and rarely causes side effects (swelling, scars, infection, bruising and other complications). Scalpel blepharoplasty and circular eyelid lift are classic methods for removing excess skin, eyelid hernia and bags under the eyes. This method is used together with other methods of facial plastic surgery - contouring, neck lifting, face lifting and other procedures. Transconjunctival blepharoplasty is performed through a small incision in the eyelid area or through a puncture. Fat tissue is removed. Transconjunctival blepharoplasty does not leave noticeable scars.
Modern plastic surgery and aesthetic cosmetology have achieved high efficiency in rejuvenating facial skin; aesthetic medicine helps restore beauty and youth to patients.