Forms
There are several types of eye damage in aphakia.
Determining the type of pathology depends on whether one eye or both are affected. Based on this, they distinguish: Aphakic eye
- Unilateral or monocular aphakia of one eye. With this form, as a rule, the lens is absent only in one eye. The monocular form of the disease may be accompanied by aniseikonia, in which both eyes see objects of different sizes. At the same time, all objects that fall into the field of view with one eye provide information about the shape and size of the image. In addition to aphakia, monocular vision occurs with monocular diplopia, monocular strabismus and monocular blindness. Diagnosing this form of the disease is not difficult for an experienced specialist.
- Bilateral or binocular form, which is often the result of severe cataracts. With this form, the lenses of both eyes are deformed, as a result of which the refractive abilities of the optical structure are disrupted. In the binocular form of the pathology, there is no accommodation, visual acuity is maximally reduced, and it is impossible to clearly see objects at different distances.
If the process is not stopped in time, both the first and second forms of aphakia will be complicated by additional diseases of the visual organ.
Pseudophakia of the right and left eyes
Artifakia. pseudophakia - lens examination performed previously. pseudophakia with other diseases of both or the better-seeing eye. Code according to ICD 10. International Classification of Diseases, 10th revision (ICD -10, By code, Enter at least three characters of the name or characters of the nosology code.
Class I - Certain infectious and parasitic diseases (776) {amp}gt;. Class II - Neoplasms (740) {amp}gt;.
Class III - Diseases of the blood, hematopoietic organs and certain disorders involving the immune mechanism (164) {amp}gt;. Class XV - Pregnancy, childbirth and the puerperium (423) {amp}gt;. Class XVI - Selected conditions arising in the perinatal period (335) {amp}gt;.
Causes
The main prerequisite for aphakia is eye injuries received either as a result of foreign objects entering the visual apparatus or unsuccessful surgical intervention. The nature of the congenital absence of the lens has not been thoroughly studied by science, due to the too small percentage of such cases.
Statistics show that the risk group mainly consists of people who have crossed the threshold of 40 years of age, in whom the processes of clouding of the lens may be activated - the development of cataracts. Untimely treatment of which, in most cases, contributes to the loss of the transparent body of the eyeball.
Surgeries to replace the lens of the eye
A complete diagnosis of the patient is a mandatory preoperative procedure. The ophthalmologist, together with the patient, determines the type of lens to be implanted, based on the safety of the ligaments, the condition of the retina, and the cornea.
On the eve of the operation to replace the lens of the eye, you are allowed to lead your usual lifestyle - eat, drink, take medications, except for blood thinning pills. Implantation of the replacement is carried out under general or local anesthesia. During the operation, the lens is softened and then removed with special instruments. The procedure takes no more than an hour.
Today there are 2 methods of lens implantation:
- ultrasonic phacoemulsification;
- femtolaser phacoemulsification.
Ultrasound surgery - a small incision is made on the surface of the eyeball, a phacoemulsifier is inserted to destroy the transparent body. Ultrasound waves impact the lens. Then the emulsion is pumped out using a special pump.
The posterior part of the capsule is not touched, becoming a barrier between the iris and the vitreous body. The doctor polishes the capsule, removing tissue, and installs the folded IOL. After implantation, it straightens out. There is no need to sew anything up, the tissues grow together on their own.
Femtolaser surgery is similar to ultrasound surgery, but uses a laser instead of ultrasound waves. The laser turns the lens into a homogeneous emulsion, which is subsequently pumped out.
Complications
Since, due to the absence of a lens, the vitreous body is held in place only by a membrane, it can bulge forward and form a hernia. If the hernia progresses, the membrane may rupture and vitreous fibers, along with blood clots, enter the anterior chamber.
As a result, the patient has a veil before his eyes, vision becomes blurry, and regular severe headaches occur. It is possible that the vitreous body may shift to the anterior pole and partially extend beyond the pupillary opening. If the hernia comes into contact with the corneal endothelium, severe and painful swelling may occur. Such processes can lead to the progression of visual dysfunction. Lack of treatment is fraught with:
- Distortion of the shape of the pupil.
- Development of glaucoma.
- Retinal detachment.
- Development of corneal dystrophy.
These diseases often cause complete blindness. However, timely and correct therapy can prevent the formation of a hernia, and if it does occur, reduce the size of the pathological protrusion. The vitreous body has the ability to repair itself.
Causes and symptoms
The main reason for fibrosis of the posterior capsule is considered to be the impossibility of ideally complete removal of the lens masses to be evacuated: invisible tiny particles remain, organically degenerate and begin to migrate in the space between the IOL and the capsule wall. Any opacity (or reduced transparency) on the main optical axis of the eye leads to deterioration of vision and the formation of various illusory artifacts in the field of view - luminous halos, balls, etc. However, the algorithm described here is extremely simplified: in fact, more and more new scientific data and ideas are emerging that force us to classify postoperative fibrosis of the posterior capsule (as a variant of secondary cataract) as a polyetiological, multi-causal phenomenon.
Causes
The leading factor that leads to the appearance of aphakia is the loss of the lens of the eye. This can happen due to trauma or penetrating injury to the visual organ, as well as after surgery to replace it, in the case of cataract treatment, for example.
The congenital form of aphakia, in which a child is born without a lens in the eye, is extremely rare.
Acquired causes of lens loss:
- Surgical cataract removal.
- Injury to the eye followed by loss of the lens.
- Dislocation or subluxation of the optical element.
Depending on the prevalence, aphakia can be monocular (when there is unilateral absence of the lens) and binocular (when there is bilateral loss of the lens).
Indications of pseudophakia
Indications for pseudophakia exist in the following cases:
- aphakia;
- glaucoma;
- cataract;
- presbyopia;
- radiation injury;
- lack of core;
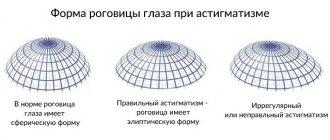
- extreme astigmatism;
- extreme myopia;
- chemical damage to the eye;
- dysfunction of the lens;
- hereditary, acquired violation of transparency;
- abnormal condition of the eye, congenital, acquired;
- removal of the lens during surgery;
- injury to the eyeball (damage, loss of the lens, destruction of the transparent biconvex lens).
Congenital defects are corrected after the age of 20, and occasionally, based on examination results, they are corrected earlier. Cataracts and aphakia are diseases that most often cause the installation of IOLs.
Aphakia is a congenital pathology acquired after injury. It can be one-sided, two-sided, the manifestations on the left and right are the same. Examining the eyeball, the ophthalmologist sees clouding of the pupil and trembling of the iris.
The appearance of aphakia, on the one hand, is the cause of impairment of binocular vision, manifested by a loss of the ability to judge the distance and shape of objects.
Associated symptoms:
- visual acuity quickly decreases;
- problematic focusing;
- image heterogeneity.
Cataracts can be congenital or acquired.
It appears as a result of injuries, in older people it is the result of age-related changes. Medications can be used to stop (rarely stop completely) the clouding, but it cannot be eliminated. Problems caused by cataracts:
- drop in visual acuity;
- development of diplopia – horizontal (less often vertical) splitting of objects. This causes headaches, anxiety, dizziness;
- dim lighting causes glare;
- light perception, visual acuity decreases at dusk;
- increased photosensitivity;
- color vision disturbance;
- the appearance of dark “flies”;
- white, gray spots around the pupil;
- Selecting lenses for glasses does not solve the problem of poor vision.
You should definitely visit an ophthalmologist if:
- there is even a slight decrease in vision;
- black "flies";
- distortion of the contours of objects;
- dark floating circles;
- veil.
Diagnosis of aphakia
If you promptly seek help from an ophthalmologist, it will be easier to diagnose and treat aphakia, and the chances of vision correction are higher. In aphakia, you need to examine the lens of the eye, namely its presence or absence.
To diagnose aphakia, the following studies are indicated:
- Visometry – makes it possible to determine the degree of decrease in visual acuity.
- Gonioscopy - shows how pronounced the deepening of the anterior chamber of the optical element is.
- Biomicroscopy of the eye using a slit lamp - the study is carried out in combination with visometry and ophthalmoscopy, it allows us to identify reactive changes in the eyeball in aphakia.
- Ophthalmoscopy - helps to assess the condition of the visual organ, as well as identify concomitant pathologies. Based on the results of ophthalmoscopy, treatment is selected.
- Refractometry - if the disease is one-sided, the study can determine how much the refraction is reduced. As a rule, these are indicators of 9.0-12.0 diopters in an aphakic eye.
- Ultrasound of the eye - with the help of this study it is possible to exclude or detect retinal detachment.
The main and visible diagnostic criterion is the trembling of the iris during the movement of the eyeball. This is the symptom observed in aphakia.
Analyzes
Tests are an important component of diagnosing any disease, and aphakia of the eye, in this case, is no exception. With the help of tests, it is possible to identify concomitant pathologies of a person, as well as find out his general condition at the time of the study.
For aphakia it is indicated:
- General blood analysis.
- Blood test for glucose levels.
- Blood test for RW and Hbs antigen.
- General urine analysis.
The results of the study show a detailed picture of the patient’s health; with their help, it is possible to prescribe correct and complete treatment.
Diagnostics
Physical examination reveals a decrease in the transparency of the anterior segment of the eyes, which may be combined with signs of traumatic injury. When the eyes move, phacodonesis develops, which is detected by an ophthalmologist under focal lighting. When performing a test with mydriatics, no reaction of the pupils is observed. Special diagnostic methods include the use of: • Non-contact tonometry.
When measuring intraocular pressure, it is possible to diagnose its increase.
IOP reaches critical values only when the outflow of aqueous humor is impaired. A mobile dislocation causes a slight increase in ophthalmotonus. • Visometry.
Visual acuity decreases sharply, regardless of the degree of transparency of the lens.
With the additional use of computer refractometry, it is possible to diagnose the myopic type of clinical refraction. • Ultrasound of the eye.
An ultrasound examination reveals a dislocation in the anterior chamber area or the vitreous body.
A unilateral or bilateral rupture of the ligament of Zinn is determined. The vitreal cavity has a non-homogeneous structure. When the lens is fixed to the retina, retinal detachment occurs. The anteroposterior axis is shifted. When completely ruptured, the capsule with the main substance acquires a spherical shape. • Biomicroscopy of the eye.
With the traumatic genesis of the disease, injection of conjunctival vessels and foci of hemorrhage are visualized.
The transparency of optical media is reduced. Secondary changes in the cornea are represented by microerosive defects. • Gonioscopy.
When the displacement vector is directed anteriorly, the volume of the eye chamber is sharply reduced.
In patients with an incomplete form of pathology, the space limited by the iris and cornea is deep, without pathological changes. The anterior chamber angle (ACA) has an uneven structure. • Optical coherence tomography (OCT).
The study makes it possible to determine the nature of the location of the luxated lens and the type of damage to the ligament of Zinn.
OCT is used immediately before surgery to select the optimal surgical tactics. • Ultrasonic biomicroscopy.
In the case of a congenital variant of the disease, the technique makes it possible to detect defects in the ciliary ligament over a range of 60° to 260°. The lens is displaced in the horizontal and vertical planes. The depth of corneal damage is measured. In case of traumatic origin of the disease, patients are additionally prescribed radiography of the orbits in direct and lateral projection. In the early postoperative period, IOP measurement using a non-contact method is indicated. To study the nature of the circulation of the intraocular fluid 5-7 days after surgery, electron tonography is used. The study determines the risk of developing glaucoma.
Lens implantation: indications and features of the operation
In medical terminology, aphakia is the name given to an eye that lacks a lens. Intraocular correction of aphakia is a surgical operation to replace the natural lens with an artificial lens (implant).
Pseudophakia is the result of surgery to insert an implant. An eye with an implant is called pseudophakic.
Indications for surgery
Implantation of an artificial lens is advisable:
– if the lens is damaged or removed;
- with clouding of the lens.
One of the common eye diseases is cataracts (clouding of the lens and its hardening), leading to decreased vision. If you do not operate, the lens becomes completely dense. Its size increases, which leads to increased eye pressure and, as a consequence, to glaucoma (an incurable disease).
Now almost 20% of the world's population after 40 years of age already have cataracts, and among older people more than 90% suffer from this disease.
Modern medical science is able not only to cure, but also to prevent the onset of many diseases. A person may not delay surgery on sore eyes.
For cataracts, pseudophakia is recommended.
Features and benefits of pseudophakia
Compared to other types of treatment, pseudophakia has clear preferences:
– the operation is safe (laser technology) and takes no more than 1 hour per eye;
– there is no cosmetic defect (the implant is completely transparent and similar to a natural lens);
– the visual field is completely preserved;
– there are no invisible areas in the field of view;
– there is no distortion of objects (typical for glasses);
– no need to wear glasses (or use contact lenses).
Complications of pseudophakia
Postoperative side effects are extremely rare. Their appearance depends on the type of lens, its quality, individual physiological characteristics, the condition of the eye before installation, and compliance with the rules of care after surgery.
Complications of pseudophakia are:
- secondary cataract – proliferation of tissue remnants;
- glaucoma is often a temporary phenomenon that goes away on its own;
- lens loss as a consequence of damage or careless actions;
- retinal detachment - can be eliminated with pulsed laser coagulation;
- macular edema forms in the center of the retina;
- infectious diseases, inflammatory processes;
- sensation of a foreign body - the artificial lens must be changed surgically;
- adhesive process when using unsuitable lenses;
- protein deposits are removed by cleaning with medicinal antiseptics.
Most often, complications arise after incorrect installation of the implant inside the eyeball, incorrect choice of lens type or size, failure to comply with hygiene rules by the ophthalmologist or postoperative care.
Eye pseudophakia is the correction of congenital and acquired eye pathologies in order to improve vision. The operations are safe and are carried out taking into account all examinations. The choice of IOL is coordinated with the patient and eye condition. Pseudophakia can restore 100% vision.
Ways to fight
For the treatment of aphakia the following are used:
- Glasses.
- Contact lenses.
- Intraocular lenses that are placed directly into the affected eye.
Ophthalmologists recommend using glasses in the presence of bilateral aphakia or if the patient has contraindications to wearing contact lenses. If the lens is missing in only one eye, the optimal treatment method is CL. Finding the right glass for a patient with aphakia is quite difficult. So, if the refractive power of the lens is 19 diopters, then even a glass lens of +10 diopters will be incomparable for such a patient.
In the presence of severe degrees of myopia, corrective lenses and glasses, as a rule, are not prescribed. In such cases, patients are advised to undergo lens implantation surgery. Contact or intraocular correction is also prescribed for monocular aphakia. The use of glasses by patients who have this diagnosis can lead to worsening aniseikonia.
If the doctor has prescribed intraocular correction to the patient, then before performing it, an artificial lens with the appropriate optical power is selected. It takes a certain amount of time to make such lenses. Most often, in the treatment of aphakia in ophthalmology, posterior chamber lenses are used, since they are installed in close proximity to the natural lens, thanks to which good quality of vision can be achieved.
Principles of IOL attachment
In general, there are currently three types of lenses. They accordingly have different designs and fastening principles:
- Anterior chamber IOLs. They are placed in the anterior chamber with support in the corner. This type of lens has to contact those areas that are most sensitive - that is, the iris and cornea. These lenses have a significant drawback - they provoke the appearance of synechiae in the corner of the area where they are located. Actually, that’s why they are used quite rarely at the moment.
- Pupillary IOLs. They are also called pupillary lenses, iris clip lenses, and ICLs. They are inserted into the pupil using the clip principle. The element is retained by the posterior and anterior haptic, that is, supporting elements. Our scientists, Fedorov and Zakharov, were the first to create such a lens. Their lenses were used back in the 60s of the last century, when intracapsular extraction was considered the best way to eliminate cataracts. The main disadvantage of such a lens is the possibility of dislocation of the supporting element or even the entire artificial lens.
- Posterior chamber or PCL. They are placed directly into the lens bag only after its complete removal or at least its nucleus. Cortical masses are also removed with extracapsular extraction. This type of IOL takes the place of the remote part of this section, becoming accustomed to the natural anatomically correct structure of the optical system of the eye. This type of lens helps provide a person with the highest quality vision. Posterior chamber lenses, better than other types of lenses, are strengthened in the area of placement and create conditions for creating a strong barrier between the anterior and posterior parts of the eye. The same type of lens helps prevent the development of pathologies such as retinal detachment, glaucoma, and so on. PCLs have contact only with the capsule where the natural lens was located. There are no vessels or nerve endings, and therefore inflammation, in principle, cannot develop. That is why this type of product is considered the most optimal in terms of quality and safety of use. Accordingly, it is used more often than other types in ophthalmic surgery.
Pseudophakia of the eye involves the use of any of the listed products to correct vision surgically. The materials for IOLs are usually the most hypoallergenic hard ones - polymethyl methacrylate, leucosapphire and others, as well as soft analogues made of silicone, hydrogel, silicone hydrogel, collagen copolymer, polyurethane methacrylate and so on.
Find out how rehabilitation should take place after cataract lens replacement surgery.
Products are made of multifocal or cylindrical type:
- Multifocals help correct myopia, farsightedness or eliminate the effects of cataracts.
- Cylindrical or toric IOLs are used to correct astigmatism.
Sometimes it is necessary to introduce two intraocular lenses into one eye at once. This is done if the optics of the fellow eye are not able to combine with the optics of the pseudophakic eye. That is why a decision may be made to introduce another lens into the area to correct the current situation. Accordingly, another lens is used, which has a degree of correction with the missing diopter.
You can find out about lenses for glasses for astigmatism, their selection and recommendations for choosing in the article.
Choose your contact lens solution according to experts and reviews here.
IOLs are biocompatible elements that, as a rule, have no consequences after insertion into the desired area. This type of lens is inserted into the eye through a micro-incision if the product is made of a soft material, or through a larger incision if a hard material is used. This factor is decided by the doctor who selected the lenses for you. The operation requires preliminary removal of the affected lens or part of it. The sooner the procedure is performed, the fewer consequences there will be for the patient.
Video shows how the eye works
ICD 10 code
There is no ICD code for this condition, since pseudophakia is not a pathological condition or disease, but rather refers to the period of recovery. Accordingly, if the operation was successful and no complications developed, then the ICD 10 code is not assigned. But in some cases, coding is provided for the following pathologies:
Types of IOLs
Size and installation method divides intraocular lenses into several types:
- anterior chamber;
- posterior capsule;
- pupillary;
- toric;
- posterior chamber.
Anterior chamber IOLs
implanted into the space between the cornea and iris, after making an incision.
Used for the following diseases:
- myopia;
- astigmatism;
- hypermetropia.
Anterior chamber implants
implanted in people with significant contraindications to laser correction. The use of LPO significantly simplifies the surgical technique; some types can cause complications. Anterior chamber lenses are made of polymethyl methacrylate and have a service life of about 100 years.
Posterior capsular IOLs
Use only when the lens is completely removed. They are implanted into a capsule. STAAR is the only company that produces substitutes that meet international requirements.
Pupil lenses
available for secondary installation. For installation, use an injector, a cartridge, inserting it through an incision. Implants have a lot of disadvantages, such as instability and a tendency to move. They do not create pressure on the cornea.
Toric implants
combine the advantages of cylindrical and spherical varieties. Such lenses are installed for cataracts, astigmatism, all kinds of corneal pathologies and other diseases. Toric lens substitutes are contraindicated in severe diabetes mellitus, iritis, iridocyclitis, and siderosis.
Posterior chamber implants
used in 90% of ophthalmic surgeries. They are notable for the fewer side effects they cause. Lenses of this type are visually invisible to an outsider and imperceptible to the patient. It can be installed after removing the natural nucleus into the lens bag, the posterior chamber. IOL prevents retinal detachment and glaucoma.
The choice of a specific type of lens is based on the type of pathology, research results, the condition of the cornea, and the financial capabilities of the patient.
All lens substitutes are divided into groups:
- Spherical, aspherical.
The latter type guarantees a contrast image, a wide viewing angle, and no glare. - Monofocal, multifocal.
The latter ensure normal focusing of vision and correct presbyopia. There are toric varieties for the correction of astigmatism. - Accommodating.
A pair of parallel lenses that move due to muscle tension, changing the distance to the focal point. - With protective functions they are the most expensive and protect against ultraviolet rays.
They come in yellow or blue. The choice of one or the other does not affect the perception of the color scheme.
First symptoms
How can a person determine that he needs pseudophakia of the eye? What it is? Of course, only a qualified medical professional can make a verdict; he also describes the essence of the problem, ways to eliminate it and possible consequences. You should consult a doctor when you feel even a slight decrease in vision: for example, there are “flying spots” in front of your eyes or you see objects distorted. These symptoms may be the first signs that will inspire you to seek help in time.
Remember that there is no need to delay. While for some people cataracts take years to develop, for others the condition worsens in just a few weeks. At the stage of a “mature” problem, a person no longer sees practically anything: he only distinguishes light from darkness. It is clear that at this stage glasses will no longer help the patient: an indestructible barrier inevitably stands in the way of the lenses - a cloudy lens, which can only be corrected surgically
You should also pay attention to the fact that neither alternative medicine nor self-medication will save you from the disease. On the contrary, they can lead to a worsening of the condition and even many negative consequences.
Why is the operation performed?
Surgical intervention helps to get rid of eye pathologies, both congenital and acquired. Implantation of a new lens is only necessary if the old one is damaged! Indications for pseudophakia of the right or left eye are the following pathological changes, namely:
- structural defects;
- serious disorders of the lens that cause blurred vision;
- absence or damage to the lens;
- birth defect. The operation is performed only in adults after twenty years of age;
- cataract;
- eye injury that leads to destruction or loss of the lens.
Cataract is the main indication for surgery. As a result of pathology, the lens loses its transparency, becomes cloudy and thickens. As a result of structural changes, vision deteriorates and sometimes is completely lost.
The operation is prescribed by a qualified doctor after undergoing a diagnostic examination. A timely visit to a specialist will help you perform the operation on time
What should you pay attention to?
The first sign of a developing pathology is the appearance of “floaters” before the eyes. Patients note that something begins to fly before their eyes, objects are distorted, or vision simply decreases. This is a serious reason to see a doctor. Cataracts are easier to treat in the early stages of its development, like any other disease.
Artifakia will help you get rid of lenses and glasses
In some cases, cataracts develop over several years, and sometimes progress in a few weeks. In severe cases, patients begin to see so poorly that they can barely distinguish light from dark. The use of traditional methods in this case is a waste of time. This can lead to the fact that the operation will not help, which is why the person will simply lose his sight.
Speaking about cataracts, a large role is played by the hereditary factor. This disease is also considered a pathology of older people.
Loss of lens properties leads to the following changes:
- age-related farsightedness;
- age-related cataract;
- lenticular astigmatism.
The lens replaces a damaged lens. It is not rejected by the body and is completely biologically compatible
Short description
Cataract is a disease characterized by varying degrees of persistent opacities of the substance and/or capsule of the lens, which are accompanied by a progressive decrease in human visual acuity.
Etiology • Senile cataract •• Long-term (lifelong) increase in the layers of lens fibers leads to compaction and dehydration of the lens nucleus, causing visual impairment •• With age, changes occur in the biochemical and osmotic balance necessary for lens transparency;
the outer fibers of the lens become hydrated and become cloudy, impairing vision • Other types •• Local changes in the distribution of lens proteins leading to scattering of light and appearing as lens opacities •• Injuries to the lens capsule result in aqueous humor entering the lens, clouding and swelling of the lens substance.
Classification by appearance • Blue - the clouded area has a blue or greenish color • Lenticular - clouding of the lens while maintaining the transparency of its capsule • Membranous - foci of clouding of the lens are located in strands, which imitates the presence of a pupillary membrane • Capsular - the transparency of the lens capsule, but not its substance, is impaired • Tremolding - overripe cataract, eye movements are accompanied by trembling of the lens due to degeneration of the fibers of the zonular ligament.
Classification according to the degree of progression • Stationary (most often congenital, opacification does not change over time) • Progressive (almost always acquired, opacification of the lens increases over time).
• General symptoms •• Painless progressive decrease in visual acuity •• Fog before the eyes, distortion of the shape of objects •• Ophthalmological examination reveals clouding of the lens of varying severity and localization.
• Senile cataract •• Initial - decreased visual acuity, clouding of the subcapsular layers of the lens substance •• Immature - visual acuity 0.05–0.1; clouding of the nuclear layers of the lens, swelling of the substance can provoke the development of pain and an increase in IOP due to the appearance of secondary phacogenic glaucoma •• Mature - visual acuity below 0.05, complete diffuse opacification of the entire lens •• Overmature - liquefaction of the lens substance, the appearance of vacuoles (cavities filled liquid), the lens takes on a pearlescent appearance.
• With nuclear cataracts, myopia initially occurs against the background of existing presbyopia (myopizing phacosclerosis); the patient discovers that he is able to read without glasses, which is usually perceived positively by the patient (“second sight”). This occurs due to hydration of the lens during initial cataracts, which leads to an increase in its refractive power.
Special studies • Qualitative assessment of visual acuity and refraction; in case of a pronounced decrease in visual acuity, tests are indicated to determine the localization in space of a bright light source. Possible hyperglycemia in diabetes can cause osmotic changes in the lens substance and affect the results of studies • Determination of retinal visual acuity (the isolated ability of the retina to perceive visual objects, while the state of the refractive media of the eye is not taken into account;
determination is made using a directed beam of laser radiation). A similar study is often carried out in the preoperative period in order to accurately predict postoperative visual acuity. • Retinal angiography with fluorescein is indicated to identify concomitant pathology when visual acuity does not correspond to the degree of lens opacity.
Management tactics • Senile cataract •• The process develops gradually, so usually the patient does not realize how pronounced the pathological changes are. Against the background of formed habits and skills, even significant clouding of the lens is perceived as a natural age-related weakening of vision. Hence the need for a thorough explanation to the patient of his condition •• The initial stages are the use of agents that slow down the progression of the pathological process, sometimes even transferring the cataract to the stationary stage.
Gender factor
A number of epidemiological studies using cross-sectional data have shown that women are at higher risk of developing cataracts compared to men. Some results indicate a general increase in the incidence of this disease. Most investigators report a higher prevalence of cortical cataracts, with only one study showing a higher prevalence of nuclear cataracts among other types (Am J Ophthalmol 1999; 128:446–65). The mechanism of the influence of the gender factor on the occurrence of cataracts is not clear, but may be associated with hormonal differences between women and men.
One reason may be postmenopausal estrogen deficiency. Recent epidemiological data provide some evidence that estrogen and hormone replacement therapy may play a protective role in the development of age-related cataracts (Am J Epidemiol 2002; 155:997–1006). Data from the Beaver Dam Eye Study suggest that early age at menarche, long-term use of estrogen-containing medications, and use of birth control pills prevent the development of nuclear cataracts. The latest Beaver Dam Eye Study assessed the possible association between reproductive age and the incidence of cataracts. The only significant result was the identification of a trend towards a decrease in the incidence of posterior subcapsular cataracts due to an increase in the number of successful deliveries.
Correction methods
The problem of aphakia can be solved using conservative methods or surgical intervention. The latter is more preferable, as it allows you to completely restore binocular vision.
Conservative therapy
You can increase the visual acuity of an aphakic eye with the help of:
- Points. They are indicated only for patients with bilateral aphakia. Usually you need two pairs: for near and far. Although, if visual impairments, for example, severe myopia, were diagnosed before the removal of the lens, then patients may not need distance glasses. To correct vision, the glass must be strongly positively convex (from +8 to +17 diopters).
- Contact lenses. This is a modern and most common way to solve vision problems. A huge advantage of the method is the possibility of application for both unilateral and bilateral aphakia. The type of material from which the lenses are made depends on the age of the patient. Thus, special soft silicone lenses are produced for newborns, and soft, breathable or hard ones for older children. But you can resort to their help no earlier than 4 weeks after surgery to remove the affected lens.
Strong plus glasses can cause annular scotoma, that is, the patient loses an entire area of vision, which leads to painful sensations from the regular sudden appearance of one or another object in front of the eyes. This significantly complicates the lives of patients, as it is difficult for them to cross busy intersections, etc.
Surgery
Surgery to install an intraocular lens (IOL) is used after lens removal.
The presence of an artificial lens in the eye is called pseudophakia, and the eye is called pseudophakic
This type of vision correction is a surgical procedure for installing an artificial plastic lens of a certain strength, the value of which is calculated using specially created computer programs and tables, taking into account:
- lens thickness;
- refractive power of the cornea;
- depth of the anterior chamber;
- length of the eyeball.
Its implementation is possible only after the final formation of the eye structures, which usually occurs by 2 years. Therefore, when treating children with congenital aphakia before reaching this age, it is necessary to use glasses or contact lenses.
There are 4 different types of IOLs, differing in how they are inserted:
- with fixation in the corner of the anterior chamber;
- iris clip lens (pupil);
- extracapillary;
- posterior chamber.
The optimal option is a posterior chamber IOL, which does not interfere with normal pupil dilation and provides better quality of vision, since it occupies the natural place of the lens.
Previously, other operations were used to restore the quality of vision in patients with aphakia, but due to their imperfections and the frequent lack of positive changes, they have not been carried out in recent years.
Types of intraocular lenses
IOLs by size and installation methods
- Anterior chamber IOLs. They are installed, as the name suggests, in the anterior chamber of the eye, on the frontal part of the eyeball. The use is limited, since in most people, due to the typical characteristics of the eye, contact of the IOL with the cornea and iris may occur, which can cause the appearance of synechiae (adhesions) in the corner of the anterior chamber. Complications also include iridocyclitis and bullous dystrophy. The most common material for anterior chamber IOLs is polymethyl methacrylate, a material that has ideal transparency, close to a healthy lens. During implantation, a small incision is made into the cornea, which is then closed with a suture made of absorbable threads.
- Pupillary or pupillary. They are embedded directly and directly into the iris tissue surrounding the pupil, like a clip. Easy to install, they do not interfere with the eye in performing its functions, but can fall out due to impact injuries.
- Posterior chamber. Since it replaces the removed lens in its bag, this position of the IOL is natural and the safest from a physiological point of view. Such a lens corresponds to the removed lens, contacting only the walls of the capsule, in which there are no nerve fibers and blood vessels. As a consequence, with such pseudophakia, inflammatory processes are impossible, due to which implant rejection may occur. It is used in 90% of surgical cases and is actively recommended by doctors. They are invisible to others, unlike the anterior chamber or pupillary (if you look closely, they are visible, since at the border of the media the light breaks somewhat).
As a variety of the latter, posterior capsular IOLs are used - such IOLs are placed when the natural lens is completely removed. The fastening is made in the capsule.
Lens materials can be hard or soft. The best imitation of natural materials are IOLs made of hydrogels, similar in texture and structure to lenses for contact optics used for everyday wear.
By type of pathology or conditions of the cornea
- spherical and aspherical, of which the latter is preferable due to a wider field of view and maximum contrast of the image being built on the retina. In addition, such lenses completely eliminate the formation of intrabody glare;
- with a monofocal or multifocal structure. The former, due to the simplicity of their design, are not able to completely imitate the work of a living lens, and the patient may experience difficulties with accommodation, that is, assessing the distance to the object in question. They require additional wearing of glasses, “plus” or “minus”, depending on the distance the monofocal lens is designed for. The latter, due to the presence of several focusing zones, are devoid of this drawback and are able to correct presbyopia - farsightedness inherent in old age. There are also toric lenses that correct astigmatism. Indicated for patients who have undergone corneal transplantation. Multifocal lenses are most often installed if there are problems with the optic nerve;
- intraocular lenses with protective function. The most advanced, but most expensive artificial products. They have a yellow or blue tint in reflected light, but this does not affect color perception in any way. This property, associated with opalescence, protects the tissues of the eye, and especially the retina, from UV radiation.
- AIOL. Accommodating lenses. Composite lenses have a double structure consisting of a pair of parallel lenses with different degrees of curvature. When the eye muscles are tense, such lenses move and are able to change the focal length of the artificial lens no worse than a real, healthy one.
Types of congenital cataracts of the eye
Cataracts are conventionally divided into two types:
- one-sided;
- bilateral.
Cloudiness of the lens in both eyes more often leads to complete loss of vision and is more difficult to treat than the unilateral variant of the pathology.
Based on the location of the cloudy spot in the lens area, the following types of disease are distinguished:
- front;
- back;
- nuclear;
- layered;
- complete.
Anterior and posterior cataracts are characterized by the presence of opacities in front and behind the center of the lens, respectively.
These types of disease can be capsular (when only the body of the lens is affected) or polar (when the cloudiness spreads to the soft tissue surrounding the lens).
The anterior capsular type of the disease in most cases (more than 80 percent) has hereditary causes and does not have a significant effect on the quality of vision or causes slight myopia.
Reference! With nuclear cataracts, when the cloudy spot is located in the optical center of the lens, visual impairment is always present.
Nuclear cataracts have hereditary causes and are difficult to treat.
With a complete cataract, the lens is completely opaque, since all its layers are affected. Loss of vision with this pathology reaches 100 percent, the patient has only weak photosensitivity.
Accompanying illnesses
Cataracts of each type, depending on the causes of its occurrence, can be complicated by concomitant eye diseases, including:
- colomba;
- hypoplasia;
- nystagmoma, etc.
Photo 2. Lens colombus: this disease often complicates cataracts.
Before treatment, the doctor determines the exact subtype of the disease.
Preoperative diagnosis
Before the operation, a detailed diagnosis of the condition of both the visual organs and the entire body is required, involving a complex of laboratory tests. The type of lens to be implanted is discussed with the ophthalmologist, especially if it will be monocular and after its implantation you will need to wear glasses.
The safety of the ligaments and the general condition of the cornea are taken into account, because there may be cases of contraindications to implantation.
Artifakia step by step:
- A day before the operation, another, additional examination is carried out according to a full or shortened cycle - depending on the general condition of the patient.
- On the morning of the operation, the daily routine is no different from the usual. That is, you can eat, drink, take medications prescribed by an ophthalmologist or other doctors - except for blood-thinning anticoagulants.
- Anesthesia is administered on an operating table or even on a sterile hospital bed by injecting anesthetic agents into the eye(s). They are local anesthetics and do not interfere with the patient’s ability to talk and perceive their surroundings. But general anesthesia can be used - according to indications or at the request of the patient, if he is afraid of instruments. Moreover, he will see them; psychologically, not everyone can bear this.
- The lens, which has become clouded and has lost its functionality, is crushed to an emulsion state with a laser or ultrasonic beam, and then sucked out with a special micropump through a small 2 1.5-2 mm hole.
- A rolled-up lens is inserted into the freed lens capsule with an injector, which immediately straightens out and takes the place of the removed organ and is fixed there.
- The micro-hole through which the implant was inserted into the eye chamber is closed.
This operation takes no more than half an hour, and its advantage is that the rehabilitation period is short, and the occurrence of complications is extremely rare.
Treatment
There are several methods to restore eye health to patients suffering from aphakia; the choice of one approach or another is determined by the results obtained when making a diagnosis and depends on the degree of advanced disease.
Since after the loss of the lens, the refraction of the eyeball (the ability to refract light) changes significantly, therefore the main goal of the fight against aphakia is to correct the refractive ability of the eye that has lost its natural lens. Below we will look at the existing possibilities.
Treatment with medications
Unfortunately, humanity and world science have not invented drugs that allow us to grow a lost organ. In nature, there are no tablets or injections capable of growing a lens inside the eyeball of the desired shape and properties.
| Therefore, drug therapy for aphakia is devoid of all common sense and is not carried out. Medicines are used as an adjunct to other methods. |
Glasses
After surgery to remove the lens, the eye's ability to refract light directed into it changes significantly. The patient's farsightedness increases significantly. The refractive power of the amputated organ is compensated by auxiliary optical means - glasses.
To correct aphakia of the eye, a glass of at least +10.0 ÷ +12.0 D is required, which is significantly less than the refractive power of the lost lens, which, as a rule, is +19.0 D. This difference is due primarily to the fact that the lens of the glasses located differently, in a different place in the rather complex optical system of the eye.
Secondly, the lens installed in glasses is surrounded by air with completely different optical properties in terms of refraction, in contrast to the lens, which is physiologically immersed in the vitreous fluid, which has a similar refractive index of light.
For a person suffering from farsightedness, the optical power of the glass must be increased by the required diopter values; for a person suffering from myopia, it must be reduced, ultimately using glass of a smaller thickness.
For example, if before the removal surgery myopia was close to -19.0 D, then after surgery, due to the bringing of the optical system into a state of equilibrium, the patient may be able to do without glasses necessary for seeing objects located at a considerable distance.
An aphakic eye loses its ability to adapt, so for near work, 3.0 D glasses are prescribed more powerful than lenses for distance. Correction with glasses is not done if there is no lens in one of the organs of vision.
An eyepiece of +10.0 D or more is a fairly powerful magnifying glass. In the case when it is present only in front of one eye, the resulting images in both eyes are too strikingly different from each other in size and geometric dimensions, and they will never merge into a solid picture.
In other words, the patient will lack binocular vision, which is fraught with serious dangers for his life: the inability to estimate distances to objects, the inability to see the whole picture of the world around him here and now.
Contact lenses
Previously, a fairly advanced method of vision correction is used precisely in cases where the patient is diagnosed with monocular aphakia. As you know, in such a situation, the use of glasses is contraindicated, for the reasons discussed earlier. And the solution is to use individually made lenses.
Surgery
| A modern method of getting rid of aphakia is vision correction, carried out by implanting an intraocular lens (IOL) into the diseased eye. The procedure is prescribed for patients with monocular aphakia. |
The essence of the intervention is the replacement of a lost or amputated lens with an artificial lens of the required optical power, implanted into the eyeball through surgery. This method is recognized as the best in getting rid of the disease.
Folk remedies
As in the case of drug treatment, alternative medicine against aphakia of the eye is powerless. No decoctions, healing herbs, conspiracies or rituals can return the removed lens to the eye.
If you come across offers of help to overcome an illness in one or another “grandmother’s” way, by making an appointment with a “healer,” you should know that these are charlatans who are only interested in your money.
What is traumatic cataract, causes of occurrence, ICD 10 code
According to the International Classification of Diseases (ICD-10), traumatic cataract is assigned code H26.1.
There is no single set of characteristics that takes into account all the factors of this type of disease.
The degree of progression of the disease depends on the speed of damage to the eye: either a slow course or a fast course. In some cases, cataracts may not progress.
Kinds
- mechanical, penetrating and contusive;
- chemical (toxic);
- radial;
- professional.
Contusion cataract occurs either immediately after injury, or a little later. There are many subtypes of the disease, but the main ones are:
- Vossius ring-shaped cataract. It is characterized by clouding of the anterior part of the lens, most often due to blunt trauma to the eye. A pigmented ring is formed on the front of the lens, consisting of cells in the rim of the pupil. Resorption of this ring may take several weeks or months.
- Rosette contusion cataract. Stripe-like opacities form, collecting in the center of the rosette. Vision deteriorates gradually.
- Total cataract. It is characterized by a rupture of the lens capsule or its contusion. The prognosis is the most unfavorable.
Important! In mild cases of ring-shaped and rosette cataracts, the eye may self-heal and restore its functions. Types of chemical traumatic cataracts are divided according to the type of substance that caused the damage
These include:
Types of chemical traumatic cataracts are divided according to the type of substance that caused the damage. These include:
- Alkali burn. In the case of a burn with a similar substance, the damage to the eye is not immediate; the pathology develops gradually.
- Acid burn. Acid has a very aggressive effect on tissue, so pathology appears instantly, immediately after the substance enters the organ of vision. Not only the eyeball is affected, but also nearby tissues.
- Burns and intoxication with other substances. The eye lesion may go away over time. When the whole body is intoxicated, the motor function of the eye is impaired, and the symptoms are associated with general poisoning.
Photo 1. An acid burn to the eye, as a result of which cataracts immediately appear. Surgery is required to remove it.
Radiation cataracts do not develop instantly; the period of manifestation can last more than 10 years. The lens of the human eye is sensitive to X-rays, infrared radiation, and microwave waves. A peculiarity of this type of lens damage is the appearance of colored waves on a gray background.
Occupational cataracts are caused by working with heat sources, with objects that can introduce a foreign body into the eye, for example, with a welding machine.
If the lens is damaged, fluid from the eyeball will enter it and its functioning will be disrupted. This is often accompanied by a shift of the lens from its place - dislocation or subluxation. Getting a foreign body or liquid into the eye further complicates the course of the disease. An injury larger than 3 mm, especially complicated by displacement, cannot heal on its own and the patient requires urgent medical attention.
Attention! Most traumatic cataracts are accompanied by changes in several structures of the eyeball
Prevention
Timely lensectomy in 2/3 of cases makes it possible to completely restore visual acuity and normalize the circulation of intraocular fluid. 30% of patients develop severe postoperative complications. Specific methods of prevention have not been developed. Non-specific preventive measures include the use of personal protective equipment when working in production conditions (goggles, masks). To reduce the likelihood of dislocation, patients with hypermetropic refraction are advised to correct visual dysfunction using glasses or contact lenses.
Source
Severe forms of ophthalmological diseases often lead to loss of vision, which cannot be restored using folk or medical means. The optimal solution is to install an intraocular lens (IOL), which can restore full visual perception of surrounding objects. Features of surgical intervention, indications, contraindications, complications are described below.
Pseudophakia is not an ophthalmological disease, but the result of its treatment. Essentially, this is the implantation of an artificial object inside the eyeball through surgery. Sometimes the procedure for installing an intraocular lens substitute is called this, and the eye is called artificial.
Intraocular lenses are made from an artificial type that is biologically compatible with human tissue. Substitutes are made from hard materials - leucosapphire, polymethyl methacrylate, and soft ones - copolymer, collagen, silicone, hydrogel.
Thanks to laser and ultrasound technologies, operations to remove a clouded, injured lens and install an artificial lens are safe, and complications are rare. Often, IOL implantation becomes the only possible solution to restore vision; installation of two or more objects is possible in severe cases.
In the international classification of diseases ICD-10
Pseudophakia is coded
H26.0
(other cataracts).
Before correction with glasses or contact lenses, IOL implantation has a number of advantages:
- restores full visual functions;
- the implanted object is self-sufficient;
- the contours of objects are clear;
- there are no blind spots.
Let's sum it up
The code classification allows for continuous improvement of health care for all people, regardless of where they live. The collected statistics of health problems systematize knowledge, record data on mortality, its causes, and determine the threshold of morbidity in each country at a certain time.
Why do we need it? To know everything about the problem that has arisen. This will help in the fight against it and protect against complications. It’s not for nothing that people say: “Aware means armed.” For a doctor, such a code is a good help. If such a code classification did not exist, he would have to describe a long diagnosis on each sick leave.
In addition, doctors have a good opportunity to use the collected material, which allows them to make an accurate diagnosis for the patient. And accordingly, choose the right treatment methods. The World Health Organization uses it (ICD) to improve health services.