Human eye tear
Tear is a colorless, salty, odorless liquid. It is characterized by a slightly alkaline reaction. Without tears, the full functioning of the organ of vision is impossible, since the eyeball must be constantly moist.
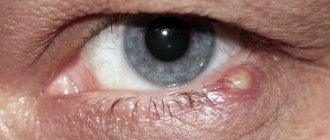
The lacrimal secretory organs are responsible for the production of important fluid, and the lacrimal secretory organs are responsible for its outflow. The complete needs of the eye are provided by the large lacrimal gland and a large number of minor, small ones. Obaglaza.ru points out that they are easily recognized visually.
Chemical composition of tears
Almost 98% of tears are H2O (water). The remaining 2% solution consists of:
- electrolytes of inorganic salts;
- mucopolysaccharides;
- proteins;
- lipids;
- a small proportion of various organic components.
The tear is responsible for keeping the front surface of the cornea clean, transparent and moist at all times. It forms a kind of precorneal film, consisting of three layers:
- surface lipid (in contact with air) – thanks to the secretion of the meibomian glands, it does not allow the next layer to evaporate;
- aqueous with mucin - the secretion of the lacrimal glands;
- mucoid - acts as a link between the second layer and the cornea.
What is a tear
The natural tear of the human eye is a salty, completely transparent liquid that continuously washes all the surface membranes of the eyeball. The special composition of tears has a slightly alkaline reaction. Tears are constantly produced by the lacrimal glands. There are several of them - one large and a number of small ones. The main functions of tears include creating conditions for the normal functioning of all structures of the human eye.
Chemical composition of tears
Natural tear fluid has a simple composition. Tears contain up to 92% water, 2% inorganic salts represented by electrolytes, lipids, a small amount of proteins, mucopolysaccharides and some other organic elements.
The structure of a tear resembles a layered film, the top layer of which is located on the cornea. The tear completely covers the anterior part of the cornea and provides it with ideal and constant transparency and the necessary smoothness. The precorneal tear film has a special composition. On top there is a lipid layer that comes into contact with the surrounding air, then there is an aqueous layer, which includes mucin. The lower layer is mucoid, it is in contact with the epithelial layer of the cornea.
The surface lipid layer contains a secretion produced by the meibomian glands. Their function is to protect the water layer from evaporation. The middle aqueous layer is formed from secretions coming from the main and also from the accessory lacrimal glands. The mucoid layer connects the corneal epithelium with the aqueous layer of tears in the human eye.
Purpose of a tear
The most important function of tears is considered to be protective. Natural tear fluid continuously moisturizes the entire conjunctiva and cornea, and this in turn greatly improves the optical properties of the eye. The special composition of tears, represented by proteins, lipid fractions and dissolved salts, allows them to perform a trophic function in relation to the cornea. Tear fluid continuously nourishes the cornea, delivering the nutrients it needs to function.
The composition of tears also includes lysozyme, an antibacterial substance that provides bactericidal properties of the tear fluid.
The protective function of tears is also manifested by the mechanical removal of small foreign substances that have entered the surface membranes of the human eye. Under the current, tears are washed away from the surface of the outer membranes of the eye, preventing inflammation from developing.
The accessory lacrimal glands normally secrete up to 1 ml of liquid per day; this volume is enough for the tears to be evenly distributed throughout the eyeball, constantly moisturizing it. The main lacrimal gland begins to function under certain circumstances. These include foreign bodies entering the eye, severe irritation of the membranes by excess light, temperature or wind, and strong emotional experiences.
Functions of tears
To maintain the surface layer of the eyeball moist, special glands produce approximately 1 ml of tear fluid per 24 hours. The release of moisture can be triggered by exposure to light radiation, the influence of heat or cold with the wind, or emotions of joy or resentment.
The tear performs several functions:
- nutrition of the cornea with fractions of lipids and proteins, salts (trophic function);
- ensuring the organ’s resistance to the effects of microorganisms due to the contained lysozyme (an antibacterial substance);
- mechanical removal of foreign bodies from the surface of the eyeball by a current of tears.
Lacrimal glands
In the conjunctival fornix there are small lacrimal glands (accessory). The main one is located under the upper eyelid in the upper-outer compartment. It is divided into two parts by the tendon of the levator palpebral muscle. The orbital (upper) lobe is located in the bony fossa on the superior outer wall of the orbit. The palpebral (lower) part is inferior to it in size and is located above the upper fornix of the conjunctiva. As a result, about 10 excretory ducts exit into it.
The lacrimal vein (outflow) and artery (inflow) are responsible for blood circulation in the gland. Parasympathetic fibers of the facial nerve regulate the secretion of tear fluid. The supply of nerve elements (innervation) is carried out:
- sympathetic fibers of the superior cervical ganglion;
- branches of the trigeminal nerve;
- parasympathetic fibers of the facial nerve.
There are three groups of accessory lacrimal glands with different secretory secretions:
- with mucous:
- granule-containing glands with goblet cells - in the conjunctiva of the eyeball and cartilage;
- Manz glands - in the limbal conjunctiva;
- crypts of Henle - in the conjunctival folds;
- with water:
- Krause's glands - in the conjunctiva of the cartilage;
- Wolfring's glands - along the edge of the cartilaginous plate and in the conjunctiva;
- Moll's glands - in the area of eyelash follicles;
- with fat:
- Zeiss glands - in the area of the roots of the eyelashes;
- meibomian glands - on the cartilaginous plate.
How a tear is structured and how it works, and what happens when the eye dries out
I have been working on biopolymers for eye treatment for about 5 years. At the end, I’ll tell you a little about what is so amazing in Russia in this direction. But let's start with the fact that tear fluid is a very interesting thing. The fact is that it smoothes the surface of the eye to obtain a smooth lens, acts as an “antivirus” at the entrance to the body through the eye, and supports several more complex reactions, in addition to immune ones.
It acts as a barrier against dust, protects the eye from scratches as a lubricant, and kills exogenous bacteria with its immune reactions. As the eyelids move, the fluid spreads across the surface of the cornea and forms a pericorneal film that lines the anterior lens of the eye. This is important because irregularities of 0.3 µm² in area are already clearly visible and distort vision. In addition, humidity is important for the non-keratinizing epithelial layer of the eye - thanks to this layer, our eyes can ultimately receive enough oxygen.
Contrary to popular belief, the lacrimal gland does very little to permanently protect the eye. This is a kind of reserve storage for fluid needed to wash the eye, or to increase the immunity of the eye (for example, as a result of emotional shock). The main tear fluid, which keeps the eye constantly moist, comes from the relatively small glands of Krause and Wolfring.
A tear
Tears are made from secretions of glands and cells from the mucous membrane of the eye; a few components also come from the vessels of the eye. The three main components of tears are lipids, mucins and water.
The yellow layer A is lipids, the blue layer B is aqueous liquid, the red layer C is the mucin layer, then comes the cornea D. Thickness is from 6 to 10 microns.
The upper lipid layer is produced by the meibomian glands (in the eyelids), the sebaceous glands of Zeiss in the hair follicles at the roots of the eyelashes, and the glands of Mohl (located nearby, these are slightly modified small sweat glands). Triple duplication of the system is necessary due to the very great importance of the eyes for the body, and, accordingly, the very great importance of this tear layer for the functioning of the eye.
This lipid film prevents tears from quickly evaporating, seals the eye when closed (so that nasty bacteria can't get inside while you sleep), reduces fluid tension and smoothes the surface of the lens, plus prevents external sweat from the skin from damaging the eye. Sometimes it happens that a patient complains of dry eyes or immediately receives an objective diagnosis of dry eye syndrome with normal or increased tear production - this is just a case of damage to lipid production for this film while the rest of the tear production glands are functioning normally. Most often, this layer is damaged as a result of blepharitis, in which the ducts of the meibomian glands in the thickness of the eyelids are blocked.
What causes dry eye syndrome?
Dry eye syndrome is essentially a disorder of tear production.
And there are several reasons for its occurrence: Systemic
- congenital, hereditary, as a result of hormonal diseases, menopause, diabetes, less often - with systemic infections. In this situation, the very properties of the eye tissues change, which leads to its dystrophy. The prevalence is 1%, and if you don’t have it in your relatives, you probably don’t need to worry. With acquired systemic dry eye syndrome, the circumstances are such that, most likely, it will worry you last in comparison with lesions of other organs.
The most common form is blepharoconjunctival.
These are diseases of the eyelids and mucous membrane of the eye. Inflammation unbalances the composition of the tear, and then the eye loses protection and everything becomes much more fun. For the doctor, not for the patient. Causes: infections, incomplete closure of the eyelids, allergies and other similar factors. Prevalence 58%.
Another 34% percent is exogenous
form (also accompanied by blepharitis). Reasons: EMP pulses (communication workers suffer), dry air, smoke, smog, cigarette smoke - the tear begins to evaporate faster. If you reduce the blinking movements of your eyes, the tears also begin to evaporate quickly. When we talk about dry eye syndrome at work or as a result of working at a computer, this is most often exactly it. Another exogenous form is caused by drugs such as hormonal contraceptives, antipsychotics, botulinum toxin injections, wearing contact lenses, ionizing radiation, and vitamin A deficiency.
The remaining cases are corneal
a form caused by an overly uneven cornea. For example, after injury, surgery (especially laser correction, keratectomy, phacoemulsification of cataracts), degenerative processes or severe toxicological lesions.
There are also combined forms, when there is no obvious “trigger”, but there are a bunch of different reasons that have accumulated as they should.
Diagnostics
The simplest method for diagnosing the correct functioning of tear fluid is the Schirmer test.
They insert special spikes on pieces of paper into your eyes and then wait until you start crying. A certain time is cut off, then it is checked how far the pieces of paper are wet. You need to gain 15 millimeters in 5 minutes. To carry it out you need these very spikes and pieces of paper; usually every ophthalmologist has them. The nuance is that patients may cry not only from eye irritation, but also from pain. Then there will be more tears. Therefore, more advanced ophthalmologists use the Jones test. Everything is the same, only first you will have pain relief.
A method available only in large diagnostic centers and laboratories is the Norn test. It shows the time it takes for the tear film to break. The tear is stained with special solutions, after which you look through the microscope without blinking until the first tear appears (visible as an unstained area). The norm is 10 seconds. The Schirmer and Jones tests measure the water component, the Norn test measures the lipid and mucin components.
There are more complex laboratory methods, but they are not as fast. If they were assigned to you, this usually already means that you are forced to deeply immerse yourself in the topic, so let’s skip it for now. If you are unlucky, you will figure out the situation.
What to do if a tear is not generated correctly?
The problem is very common. Various treatments are prescribed, which boil down to eliminating the cause of the disorders (this could be rare surgery, if there was an injury; hormonal effects, and so on), but almost always we are talking about two basic things:
- Prescribing tear replacement therapy (so that the eye does not suffer further as it loses protection as a result of the disease).
- Improvement of trophism, prevention or treatment of concomitant inflammatory processes.
Unfortunately, the second is usually forgotten, or simply not prescribed, since blepharitis may not exist at the beginning.
But with a very high probability it can arise later. But let's start with a tear. Of course, a couple of centuries ago, saline solutions worked great, then around the 80s, natural polymers became widespread - solutions based on the patient’s dry plasma or blood serum. Since not every patient was eager to become an honorary donor (even if only for themselves), the synthesis of artificial polymers was necessary. They were injected into the eye very often, which caused a lot of inconvenience to patients. Then long-acting drugs appeared:
The choice depends on the specific patient's condition. Sometimes two drugs are prescribed to work together.
Also, during treatment, hydrogel protective lenses are used, which must be worn constantly, and drugs must be administered at the same time. They are supposed to protect the eye long enough for the drugs to start working normally.
It is also possible to increase tear production due to the effect on the glands or reduce the viscosity of tears due to the effect on the mucin layer (it is limited - if there are problems with mucin, it is not applicable, plus there are rather unpleasant side effects, but sometimes the method turns out to be suitable).
Then, actually, surgery. For this purpose, they use a coating with preserved amniotic membrane (only for patients with the corneal form of the syndrome) or autoconjunctiva (according to Kunt) or perform a corneal transplant. It is better not to bring this story to light - extremely high risks and an almost astronomical cost of operations. If you do, try to go to Germany for the operation. You can also use collagen plugs for 5-7 days to prevent tears from flowing from the eyes into the nasal cavity. They gradually dissolve, but give a week for the eye to function normally.
The first part of the treatment is protective. In addition to it, etiotropic treatment is very often used, that is, helping to relieve the causes of the disease. These are restorative agents, antibiotics, desensitization, efferent therapy and reparative therapy.
Reparative therapy - restoration of the integrity of the cornea, mucous membrane, improvement of metabolism. Here are the main drugs:
You can also use autologous blood serum (a preparation from the patient’s blood).
In the blepharoconjunctival form of dry eye syndrome and in situations where blepharitis is more than possible as the disease progresses (that is, in the vast majority of cases), warm compresses, eyelid massage and hygiene products are prescribed. This is where our laboratory became one of the unique world phenomena. We developed the gels Blefarogel and Blefarogel-2 (yes, in the 90s we were more involved in science than marketing). Blepharogel is applied to the eyelids and acts as follows: it is based on hyaluronic acid, which slowly cleanses the excretory ducts of the sebaceous, meibomian, and sweat glands of the eyelids from plugs. Here, by the way, confusion arises - for some reason, ladies on cosmetology forums, seeing a familiar biopolymer, decide that it removes wrinkles. No, blepharogel is for something else. But yes, the hydrobalance of the eyelid skin is also normalized and its elasticity increases. Then aloe extract works - it is an antiseptic and helps trophism. As a result, swelling and hyperemia are relieved. And Blefarogel 2 is more serious. It additionally includes sulfur preparations that accurately kill parasites, in particular Demodex mites - a lot of blepharitis is associated with them.
As a result, with the parallel administration of massage or phonophoresis (magnetophoresis, electrophoresis), dry eye syndrome is successfully cured, since fluid exchange and gland function are normalized. The cause of the disease is being treated. In addition, both drugs can be used to prevent dry eye syndrome, as well as simply to improve trophism, especially if a person is in uncomfortable working conditions.
Historically, in the late 90s, my company worked on biopolymers for cosmetics in an institute laboratory. Doctors came to us who needed our developments - during a series of tests they used our hyaluronic acid gels for treatment, and the very first tests showed results. The medical developers showed us what we needed to achieve, and the polymer developers made the necessary tools. Before the start of our work, for example, on Blepharogel, 2 patients with demodicosis were transferred from optics to KVD and back. For 3-4 years we tested the first products and certified them as hygienic. Then another series of studies and documents for a medical device were needed. Initially, we were very lucky that from the very first experiments we worked exclusively with pure hyaluronic acid (we will talk about the importance of this and methods of synthesis a little later).
A little later I will tell you in more detail about the process of developing biopolymer products, if you are interested. In the meantime, here you can look at our production of gels for ultrasound and cosmetic preparations, which are based on the same polymer developments. Well, here are some more details about the SSG.
Lacrimal organs
There is a rather complex system for the outflow of tear fluid. First, the tear passes along the lacrimal stream between the apple and the back surface of the edge of the eyelid. Then it collects in a lake at the entrance to the lacrimal canaliculi (the upper and lower lacrimal openings on the corresponding eyelids), enters the lacrimal sac and the nasolacrimal canal. The latter has an opening inside the nasal cavity. The lacrimal tubules first run vertically for about 2 mm, then horizontally for about 8 mm. The inferior tubule drains almost 70% of the fluid.
Reverse flow (reflux) is limited by the Rosenmüller valve at the entrance of the canaliculus to the 5-10 mm long lacrimal sac, located between the anterior and posterior bony lacrimal crests. When blinking, tears are removed from the accumulated lake by a pumping mechanism due to the pressure created by the orbicularis muscle and the fascia of the sac.
The fluid moves further along the nasolacrimal duct into the lower nasal passage, partially covered by the Hasner valve. Obaglaza.ru reminds that the listed valves are mucous folds.
Diseases of the lacrimal organs
The main signs of deviations from the normal state of the lacrimal organs:
- burning in the eye;
- sensation of so-called “sand” or the presence of a foreign object on the mucous membrane;
- dryness;
- profuse lacrimation.
Such symptoms are characteristic of insufficient production of tear fluid (hypofunction) or disruption of its outflow. The cause of the lesion can be located externally (at the lacrimal openings, at the border of the lower eyelid), and deeper - in the nasolacrimal canal or in the tubules. Obaglaza.ru notes that swelling and redness of the edge of the eye from the inside may indicate inflammation of the lacrimal sac with a long delay in the outflow of fluid. This anomaly of the lacrimal gland occurs most often with certain lesions of the glandular organs.
Diagnosis of diseases of the lacrimal organs
- When palpating the inflamed lacrimal sac, pain is felt. Swelling and discoloration of the eyelids are detected by visual inspection of their condition and position.
- To examine the palpebral lobe of the lacrimal gland, eversion of the upper eyelid is used under the light of a slit lamp.
- The biomicroscopy of the eye makes it possible to diagnose the condition of the lacrimal openings, the sufficiency of hydration of the cornea and conjunctiva.
- Bengal pink dye is used for testing to identify dead (non-viable) epithelial cells that appear as a result of disturbances in the functioning of the lacrimal glands.
- The patency of the lacrimal canals is checked by washing the inflow and outflow of fluid. If there are no deviations from the norm, then water passes through the lacrimal opening into the nasal and oral cavities. A special dye, fluorescein, serves the same purpose: it should be released from the nose a few seconds after injection into the conjunctival sac.
If there is a suspicion of tract obstruction, then an X-ray examination using contrast dacryocystography is prescribed. This allows you to unambiguously determine the degree of development of the inflammatory process.
The rate of fluid reproduction is assessed by performing the Schirmer test - a test with special strips that are placed behind the lower eyelid. If they are wetted with moisture at less than 1 mm/minute, then this speed is considered insufficient and indicates a violation of the secretion of the lacrimal glands. Often, tear production is inhibited by the use of certain medications.
Compound
The main part (up to 98%) is water, the rest is inorganic substances (sodium chloride, sodium and magnesium carbonate, as well as calcium sulfate and phosphate. Tears contain proteins and carbohydrates, and in order not to linger on the surface of the skin, they [ what?
] are covered with a thick, greasy film.
This greasy film was specially studied by American scientists [ which ones?
], who discovered the lipid oleamide in it (previously it was found only in the cells of the brain and central nervous system). [
source not specified 150 days
] In addition, the tear fluid contains enzymes, the most important of which is lysozyme, which gives tears bactericidal properties . It kills bacteria by breaking down their cell walls.
Tears contain approximately 1.5% sodium chloride, some albumin and mucus.
The chemical composition of tears is similar to the composition of blood, but unlike blood, the tear fluid contains a higher concentration of potassium and chlorine, but less organic acids. Tears carry no less information than a drop of blood: their chemical composition is constantly changing depending on the state of the body.
Among the numerous proteins produced by the lacrimal glands, the highest concentrations in the tear fluid are characteristic of lactoferrin, lipocalin and lysozyme; Amylases, peroxidases[en], plasminogen activator[en], prolactin, epidermal growth factor, transforming growth factor beta (TGF-beta), endothelin-1, retinol (lactoferrin, lipocalin, peroxidases and lysozyme protect the cornea from viral and bacterial infections, retinol is important for corneal health, growth factors and endothelin-1 play an important role in the healing of the cornea when abrasions or ulcers appear on it)[1][2].
Treatment of disorders
- After identifying disturbances in the functioning of the lacrimal organ system and determining the causes of pathologies, instillations of drugs are usually prescribed that, by their properties, can compensate for the lack of tear fluid for a certain period. This therapy is called replacement therapy.
- In some cases, the lacrimal openings are clogged with a kind of “plugs” in order to prolong the effect of the presence of tears.
- Anti-inflammatory therapy is prescribed in case of obstruction of the lacrimal ducts. According to obaglaza.ru, the most common cause of this pathology is inflammatory processes.
- Another option for solving the problem is surgical treatment with further administration of bougienage in order to restore the outflow tract.
Chronic obstruction of the nasolacrimal duct is eliminated by using dacryocystorhinostomy. During this operation, an anastomosis is performed, restoring communication between the lacrimal sac and the nasal cavity directly through the border bone wall.
Types of tears
Tears can be of two types: emotional and reflexive.
In ophthalmology, artificial tears are also distinguished. Tears appear due to the work of an entire system in the body. They can be reflexive and emotional, and in ophthalmology there is such a term as “artificial tears.”
Reflex
Such tears also have another name – “mechanical”; they actively cleanse and moisturize the eyes. If the fluid in question is produced in insufficient quantities by the lacrimal system of the visual organs, then problems may arise associated with drying out of the corneal layer and conjunctiva of the eye.
It is interesting that in old age the ability to self-hydrate the organs of vision is lost and therefore many characterize the eyes of old people as “faded, lifeless, dull.”
Emotional
It doesn’t matter what emotions a person experiences (negative or positive), tears can appear at any moment. Some people successfully restrain them, while others cry “with or without reason.” Scientists say that emotional tears (only sincere ones!) are very beneficial for health:
- relieve emotional stress;
- help relieve stress;
- bring psychological relief.
Interestingly, emotional tears can normalize and stabilize blood pressure, remove toxins and other harmful substances from the body, and promote the healing of the smallest wounds on the skin.
Artificial
Artificial tears are used in ophthalmology for severe dry eyes.
In ophthalmology, this term refers to special preparations that improve the hydration of the mucous membrane of the eyeball. Especially often, artificial tears have to be used by those people who spend a long time in front of computer monitors, are forced to work with printed documents, or are in a smoky room.
Artificial tears can only be used for a short time, otherwise addiction occurs and natural hydration of the mucous membrane of the eyeball does not occur. Ophthalmologists emphasize that if there is no positive effect, the use of the drug in question should be stopped and seek qualified medical help.