Retina
- the thinnest multilayer structure of the eye, covering 70% of the area of the inner surface of the eyeball. The retina of the eye is connected to the visual analyzers of the brain, into which it transmits information and is responsible for converting light impulses into nerve impulses.
The inner side of the retina is adjacent to the vitreous body, and the outer side is adjacent to the choroid: the choroid from which it receives nutrients and oxygen. Sometimes, under the influence of one reason or another, part of the retina moves away from the choroid. In this case, cells deprived of nutrition and oxygen quickly die. Without surgical intervention, the process leads to disturbances up to complete loss of vision. This condition is called retinal detachment.
Retinal disinsertion
–
a severe pathological process requiring emergency surgical care, in which the reticular layer of the eyeball is separated from the vascular layer.
The term itself was first proposed at the beginning of the 8th century, but its clinical confirmation was made only in 1851 after the invention of the ophthalmoscope. According to research, the incidence of the disease has increased significantly over the past decade: previously, 1 in 15,000 people were at risk of retinal detachment, now it is 1 in 10,000. Patients with myopia and aphakia often suffer from retinal detachment, especially if part of the vitreous lens was removed during surgery simultaneously with the lens. bodies. In the latter case, the risk of developing pathology increases to 10%.
Causes of retinal detachment
The most common cause directly leading to detachment is a retinal tear. As long as the shell is intact and sealed, it remains motionless. If a gap appears on it, its edges begin to lag further and further behind the choroid. The more extensive the process, the more severe the consequences for the patient, and the more difficult it is for the doctor to restore the patient’s vision.
Among the main causes of the disease are:
- Congenital or acquired myopia (myopia): 40-50% of all cases.
With myopia, the size of the eye changes: this leads to tension in the tissues of the eye and, as a result, thinning of the retina, its fragility and vulnerability. The affected retina easily bursts, which leads to detachment. - Injuries to the organ of vision: 10-20% of all cases.
- Surgical interventions (for example, cataract removal - 30-40% of all cases). It happens that retinal detachment recurs in an eye that has already been operated on for this reason.
- Oncological diseases of the eyes.
- Inflammatory diseases of the retina, degenerative processes in it.
- Hemorrhages, retinopathy, and retinal dystrophy significantly increase the risk of detachment.
- Systemic diseases of the body (endocrinological, hematological, cardiological, vascular).
The risk of the disease increases with intense sports (especially if it is associated with impacts, jumping), as well as pregnancy and childbirth - due to strong tension in pushing. If one eye has already had an episode of retinal detachment, the likelihood of a recurrence in the other increases by 15%. Heredity also influences the possibility of developing the disease.
Causes of retinal dystrophy
The development of pathology can be triggered by many factors. Basically, dystrophy occurs:
- in old age, as a consequence of aging processes in the body
- by hereditary predisposition
- for hypertension, atherosclerosis and other vascular diseases
- as a complication of diabetes
- for vitamin deficiencies and poor nutrition
- if you are overweight
- from the harmful effects of smoking
- as a result of stress and nervous shock
- after a viral illness
- as a result of harmful effects of ultraviolet radiation
Up to 40% of different types of this retinal pathology are observed in myopic people. With farsightedness, dystrophy is observed only in 8% of cases, from 2 to 5% occur in people with normal vision. All causes of the disease can be classified into local and general. The first include:
- genetic predisposition;
- eye injury;
- myopia;
- inflammatory and infectious eye pathologies
Common reasons include:
- diabetes
- atherosclerosis, hypertension
- various types of intoxication
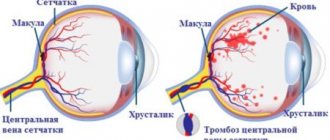
Types of retinal detachment
Depending on the reasons that caused the detachment and the nature of the lesions, rhegmatogenous, traction and exudative (serous) types of the disease are distinguished.
Rhegmatogenous retinal detachment (RRD)
Primary detachment associated with a rupture (from the Greek rhegma - rupture)
on the shell of the retina.
Medical statistics indicate that men are more likely to experience RRD, with the peak of the disease occurring at 65-69 years of age.
With RRD, the vitreous body begins to penetrate through the breaks formed in the retina, promoting increasingly severe detachment. The condition of the vitreous body loses its homogeneity with age, dividing into two fractions: thick and liquid, which explains the fact that the peak incidence occurs in old age.
Tractional retinal detachment (TRD)
Due to various pathological processes, adhesions can form between the retina and the vitreous body. Strands or formed vessels, when the position of the vitreous body changes, literally pull back and tear the retina away from the choroid. There is no retinal tear.
This type is associated with diseases such as diabetes, sickle cell anemia, retinopathy of prematurity, etc.
Exudative retinal detachment (ERD)
Exudative, or, as it is also called, serous retinal detachment also develops without breaks. With EOS, fluid accumulates in the lower parts of the subretinal space. With an increase in the volume of this interstitial fluid, the retina begins to lag behind the choroid.
The cause of the accumulation is a violation of vascular permeability. This indicator is affected by inflammatory and infectious diseases, genetic characteristics, oncology, complications of surgical interventions, systemic diseases, and kidney diseases.
The prognosis for any type of retinal detachment is associated with:
- how acutely the disease begins and how quickly the affected area increases;
- area and location of the detachment (if the central areas are affected, it will be more difficult to restore vision);
- speed of medical care.
Restrictions
People diagnosed with macular degeneration will have to:
- regularly carry out self-monitoring of vision using an Amsler grid;
- wear sunglasses;
- read books in a room well lit with halogen lamps;
- stop smoking;
- provide physical activity;
- take antioxidants and multivitamins.
Although it is impossible to completely restore vision with macular degeneration, treatment will prevent further tissue degradation, avoid blindness and disability, and maintain ability to work.
Symptoms of retinal detachment
The main symptoms indicating retinal detachment are:
- the appearance of a veil, flies, floating spots before the eyes. The veil is not eliminated when using eye drops; “foreign objects” cannot be removed;
- blurred vision, decreased sharpness;
- “curtain” effect: peripheral vision suddenly disappears, as if part of the field is covered with a gray curtain. The situation improves in the morning: it seems to the patient that the area hidden behind the “curtain” has become smaller. By evening, the viewing area decreases again;
- flashes in the form of lightning or sparks;
- distortion of the objects in question.
Causes and symptoms
With macular degeneration, retinal vessels degenerate (their diameter decreases) and their destruction. As a result, macular cells do not receive enough nutrients and oxygen, which is why degenerative processes begin to occur in them.
Various factors can provoke the development of degenerative processes:
- hereditary predisposition;
- genetic diseases;
- age-related changes;
- ultraviolet exposure;
- unbalanced diet leading to vitamin deficiency;
- abuse of fatty foods containing cholesterol;
- excess weight;
- diabetes;
- cardiovascular diseases (atherosclerosis, hypotension, hypertension);
- cataract surgery;
- smoking (increases the risk of dystrophy by 5 times).
Elderly people are especially susceptible to macular degeneration, as they are often diagnosed with problems in the functioning of the circulatory system. The disease is diagnosed more often in women than in men.
Main symptoms of the disease:
- deterioration of visual acuity;
- loss of clarity of perception;
- difficulty orienting in the dark;
- difficulty reading text;
- difficulty recognizing the faces of others;
- blurred vision;
- the appearance of a dark spot in front of the eyes that does not have distinct contours, which makes it impossible to read, drive, or do work that requires fine motor skills;
- distortion of outlines;
- visual bending of straight lines, their discontinuity;
- deformation of letters and numbers;
- inability to determine the distance to an object;
- increased photosensitivity.
As a result, a person has serious problems in everyday life: when doing minor work, driving a car, crossing the road, counting money. He loses his independence, which often provokes the development of depression and mental problems.
There is no pain syndrome with macular degeneration.
Diagnosis and treatment of retinal detachment
If one or more symptoms appear, immediately consult a specialist: this will allow you to diagnose retinal detachment and begin treatment at an early stage.
To diagnose the disease, the doctor will check:
- visual acuity;
- fields of view;
- intraocular pressure.
In addition, the fundus of the eye will be examined and examined using an ophthalmoscope - a slit lamp.
Slit lamp
The ophthalmologist may also prescribe additional studies: ultrasound, electrophysiological (cardiogram of the eye), X-ray, tomography, MRI.
The disease cannot be corrected with drops, ointments or tablets.
Treatment of retinal detachments is surgical. During the operation, the detached part is returned to its place, the breaks are blocked, and, if necessary, the cords connecting the retina with the vitreous body are removed. The retina, returned to its previous position, is strengthened with fillings or a laser. If the outcome is successful, significant improvements will occur immediately, and vision will be restored within another 3 months. However, you may not be able to get rid of some of the consequences of retinal detachment - especially its advanced forms: blurry spots, blurriness and blurriness may remain forever.
Types of macular degeneration
Macular degeneration of the retina can manifest itself in two forms: dry (occurs in 90% of cases) and wet. In 10-20% of patients, the dry form turns into a wet one.
In the dry form, the retinal tissue becomes thinner and extracellular deposits (drusen) of yellow pigment appear in its layers.
In the wet form, new blood vessels form and grow into the space between the pigment epithelium and the retina. They are very fragile, which is why they are often damaged, leading to swelling and hemorrhage. In addition, such vessels cause the death of light-sensitive cells.
Prevention of retinal detachment
To prevent retinal detachment, you can use all the recommendations that accompany a healthy lifestyle. Give up bad habits, eat a variety of foods rich in vitamins, follow the rules of eye hygiene, protect them from external influences - bright sunlight, shocks, and injuries at work.
Monitor the general condition of the body: control blood pressure and blood sugar levels. And, of course, do not forget about regular – at least once a year – visits to the ophthalmologist.
Treatment with MACDEL devices
For macular degeneration of the retina, treatment is aimed at stopping the formation of new vessels, which helps slow down further progression of the disease and prevent loss of vision. An effective result is provided by taking antioxidants in combination using the MAKDEL-08 device, made on the basis of a helium-neon laser. Retinal tissue is stimulated by low radiation energy, due to which there is no visible destruction and the antioxidant activity of cells increases.
In addition, under the influence of laser beams, a speckle structure is formed, which the patient perceives as chaotically moving “grain”. Looking at it has a beneficial effect on the eyes, reduces tension, and improves nutrition of the retina.
What should you not do during the recovery period after surgery?
After surgery to restore the integrity of the retina, the patient wears a bandage on the operated eye for the first day. If pain occurs, you can take painkillers - a specific drug, the regimen of which will be recommended by your doctor. The next day, the bandage can be removed and the eyelids (not the eye itself!) treated with a solution of chloramphenicol or furatsilin.
What not to do during the recovery period:
- overexert yourself, engage in any kind of sports, lift weights;
- expose the eye to any radiation (especially ultraviolet radiation) and heat - it is advisable to refrain even from cooking food on the stove yourself;
- make sudden movements of the head, bend over;
- rub the eye or subject it to any other mechanical stress.
It is highly undesirable to use decorative cosmetics for two months after surgery. Particular care must be taken when washing and performing other hygiene procedures: water, soap and other products should not get into the eye. To do this, you can cover it with a sterile napkin secured with an adhesive tape.
In addition, you should be especially careful about your general health: even a minor cold accompanied by an increase in temperature can lead to a deterioration in the condition of the retina.