TRACHOMA
(Greek trachys rough, uneven + -oma; synonym:
conjunctivitis trachomatosa, s. granulosa, ophthalmia bellica, s. militaris
) - a chronic infectious eye disease caused by chlamydia trachoma, characterized by damage to the cornea and conjunctiva with the formation of follicles (trachomatous grains) , and in the late stage - scarring of the conjunctiva and cartilage of the eyelids.
Trachoma has been known since ancient times. In the Ebers papyrus, dating back to approximately the 17th - 16th centuries. BC e., contains a description of an eye disease that affected the population of Africa and Asia, in which discharge from the eyes, granulation, loss of eyelashes, entropion of the eyelids, scarring and clouding of the cornea were observed. The term “trachoma” first appears in the writings of the Sicilian physician Dioscorides (1st century AD). K. Galen introduced the term “trachochmatous” and described four stages of the disease. The appearance of T. in Europe is associated with Napoleon’s campaign in Egypt in 1798, after which an epidemic of eye disease arose, then called Egyptian (oriental, military, granular) ophthalmia.
Nowadays, Trachoma is widespread in developing countries of Southeast Asia and Africa. According to WHO (1981), trachoma affects St. 500 million people, of which approximately 2 million had this disease as the cause of complete blindness.
In Tsarist Russia, Trachoma was widespread and was the main cause of blindness. The high incidence of T. was largely due to the extremely low level of medical care and unfavorable social and living factors. After the Great October Socialist Revolution, a systematic fight against T. began. The resolution of the All-Russian Central Committee of the K and the Council of People's Commissars of the RSFSR dated November 28, 1927 determined the main directions in carrying out health-improving activities: organizing a network of special treatment-prof. institutions in trachoma-prone areas (nursing and medical trachomatosis stations, trachomatosis dispensaries, training of specialists, identification of patients and mandatory treatment). On the territory of the USSR, thanks to the preventive measures taken and the development of specialized types of assistance, it was possible to achieve the elimination of trachoma as a mass disease; Only sporadic cases occur. Among newly identified patients, up to 80-90% are people with relapses of trachoma.
The causative agent of T. was discovered in 1907 by S. Provacek and L. Halberstadter and classified by them into the group of trachoma chlamydia - Chlamydia trachomatis (see Chlamydia).
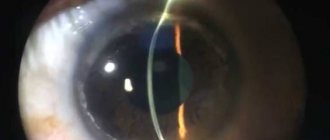
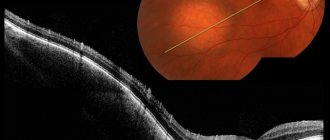
Rice. 1. Cytological preparation of conjunctival scraping for trachoma: the Provacek-Halberstaedter body is tightly adjacent to the nucleus of the epithelial cell (indicated by the arrow); Romanovsky-Giemsa staining; X 900. Fig. 2. Appearance of the eye with trachoma stage II: germination of blood vessels into the cornea in the area of the upper part of the limbus (trachomatous pannus). Rice. 3. The inner surface of the upper and lower eyelids with stage III trachoma: areas of infiltration and follicles (1) in the conjunctiva alternate with tender rubies (2). Rice. 4. Inner surface of the upper eyelid with stage IV trachoma: widespread whitish areas of scar tissue in the conjunctiva; dark brown spots on the conjunctiva—hemorrhages.
The causative agent of T. is found in the cytoplasm of conjunctival epithelial cells in the form of inclusions - Provacek-Halberstadter bodies (printing Fig. 1).
The onset of the disease is associated with the damaging effect of the pathogen on the epithelial cells of the conjunctiva and cornea; then the inflammatory process spreads to the deeper tissues of the conjunctiva and affects the cartilage of the eyelids. Active forms of the disease are more often observed at the age of 4-10 years, the consequences of T. - trichiasis (see Eyelids) and entropion (see) - at the age of over 50 years. Women get sick 3 times more often than men.
Tuberculosis and other hron. diseases, helminthic infestations, and nutritional dystrophy aggravate the course of T. Entropion of the eyelids, trichiasis, damage to the lacrimal ducts, as well as seasonal epidemics of bacterial and viral conjunctivitis contribute to relapses of T.
Epidemiology
Trachoma is an endemic disease. The living conditions of the population and their level of dignity play an important role in the spread of T. culture. The infectious agent is transmitted directly or indirectly (through hands, clothing, towels).
The main sources of infection in T.'s foci are patients with active forms of the disease. A significant role in the transmission of infection also belongs to patients with erased forms of T., with relapses of the disease, as well as carriers of the infectious agent, persons with unusual localization (for example, in the lacrimal ducts) and an atypical course of the process.
Pathological anatomy
The main morphol. manifestation of Trachoma is hron. inflammation of the conjunctiva with proliferation and hyperplasia of adenoid tissue, culminating in the development of scar changes. Trachoma is characterized by the simultaneous presence of signs of inflammation, proliferation of connective tissue and epithelium, and degenerative phenomena.
In the initial period of T., diffuse infiltration of neutrophilic leukocytes and histiocytes is determined in the conjunctiva. Starting from the 10-12th day of the disease, lymphocytic and plasma cell infiltration develops. Subsequently, a large number of young undifferentiated cell forms appear with the presence of numerous mitotic figures; in severe cases - a large number of lymphoblasts, plasma cells and basophils.
In addition to diffuse infiltration, T. is characterized by the formation of follicles, which initially represent focal accumulations of lymphocytes (immature follicles). In a mature follicle, there is a peripheral zone consisting of lymphocytes and a lighter central zone (reproduction center), which includes epithelioid cells, lymphoblasts, histiocytes, and phagocytes.
The trachomatous process is marked by early onset dystrophic changes and necrosis of conjunctival tissue, primarily in the area of the follicles. The stroma of the follicles undergoes sclerosis and hyalinosis, but their resorption is possible without scar formation. Around the follicles, fibrous tissue develops, forming a capsule, in which cellular infiltrates and the causative agent of infection can remain “walled up” for many years.
In patients with severe disease, diffuse infiltrative processes in the conjunctiva and edema predominate, thickening of the conjunctiva with an increase in the size of the follicles and their noticeable prolongation is noted - the papillary form of trachoma.
In the cornea, diffuse inflammation of varying intensity is noted with penetration of newly formed vessels and infiltration into the area of the upper part of the limbus (color Fig. 2) and the formation of trachomatous pannus (see). In severe cases, follicles appear in the stroma (intrinsic substance) of the cornea (see). In the lacrimal organs (see), inflammation with lymphoid-plasma cell infiltration and scarring is observed. In severe cases, infiltration extends into the deep layers of the eyelid cartilage. In the meibomian glands, the development of cysts, vacuolization, fatty degeneration, hyalinosis, and amyloidosis of cartilage are observed.
Diagnostics
The diagnosis is made based on the patient's complaints and instrumental examination of the eye. Upon examination, changes in the structure of the visual organs are revealed: characteristic follicles and papillae are formed. Depending on the stage of the disease, the follicles may be in the stage of formation, proliferation, connection or scarring.
Most often, the doctor performs an examination using a binocular loupe. A slit lamp examination may be necessary. The doctor determines whether visual functions are impaired and how much the patient’s vision has decreased (if the results of previous examinations are available). The ophthalmologist prescribes the following laboratory tests:
- cytological examination of scrapings from the conjunctiva;
- study of the composition of follicles;
- determining the presence of antibodies in the blood;
- bacterial culture of discharge;
- biomicroscopy of the eye;
- pathogen identification based on DNA analysis.
The most accurate diagnosis is provided by microscopy of smears from the inflamed conjunctiva, as well as identification of intracellular inclusions (Provacek-Halberstadter bodies).
If there are systemic diseases, the patient is referred for consultation to other specialists. Based on the test results, the patient is prescribed treatment.
Clinical picture
The incubation period is 7-14 days. Both eyes are usually affected. The onset of the disease may be invisible, without subjective sensations. Sometimes there is a slight mucopurulent discharge, a sensation of a foreign body and a burning sensation in the eyes.
An acute onset of the disease is also possible. In this case, symptoms of acute conjunctivitis (see), reminiscent of conjunctivitis with inclusions, are observed; there is hyperemia of the skin of the eyelids, photophobia, and copious mucopurulent discharge; the conjunctiva is swollen and hyperemic.
In approximately 25% of cases, erased forms occur, in which the symptoms are scanty, and the disease is often diagnosed as chronic. conjunctivitis.
In the wedge, picture of T., according to the classification of V.V. Chirkovsky (1935) and McCallen (AF Mac Callan, 1936), four stages are distinguished. Stage I (initial T.) - the development of inflammatory phenomena in the conjunctiva, the appearance of immature and single mature follicles (trachomatous grains) on the upper eyelid and in the transitional folds with edema and vascularization of the upper part of the limbus, with superficial subepithelial infiltration of the cornea. Stage II (active Trachoma) - further development of follicles, their papillary hyperplasia in the area of transitional folds and cartilage, formation of pannus and infiltrates in the cornea; the appearance of individual scars as a result of follicle necrosis. Stage III (scarring T.) - the predominance of processes of scarring of the conjunctiva of the eyelids, transitional folds with persistent phenomena of inflammation (tsvetn. Fig. 3), characteristic of stages I and II. Stage IV (scar T.) - clinically cured T.: follicles and infiltrates are completely replaced by scar tissue (tsvetn. Fig. 4).
Depending on the predominance of certain pathol. elements in the active period (stages I - III) Trachomas distinguish four forms of the disease: follicular, in which predominantly follicles are observed; papillary, with a predominance of papillary growths; mixed, when both follicles and papillary growths are detected; infiltrative, characterized by predominant infiltration of the conjunctiva and cartilage of the eyelids.
When infected in early childhood, the wedge, T.'s picture resembles blenorrhea of newborns (see Blennorrhea); with repeated exacerbations, these patients develop cicatricial changes in the cornea characteristic of T., detected by biomicroscopy (see Biomicroscopy of the eye).
The most severe complication of T. is a trachomatous corneal ulcer, the appearance of which is promoted by a secondary bacterial infection. A corneal ulcer may be accompanied by hypopyon (see), perforation, endophthalmitis (see), panophthalmitis (see). T.'s complications also include acute and chronic. conjunctivitis that develops as a result of a bacterial or viral infection. With T., diseases of the lacrimal organs (see) are often observed (up to 10% of cases) - dacryoadenitis, dacryocystitis, canaliculitis, caused by the pathogen T. in combination with a secondary infection.
The consequences of T. are due to the process of scarring. The development of scar tissue in the area of transitional folds of the conjunctiva leads to the appearance of adhesions between the conjunctiva of the eyelid and the eyeball; in this case, the conjunctival fornix shortens or disappears completely (spmblepharon). Changes in the cartilage of the upper eyelid with T. lead to inversion of the eyelids (see), abnormal growth of eyelashes (trichnaz). As a consequence of T., drooping of the upper eyelid develops (see Ptosis), giving the face a peculiar sleepy expression. As a result of cicatricial changes in the lacrimal gland, lacrimation decreases and drying of the conjunctiva and cornea occurs - xerosis (see Xerophthalmia). Severe scarring of the conjunctiva in combination with trichiasis and entropion leads to decreased vision, and scarring and clouding of the cornea leads to partial or complete loss of vision.
Stages of trachoma
The main stages of trachoma, which experts identify, are as follows:
- The first stage
is characterized by inflammation of the mucous area. The eyelids begin to swell and an infiltrate forms, so the eyelashes may stick together and fall out. The patient may experience a feeling of sand in the eyes. In addition, light can cause an unpleasant feeling. Single occurrences of follicles are possible, which in appearance will resemble millet grains. - At the second stage
of trachoma development, a person is most dangerous to the environment, as the disease becomes very contagious. The patient suffers from profuse lacrimation syndrome. The number of follicles increases sharply, and they begin to look like frog eggs. Moreover, their condition is not stable; on the contrary, they can merge with each other, causing severe swelling. Some follicles may undergo the process of decay, leaving scar tissue. At this stage, the course of the disease affects the cornea of the eye, which can cause a decrease in the quality of vision. - The third stage
is characterized by active tissue scarring. New follicles still continue to disturb the patient, but their number is significantly reduced. The inflammation process subsides, the follicles dry out and leave scars. They are clearly visible upon closer inspection, as they are white. An increase in the amount of scar tissue leads to deformation of the eyelid. As a rule, the area of the upper eyelid falls under the greatest negative impact. Moreover, the ciliary edge can turn inward, causing damage to the cornea. - At the last stage
, the inflammation that tormented the patient goes away, and the source of infection fades away. From a clinical point of view, the person will be considered healthy. However, at this stage the negative consequences of the disease must be addressed. The cornea has a cloudy appearance, and the patency of the tear duct is reduced. Upper eyelid tissue that has undergone the scarring process can cover almost the entire eye. At this stage, complete loss of vision may occur. The tissue covering the eye can only be removed through surgery.
The given stages describe the disease process without timely treatment. The last stages of the development of trachoma can lead to loss of vision, completely or partially. Therefore, seeing a doctor at the first unpleasant symptoms can save the patient’s vision.
Diagnosis
Wedge, T.'s diagnosis is based on the results of a study of the conjunctiva and cornea. To make a diagnosis, at least 2 of the 4 following signs must be present: follicles on the conjunctiva of the upper eyelid; follicles in the area of the upper limbus or their consequences; typical conjunctival scars; pannus, more pronounced in the upper part of the limbus. In endemic foci, the presence of one of these signs is sufficient.
The main methods of laboratory diagnosis include: 1) cytological examination (see) of scrapings from the conjunctiva (cytoscopy) and at the same time for the presence of Provacek-Halberstadter bodies in epithelial cells; 2) detection of trachoma antigen by the method of fluorescent antibodies (see Immunofluorescence) in the epithelial cells of scrapings from the conjunctiva; 3) isolation of T. chlamydia from the conjunctiva by cultivation in the yolk sac of chicken embryos or in tissue culture (see Cultivation of viruses); 4) determination of specific antibodies (see) in blood serum.
Differential diagnosis is carried out with other follicular conjunctivitis. Moreover, in the initial stages of T., the main differential diagnostic feature is the presence of Provacek-Halberstadter inclusions in the epithelial cells of the conjunctiva and the formation of pannus in the upper segment of the cornea. Differential diagnosis with paratrachoma (conjunctivitis with inclusions, blenorrhea with inclusions), caused by a pathogen of the same group, presents significant difficulties due to the similarity of the wedge, the picture, as well as the fact that with paratrachoma, as with T., in the epithelial cells of the conjunctiva detect Provacek-Halberstaedter inclusions. The most important sign of paratrachoma is the predominant involvement of one eye, adenopathy; in addition, differentiation is carried out according to the location and shape of the follicles, the presence of papillary growths, and the nature of the corneal lesion (see Conjunctivitis, table). Stage IV trachoma must be differentiated from the consequences of burns of the conjunctiva and cornea, as well as diseases accompanied by the formation of scars in the conjunctiva: conjunctival pemphigus (see Conjunctiva), diphtheria (see), Sjögren's dry keratoconjunctivitis (see Sjögren's syndrome), molluscum contagiosum (see Molluscum contagiosum), etc.
Causes of trachoma
Trachoma of the eye is caused by the bacteria Chlamydia Trachomatis. These bacteria are essentially intracellular parasites. The initial symptoms are often consistent with the symptoms of conjunctivitis, although the causative agent is bacteria. The parasite inhabits the cells of the human body, reacting like a virus.
The cause of trachoma may be infection with chlamydia from an already infected person. Often the disease begins to develop due to touching the face and area around the eyes with dirty hands. In this case, a person becomes self-infected. Infection can also occur as a result of using common items intended for personal hygiene. For example, through a dirty towel that is publicly available. In addition, trachoma is often spread by insects; even ordinary flies are dangerous.
Treatment
Methods of drug treatment for T. were developed in the USSR under the leadership of M. P. Chumakov. Specific etiotropic treatment is carried out with antibiotics (see) and sulfonamides (see Sulfonamides). The most effective are tetracycline antibiotics (see Tetracyclines).
Antibiotics are used in the form of 1% ointments, which are placed in the conjunctival sac 3-6 times a day. In the next 6 months. ointment applications are reduced to 1 time per day (anti-relapse treatment); carry out dispensary observation. In countries with an underdeveloped healthcare system, according to WHO recommendations (1981), intermittent treatment is carried out: applications of tetracycline ophthalmic ointment or long-acting preparations (dibiomycin and ditetracycline ophthalmic ointments) 2 times a day for 5 days, or 1 time a day for 10 days every month; Duration of treatment - 6 months. In severe forms of the disease, local use of tetracycline in the form of 1% ointment is combined with oral administration of 250,000 units 4 times a day for 3-4 weeks. In addition, sulfapyridazine sodium is prescribed (on the first day 1-2 g, in the next 9 days 0.5 g) or doxycycline once a day for 3-4 weeks. Since 1966, interferon preparations have also been used to treat T. (see Interferon inducers, Interferon), mainly in cases of intolerance to antibiotics and sulfonamides. According to indications, during treatment, non-traumatic expression of the follicles is performed - squeezing out with special tweezers, carried out under local anesthesia in compliance with the rules of asepsis and antisepsis.
For severe scarring, repeated multiple diathermocoagulation (see) of focal infiltrates is used. Localized trichiasis is eliminated by careful epilation of eyelashes, as well as by electrolysis (destruction of hair follicles by introducing electrodes) or cryosurgery (see). For trichiasis in combination with entropion (entropion of the eyelids), plastic surgery of the anterior plate of the eyelid is used (see Blepharoplasty). Using the Snellen operation, the cartilage is straightened by removing a prismatic piece from its convex surface and bringing the edges of the semilunar groove together with ligatures. Plastic surgery of the eyelid margins is performed using various grafts, mucous membrane from the lip (Sapezhko operation), catgut, and preserved umbilical cord. For severe pannus, peritomy (dissection of the conjunctiva of the eyeball around the limbus) and periectomy (cutting a strip of conjunctiva up to 2-3 mm wide around the upper part of the limbus with scraping of the episcleral plate) are proposed, which leads to scarring and reverse development of the pannus. In case of severe xerosis, the eyelids are sutured, leaving a small space in the pupil area unsewn, a mucous membrane is transplanted and an operation is performed to move the Stenon's duct (parotid duct, T.) into the conjunctival sac (see Xerophthalmia).
Complications
In the absence of timely and adequate treatment, serious complications may develop. These include:
- dry eye syndrome;
- formation of a cloudy film on the cornea;
- scarring of the mucous membrane;
- entropion of the eyelid;
- trichiasis – abnormal direction of eyelash growth;
- dacryoadenitis - inflammation of the lacrimal gland;
- dacryocystitis - damage to the lacrimal sac;
- canaliculitis - inflammatory processes in the lacrimal tubules;
- iridocyclitis is an eye disease that affects the iris and ciliary body;
- complete loss of vision.
The latter complications arise as a result of the addition of a secondary bacterial infection. The most serious complication (purulent corneal ulcer) can lead to its perforation and a sharp decrease in vision, including loss of vision. The cornea may dry out as a result of the death of the conjunctival glands.
Some types of complications can only be treated with surgical methods. Cryosurgery allows you to remove abnormally growing eyelashes. If the eyelids are turned up, plastic surgery is indicated.
Given the serious complications, it is necessary to visit a doctor at the first signs of illness. Especially if you have recently visited countries with an unfavorable epidemiological situation for this disease (South-East Asia, Africa).
Prognosis and Prevention
The prognosis for timely treatment is favorable. Up to 80% of patients are cured within 2-3 months. Relapses are possible after 5-20 years or more in stage IV of the disease. With insufficient treatment, a complicated course, as well as untimely use of surgical methods of treatment, T. leads to loss of vision.
Prevention. In the USSR, a system of organizational, therapeutic and preventive measures was created that ensured the elimination of T. as a mass disease. In the regions where T. is distributed, a wide network of trachomatous dispensaries was organized (district, city, regional, republican). They represent the doctor-prof. institutions, the structure of which includes an outpatient clinic, inpatient departments, diagnostic laboratories, and an organizational department. Dispensaries provide treatment for patients with active forms of T., diagnosis and treatment of erased forms of the disease and relapses, as well as conjunctivitis caused by chlamydia, viral and bacterial conjunctivitis. In the surgical departments of the dispensary, operations are performed for the consequences of T. The trachomatous dispensary carries out long-term observation of family foci and persons with stage IV T., mass examinations of the population, selective control examination of persons who have recovered from T., regular examinations of children and pre-conscripts in areas where the disease is spreading with in order to identify patients with T. If necessary, mobile outpatient clinics and temporary hospitals are created, equipped with laboratory equipment necessary for conducting qualified mass epidemiol. examination, diagnosis and treatment of patients. The dispensary organizes personnel training - training of doctors and paramedics, conducts extensive health education, work among the population, monitoring compliance with hygiene regulations. requirements in family centers of T. During the period of a sharp decline in incidence in the zones where T. trachomatous dispensaries are widespread, without weakening the work on the prevention of T., they take part in the provision of ophthalmic. assistance to the population regarding other eye diseases.
Bibliography:
Antibiotic therapy of trachoma, ed. M. P. Chumakova and A. S. Savvaitova, M., 1955; Dawson C. R., John B. R. and Tarizzo M. L. Guide to trachoma control, trans. from English, M., 1983; Zaitseva N. S. Trakhoma, M., 1976; M a i ch u k Yu. F. Antibiotics in ophthalmology, p. 173, M., 1973; aka, Viral eye diseases, M., 1981; Maslova I.P. Study of the epithelium of the conjunctiva of the eyelids in trachoma using an electron microscope, Vestn. ophthalm., No. z, p. 17, 1963; Multi-volume guide to eye diseases, ed. V. N. Arkhangelsky, vol. 2, book. 1, p. 77 and others, M., 1960; Guide to eye surgery, ed. M. L. Krasnova, p. 38, M., 1976; Guide to trachoma, ed. G. X. Kudoyarova and others, parts 1-3, Ufa, 1970; With and in in and and t about in A. S. Treatment and prevention of trachoma, M., 1955; Ch and r to about in with to and y V. V. Trakhoma, L., 1953; Sh a t k i n A. A. Trakhoma, L., 1 965; A o u with hi with he M. Pathologie oculaire en Afrique du Nord, Rev. int. Trachome, t. 55, p. 97, 1978; Daghfous T. Trachoma, ibid., t. 53, p. 9, 59, 1976; D a o X and an Tra et Vu C ong Long, La liquidation de l'entropion-trichiasis et de ]a cataracte dans la lutte contre la cecite au Viet-nam, ibid., t. 56, p. 65, 1979; D ar o ugar S. ao Topical therapy of hyperendemic trachoma with rifampicin, oxytetracyclme, or spiramycin eye ointments, Brit. J. Ophthal., v. 64, p. 37, 1980; Diallo JS a. Cornand GA Post trachomatous degeneration, Rev. int. Trachome, t. 55, p. 5, 1978; Field methods for the control of trachoma, ed. by M. L. Ta-rizzo, Geneva, 1973; Ghione M., Werner GH et Cerulli L. Problemes immunologiques du trachome, Rev. int. Trachome, t. 51, p. 3, 1974; Mac Callan AF Trachoma, L., 1936; Schachter J. Complement-fixing antibodies to bedsonia in Reiter's syndrome, TRIC agent infection, and control groups, Amer. J. Ophthal., v. 71, p. 857, 1971; Treharne JD ao Antichlamydial antibody in tears and sera, and serotypes of Chlamydia trachomatis isolated from schoolchildren in Southern Tunisia, Brit. J. Ophthal., v. 62, p. 509, 1978; V 6r in P. Trachome et conjoncti-vite a inclusions similitudes et differences. Rev. int. Trachome, t. 57, p. 30, 1980.
N. S. Zaitseva.
Content
- 1 Signs and symptoms
- 2 Reason
- 3 Diagnosis 3.1 McCallan classification
- 3.2 WHO classification
- 4.1 Environmental measures
- 5.1 Antibiotics
- 7.1 Remedy
- 8.1 Etymology