Occlusion (embolism, obstruction, thrombosis) of the central retinal artery
Before embarking on a review of the designated topic, it is necessary to clearly define the concepts included in the title and differentiate them - in order to avoid confusion that is so common in our time.
Any vessel or duct participating in the complex system of circulation of biological fluids in the body (be it blood, lymph, bile, urine, etc.) must perform its functions uninterrupted. To do this, the lumen of the vessel must remain exactly as nature created it - no more and no less - otherwise the laws of hydrodynamics will inevitably change the pressure of the transported liquid, which will lead to its excess or, conversely, its deficiency at the “destination”. For the body, this always means serious problems.
If we talk only about the circulatory system, then in a number of areas of medicine there is the term “vascular catastrophe,” meaning a sudden blockage of a blood vessel. More precisely, perhaps, you cannot say here: this is precisely a catastrophe in a local area, since a deficiency or cessation of blood supply (ischemia) quickly leads to necrosis, the death of working cells of a tissue or organ on a certain scale (depending on the caliber and significance of the blocked vessel and the organ being supplied ) – a heart attack occurs.
The most famous and clear examples of what such conditions mean for the body as a whole are coronary heart disease and myocardial infarction. But not even a complete, but only a partial reduction in the standard volume of blood that should flow through the arteries or drain through the veins ultimately leads to equally catastrophic consequences: dystrophy gradually develops (a state of constant deficiency of nutrients and oxygen bound by red blood cells), a decrease and “drying out” of the starving tissue/organ, then atrophic degeneration begins, i.e. disintegration of high-molecular proteins and degeneration, replacement of parenchymal (functional, specialized) cells with universal and useless, in this case, connective tissue, as well as its scarring (fibrosis) with growth in size and compaction. Various options for vascular obstruction are possible, and none of them are safe. Stenosis is a persistent narrowing of the lumen, for example, due to thickening of the vascular walls for any reason.
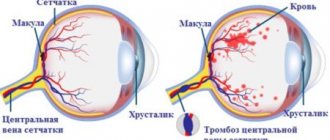
Thrombosis is a complete or partial blockage of a vessel, for example, by a detached and migrating atherosclerotic fatty plaque or a clot of coagulated blood. Occlusion is a complete and, in the literal sense, hopeless closure of a vessel, i.e. lack of even minimal lumen and blood flow. Thus, thrombosis in its extreme form means occlusion, but partial thrombosis does not. Embolism is a synonymous term used to designate blockage of a vessel by any body or particle in general; This is not necessarily a blood clot - an embolus can be, for example, a gas bubble that gets inside a vessel (the original meaning of the ancient Greek word “embolos” is “gag”, “plug”, “plug”, etc.).
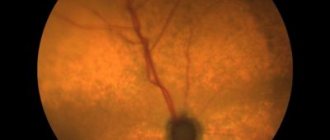
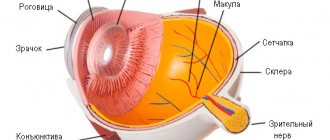
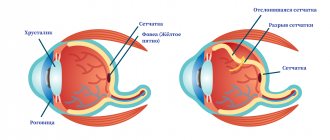
Returning to the topic, let’s imagine a very thin, very fragile, not very well protected and not equipped with uninterruptible power supply systems, but normally a perfectly tuned and balanced optical-biomechanical system called the eye. Along the inner surface of the back wall of the eyeball, - on the so-called. the fundus of the eye - its most important functional tissue, or retina, is located in a thin layer. The retina consists of receptor cells saturated with light-sensitive enzymes and is nourished by the underlying choroid. Approximately in the center of the most sensitive zone (“macula”, “macula”) the retina is fused with the receiving disc of the optic nerve (OND), where the optical image is “digitized” into electrochemical signals-impulses and in this form is transmitted further along the nerve to the visual cortex of the brain brain The largest vessels in the circulatory system of the eye are located along the optic nerve: this is the central retinal artery (CRA), from which blood saturated with oxygen and nutrition is supplied to the smaller branches and smallest capillaries of the retina, as well as a paired vessel for draining waste blood that has released nutrients, also carrying away metabolic products (metabolism) - the central retinal vein (CRV).
Since functional retinal (retinal) tissue is very thin and vulnerable, the slightest problems with its blood supply and nutrition lead to degenerative changes (the most common and well-known example is diabetic retinopathy), and with a stable and long-term worsening of such problems, the retina simply detaches from the choroid. Nutrition, oxygenation (oxygen saturation), as well as the processes of formation of visual images and transmission of signals to the brain stop at this point. Blindness sets in.
The attentive reader, now fully armed with an understanding of the terms, can then independently model the catastrophic picture of what happens to the retinal tissue during thrombosis, embolism and/or, in the worst case scenario, occlusion of the central vein or central retinal artery. The CAS is blocked approximately one and a half times less often than the central vascular system, but the consequences of thrombosis/occlusion of the artery develop more rapidly and turn out to be more (even more) severe than with blockage of the vein.
In addition to atherosclerosis and hypertension (arterial hypertension), as well as damage to the vascular walls in diabetes mellitus, arterial occlusion can be caused by acute and chronic vascular inflammation (vasculitis, giant cell arteritis), ocular ischemic syndrome due to stenosis, compression of the artery by an oncological neoplasm or fibrous tissue. Complete or partial blockage can occur both in the main artery itself and at any point in its basin, i.e. systems of branches and capillaries; in the first case, the ischemia is extensive and total, on a retinal scale, in nature, in the second - local, affecting a more or less limited area.
↑ Arterial occlusion
Classification.
Since various factors play a major role in the mechanism of PCA in the CAS and its branches (acute spasm, embolism, which can be caused by damage to the heart valve, disintegrating atherosclerotic plaque of the carotid artery or collateral blood flow tracts, as well as blood clots forming in the heart cavity), acute arterial obstruction according to its localization: occlusion of the central nervous system; occlusion of vascular arcades (superotemporal, inferotemporal, superonasal, inferonasal).
Basic position. It is necessary to try to restore blood flow
by massaging the eye and lowering IOP if the patient consults a doctor on the day of vision loss.
Diagnosis
History (list of necessary information)
? To find out the cause of the embolism
(the embolus can be hemorrhagic, bacterial, contain cholesterol, calcium, lipids): arterial hypertension, atherosclerosis (carotid artery in 45% of cases with a 60% degree of narrowing or more in 20% of patients, age 40-60 years); endocarditis, mitral valve prolapse, myocardial infarction (embolism from the heart is the most common cause of CVA in patients under 40 years of age); myxoma of the heart, administration of intravenous contrast diagnostic agents, pancreatitis, Purcher’s disease - lipid embolism; obliterating endarteritis (rare etiology - 2% of cases, but this pathology must be considered in elderly patients unless another cause is found, especially since damage to the other eye cannot be ruled out).
? To find out the cause of vasoconstriction
: nervous stress, giant cell arteritis, collagenosis, vasculitis, oblique discharge and drusen of the optic disc, cystinuria, use of contraceptives, hormonal disorders; Bleeding disorders (coagulopathy in sickle cell anemia), as well as antiphospholipid syndrome and migraine are the most common cause of CAC in patients under 30 years of age.
? To determine the cause of vascular compression
: acute attack of glaucoma, retrobulbar hematoma or retrobulbar injection of drugs, severe arterial hypotension, in which the pressure in the retinal arteries is below IOP.
The history is typical of sudden loss of vision in a previously healthy eye, not accompanied by pain.
Physical examination and clinical picture
? Visometry.
Suddenly and quite sharply vision decreases, most often in the morning, up to complete blindness.
Visual functions may fluctuate from zero to 0.08 eccentrically. In 12% of cases, this may be preceded by short-term transient blindness, flickering, and the appearance of sparks. About 20% of patients are able to determine only the presence or absence of light. ? Perimetry.
Narrowing, sectoral loss of visual field, amaurosis. When the branches are affected, sectoral absolute scotomas do not reach the point of gaze fixation by 2-10° or merge with absolute central scotomas in the case of damage to the macular zone of the retina.
? Biomicroscopy.
The reaction of the pupil to light is sharply reduced or absent.
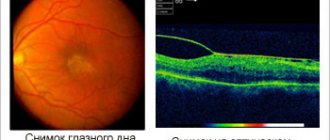
? Ophthalmoscopy.
The fundus shows a typical picture:
? Retinal swelling increases within a few minutes
. It acquires a milky white color, against which a cherry-red spot of the central fovea of the macular region stands out (a contrast phenomenon, a “cherry pit” symptom).
? In the initial stage, the optic disc has a pink color, the borders are somewhat blurred due to swelling of the surrounding retina. The arterioles are sharply narrowed, of uneven caliber, the blood flow in them becomes segmental.
? At a later stage, the arterioles are obliterated, the veins are narrowed due to a decrease in blood flow. Thrombotic phenomena often develop in them secondarily.
? In the case of CAS in the branches of the central nervous system, the changes described above develop in the zone corresponding to the blood supply to the affected branch. Of the branches of the CAS, the temporal (especially the upper) branches are most often affected.
? The acute period of the disease is short-lived. After 2-3 weeks, the process begins to reverse, and after 4-6 weeks, retinal edema completely disappears, but is replaced by secondary degenerative and atrophic changes in the fundus tissue.
? In the presence of a cilioretinal artery (anastomosis between the posterior short ciliary and retinal arteries, present in 15-30% of eyes), it is possible to preserve the zone of normal blood circulation in the form of an island, which in some cases allows maintaining vision at a higher level. On the other hand, ONC may arise precisely in the cilioretinal and opticoretinal branches. In this case, patients note the appearance of a positive central scotoma, and defects in central and peripheral vision depend on the size of the retinal infarct zone.
? Fluorescein angiography.
There is no contrast in the distal part of the affected artery, or the patency of the vessel is preserved, but its sharp narrowing and uneven segmental blood flow are observed.
? Electrophysiological study
. With ONC in the trunk of the central nervous system there are signs of attenuation and the appearance of a negative ERG, a decrease or complete absence of optic nerve conductivity. ERG changes depend on the extent of the ischemic process.
Laboratory and other studies
? Complete blood count (erythrocytes, platelets), determination of ESR (temporal arteritis).
? Blood coagulogram.
? Study of blood clotting indicators (fibrinogen, prothrombin, bleeding time).
? Diagnosis of antiphospholipid syndrome
(the symptom complex includes venous and/or arterial thrombosis, thrombocytopenia, neurological, cardiovascular and hematological disorders). The titer of antiphospholipid antibodies of the IgG and IgM classes of blood plasma to cardiolipin is determined using the enzyme immunoassay method. If antiphospholipid syndrome is detected: patients are observed by general practitioners and treatment is carried out for life to prevent thrombosis.
? Determination of the concentration of glucose (daily profile of blood sugar levels), lipids, triglycerides, cholesterol, proteins in blood serum.
? Blood culture for suspected bacterial embolus.
? ECG (atrial fibrillation), if necessary, monitoring for 24 hours to detect arrhythmia.
? Chest X-ray (heart failure).
? Auscultation and ultrasound of the carotid arteries (atherosclerotic plaques and stenosis) and ultrasound of the heart.
Differential diagnosis
: hypertensive and diabetic neuroretinopathy, vasculitis, anterior ischemic neuropathy. Indications for consultation with other specialists: therapeutic and neurological examination to identify sources of embolism and cardiac arrhythmias.
Treatment
? It is usually impossible to completely eliminate the occlusion.
? Despite the lack of effective methods for treating occlusion of the central nervous system leading to the restoration of visual functions, an urgent consultation with an ophthalmologist is required in order to prescribe emergency drug therapy. Immediate intervention improves the possibility of vision restoration, but only in 21-35% of cases. Although restoration of vision is the immediate goal of the treatment, one should be aware that POC in the CAS is a harbinger of other systemic diseases, the prevention of the further development of which requires serious attention.
Decrease in IOP level
? It is possible for the embolus to move through the artery in the peripheral direction from the main trunk to one of the branches of the CAS after massaging the eye and lowering the IOP level, as a result of which the area of retinal damage decreases. This method of treatment can be used if no more than 8 hours have passed since the loss of vision, so more often this treatment technique can be used by a therapist or neurologist who witnessed a sharp deterioration in the patient’s vision during this period of time. An increase in IOP during massage leads to a reflex expansion of the small ophthalmic arteries by 16%, and a sudden decrease in IOP after compression of the eyeball ceases increases the volume of blood flow by 86%, as a result of which the embolus moves further down the vessel. Eyeball massage technique
for acute obstruction of the central nervous system.
1.
The patient's head should lie low to avoid orthostatic relative deterioration of the retinal blood supply.
2.
Using your fingers, press through the closed upper eyelid onto the eyeball.
3.
The eyeball is pressed into the orbit, first weakly, then more forcefully, and after 3-5 s it is suddenly released.
4.
After a few seconds, the process is repeated.
5.
If necessary, the patient can massage the eyeball independently.
? IOP can be reduced with corneal paracentesis
if less than 24 hours have passed since the decrease in vision.
? To reduce ophthalmotonus, the hyperosmotic drug glycerol
orally at the rate of 1-2 g/kg of the patient’s body weight. The maximum decrease in IOP occurs after 1 hour, the duration of the effect lasts about 5 hours. During treatment, it is possible to repeat glycerol intake up to 5 times, taking into account contraindications (acute urinary retention, hypervolemia, diabetes, dehydration, severe pathology of the heart, kidneys, liver). Medicines are not used parenterally!
? IOP can also be reduced using epibulbar instillations of drugs (local β-blockers, brinzolamide), taking into account their contraindications.
? Diuretics (acetazolamide) for the purpose of dehydration and lowering IOP should be used with caution, keeping in mind the possible increase in blood viscosity.
? Vasodilators
? When establishing the fact of POC in the CAC, it is advisable to take 1 tablet of validol or nitroglycerin under the tongue.
? Vasodilators are prescribed (10 ml of 2.4% aminophylline solution IV for 10-15 days, 1 ml of 1% nicotinic acid solution IM or 2 ml IV drip for 7-10 days).
? Dextran solutions (or saline solution) with 5 ml of pentoxifylline and dexamethasone are injected intravenously.
? The use of carbogen helps cause dilation of small retinal arteries (5% carbon dioxide) and enrich ischemic retinal tissue with oxygen (95% oxygen in carbogen).
? For the same purpose, hyperbaric oxygenation is indicated if 2 to 12 hours have passed from the onset of signs of acute onset in the central nervous system.
? Improvement of rheological blood parameters.
? In the presence of other diseases of atherosclerotic origin, the patient can be prescribed acetylsalicylic acid (100-250 mg/day).
? Heparin 500 units with dexamethasone 0.5 ml or nadroparin calcium (fraxiparin) 0.3 ml is administered parabulbarly once a day for 5-7 days.
? 5% ethylmethylhydroxypyridine succinate IV drip 2 ml for 4 days, then IM 2 ml 4-6 days, then piracetam 400 mg + cinnarizine 25 mg 1-2 capsules 3 times a day for 1-1 ,5 months
? A radical (“aggressive”) method of probing the proximal ophthalmic artery through the femoral artery with the introduction of thrombolytic agents is also proposed. This method is effective only in the case of a blood clot (hemorrhagic embolus), and not a calcium or cholesterol embolus.
? It is advisable to prescribe magnetic therapy and electrical stimulation of the optic nerve
to reduce acidosis and intercellular edema by increasing blood pH and increasing the linear speed of blood flow.
Patient education.
Patients with hypertension, diabetes, rheumatism, who have suffered a myocardial infarction, suffering from heart valve defects and increased blood viscosity should monitor their vision by periodically alternating closing one or the other eye. If loss of vision is detected in an eye that previously had good vision, it is necessary to massage the eyeball according to the method described above as a means of self-help, and then seek help from an ophthalmologist.
Further management.
Patients who have undergone POC in the CAS and its branches must, under the control of a coagulogram, use antiplatelet agents (acetylsalicylic acid), antihypertensive and vasodilator drugs prescribed by a general practitioner.
Forecast
? Often, if the central circulation is obstructed, it is possible to restore blood circulation
, but ischemic edema persists, its reverse development proceeds very slowly, ending with atrophy of the retinal tissue and optic nerve. Subsequently, secondary emptying of the retinal vessels is observed.
? The mortality rate of patients who have suffered arterial occlusion of the retina over the next 9 years after the disease is 56% compared to 27% in the same age group who do not have a history of CAS.
? The life expectancy of patients after occlusive arterial pathology of the retina is 5.5 years (compared to 15.4 years in a similar age group without this pathology). The development of ANC in CAS is associated with smoking and cardiovascular diseases, as well as with increased neuropsychic stress.
? Both eyes have the same incidence of possible involvement, with bilateral disease occurring in 1-2% of cases.
Symptoms of thrombosis
With occlusion of the central nervous system, a person does not experience any pain or discomfort, but suddenly there is a profound deterioration in vision - up to its complete loss. In case of thrombosis or embolism of one of the local arterial branches, only a separate zone in the field of view (corresponding to the projection of the affected sector of the retina) may become “blind” - a “blind spot” or scotoma occurs.
In some cases, the patient feels a kind of “flickering”, emerging and receding blindness; such symptoms indicate spastic compression and reverse relaxation of the artery, which serves as a direct harbinger, again, of approaching thrombosis. With any symptoms of this (or similar) kind, the count may no longer be in hours, but in minutes, i.e. At any cost, specialized ophthalmological care should be provided as quickly as possible, as an emergency.
Symptoms of angiopathy
A serious problem is late diagnosis due to the absence of symptoms for a long time, while pathological changes in the eyes progress.
Often angiopathy is determined already when complications have formed.
Symptoms that may indicate retinal angiopathy:
- headache;
- episodes of blurred vision;
- pain in the eye area;
- decreased visual acuity;
- peripheral vision impairment.
The listed symptoms are a reason for an urgent visit to an ophthalmologist.
Treatment of occlusion of the central nervous system
The chances of restoring blood circulation and saving the retina from necrosis/infarction are determined by how quickly help is provided. Inpatient placement is required. Standard medical response regimens include vasodilators, antihypertensives, anti-inflammatory drugs, diuretics (diuretics), and anticoagulants (drugs that reduce blood clotting). Blood pressure, blood composition (primarily coagulation factors), as well as the clinical picture of concomitant systemic diseases, if any, should be constantly monitored.
Even if a vascular accident in the central retinal artery basin is experienced more or less well, in the future a comprehensive examination will be required (to diagnose and clarify the causes of the incident), treatment and intensive prevention of exacerbations of the underlying pathology, as well as regular ophthalmological monitoring and strict adherence to all recommendations.
Content:
- 1 Arterial occlusion
- 2 Retinal vein thrombosis
Description
Acute circulatory disorders (ACI) in the retina
are urgent conditions based on spasm, thrombosis or embolism of the main vessel or its branches. ONK are among the most severe forms of eye pathology, leading to partial, and in some cases, complete loss of vision.
ICD-10
H34.0 Transient retinal arterial occlusion. H34.1 Central retinal arterial occlusion. H34.2 Other retinal arterial occlusions. H34.8 Other retinal vascular occlusions. H34.9 Retinal vascular occlusion, unspecified. H40.5 Glaucoma secondary to other eye diseases.
Abbreviations: AC - acute circulatory disorder, CAR - central retinal artery, CVR - central retinal vein, ERG - electroretinogram.
Purpose of the recommendations
: timely diagnosis and rational therapy of the disease to preserve the patient’s health and quality of life by ensuring the possible preservation of visual functions.
Epidemiology
? In 91.2% of cases, PNCs in retinal vessels develop against the background of cardiovascular diseases
. The most common cause of obstruction of the CAS and CVS and their branches are hypertension and atherosclerosis (79%), as well as diabetes. Due to the annual increase in the incidence of the latter, there is a tendency to increase the incidence of vaso-occlusive diseases of the retina.
? Occlusion of the central nervous system is often associated with systemic diseases
requiring immediate treatment for life-saving reasons. The process is predominantly one-way. Occlusion of the main trunk of the CAS occurs in 57% of cases, its branches - in 38%, cilioretinal occlusions - 5%. In most cases, the age of patients is from 40 to 70 years. Men are more often affected.
? Occlusion of the central vascular system and its branches (as opposed to arterial obstruction) is mainly due to the thrombotic process
. The severity of the obstruction and the preservation of vision are determined by the degree of venous decompensation and the duration of the thrombotic process. In 67.2% of cases, thrombosis of the vascular arcades occurs. Most often (82.4%) the superior temporal branch of the central nervous system is affected.
Prevention
: prevention and treatment of hypertension, atherosclerosis, diabetes and other predisposing diseases (rheumatic carditis, temporal arteritis, etc.), prescription of disaggregation therapy when indicated can prevent the development of vaso-occlusive diseases of the retina.
Screening
: one should suspect POC in the vessels of the retina and conduct an examination of the organ of vision in case of a sharp and sudden decrease in vision without pain in patients with hypertension, severe atherosclerosis and diabetes, as well as in case of loss of vision against the background of a hypertensive crisis. The examination includes determination of visual acuity, perimetry, IOP measurement, biomicroscopy, ophthalmoscopy, fluorescein angiography and ERG.
Diagnostics
It is recommended to make preventive visits to an ophthalmologist at least once a year. Examination of the fundus is a simple, quick and painless procedure that allows the doctor to diagnose even the initial signs of angiopathy and begin treatment on time.
The Center for Vision Protection provides effective diagnosis of retinal angiopathy using modern equipment. If necessary, the doctor prescribes other studies, for example, duplex examination of the brachiocephalic vessels, ultrasound of the eyeballs, etc.
Treatment
Urgent therapeutic measures must be taken soon after the onset of symptoms. If you do not get emergency help within 1–2 hours, you will not be able to restore your vision.
The doctor must massage the eyeball to reanimate blood supply, drops are used to reduce intraocular pressure, diuretics are administered, and the cornea is punctured.
If arterioles (small arteries) are spasmed, then vasodilators and inhalations are used. When the lumen is closed by a blood clot, they resort to thrombus-dissolving drugs, as well as drugs that reduce blood clotting.
In all cases, it is advisable to use antioxidants and injections of vasodilators. At the same time, treatment is prescribed for the disease that caused the occlusion of the central nervous system.
The effectiveness of treatment measures directly depends on how quickly the patient responded to the symptoms and managed to seek professional help.
The ability to see can be preserved if doctors managed to carry out adequate therapeutic actions in the first hour. 1% of patients subsequently develop glaucoma, and the most common complication remains irreversible blindness.