According to the World Health Organization, cataracts are one of the most common diseases in the world among older people, leading to decreased visual acuity.
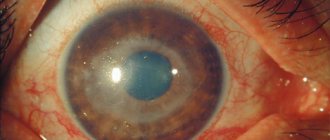
Cataracts are an ophthalmological disease characterized by clouding of the natural lens of the eye, which leads to blurred vision. With age, the lens loses its functions and begins to become cloudy. Opacities can be complete or partial. The retina of the eye converts the light that is formed in the lens, and we see a clear image. When the lens becomes cloudy, its transmission power decreases and the clarity of penetration of light rays decreases, as a result, vision deteriorates.
Causes of cataracts
Lens clouding can occur at any age. And it develops most often due to the natural characteristics of the body. Age-related changes become noticeable at the age of 40; by the age of 60, the vision of almost all people becomes blurred. There is no exact reason for the change in the lens, but there are a number of factors that influence the development of the pathology:
- Poor nutrition;
- Smoking;
- Health problems associated with metabolic disorders in the body (for example, diabetes);
- Alcohol consumption;
- Injuries or inflammatory diseases of the eyes;
- Long-term use of medications (glucocorticosteroids, etc.);
- Patient's age;
- Hereditary factor (history of cataracts)
What is immature cataract
As cataracts develop, they go through several stages with individual durations. Among them are the following forms of the disease:
- Initial. The lens loses transparency, while the patient's visual acuity remains at the same level. It is not for nothing that ophthalmologists call the disease insidious; it is very easy to skip the first stage, at which you can help a person using non-surgical methods (conservative treatment).
- Immature cataract. Symptoms of visual impairment appear sharply, but when examined using diagnostic equipment, the details of the fundus are still clearly visible.
- Mature. The structure of the fundus is not determined at all, visual acuity decreases. The patient can only see the top one or two lines of the vision test chart.
- Overripe. Pathological changes provoke compaction of the lens nucleus. The surrounding objects are as if in a thick fog, the patient sees only their blurry outlines. The process of clouding continues to progress, the final point of this stage is absolute blindness.
Thus, immature cataract of the eye is a certain stage in the development of the disease, accompanied by the appearance of the first symptoms. Lens clouding is often called the senile or senile form of the disease.
It is classified depending on where the primary changes are localized. If the opacification begins in the capsule, it is a cortical cataract. The nuclear form is characterized by damage to the nucleus of the lens.
Symptoms
Typically, patients with cataracts experience gradual blurring of vision. Due to the reduced capacity of the lens, objects around become foggy and blurry. The symptoms of the disease are as follows:
- The appearance of transparent spots in the field of vision;
- Blurred and unclear images of objects;
- Formation of corollas when light enters the eyes;
- Decreased night vision;
- Blurry images of objects – a person notices “fog” or “veil” before the eye
- Color vision disorders;
- Difficulty when working with small objects;
- The need to turn on bright light, especially when reading;
- Double vision when looking at various objects.
Specialists from the ophthalmology department of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency recommend visiting an ophthalmologist at least once a year.
If you experience these symptoms, we recommend making an appointment with an ophthalmologist. Early diagnosis will prevent negative consequences for your health. Phone for registration: 8 (499) 725-44-40
Diagnostics
To diagnose cataracts, it is necessary to conduct a complete ophthalmological examination, including:
- Visiting an ophthalmologist;
- Visometry (assessment of visual acuity using a special ophthalmological table);
- Ophthalmoscopy (examination of the fundus of the eye using ophthalmic instruments);
- Tonometry (measurement of intraocular pressure);
- Biomicroscopy (examination of eye structures using a slit lamp);
- Autorefractometry;
- Ultrasound examination of the eye.
Based on the diagnostic results, doctors at the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency will be able to determine the degree of development of the pathology and prescribe the necessary treatment.
Operation stages
Phacoemulsification involves the following steps:
- The ophthalmic surgeon performs a small puncture measuring 1-2 mm using a diamond instrument.
- Viscoelastic is injected into the ocular chamber, a substance that helps protect the ocular structures from mechanical and ultrasonic damage. Viscoelastic allows the specialist to freely perform all required manipulations.
- Through the puncture, the surgeon inserts a probe that crushes the lens with ultrasound, after which the emulsion is pumped out.
- Through the same puncture, a flexible intraocular lens is inserted into the place of the removed lens. Once placed inside, the lens unfolds and securely fastens.
- The viscoelastic substance is removed from the eye chamber (washing with an irrigating solution is used for this purpose).
Prevention
When the disease has just arisen and has not yet entered the stage of active development, as a rule, drug therapy is used for treatment. However, the patient must be regularly observed by an ophthalmologist to monitor and, if necessary, correct the selected treatment. Instillations of drugs are prescribed (medical observation). It is worth noting that eye drops do not improve vision and do not cure cataracts, but can stop destructive changes in the lens. Such drugs are prescribed after a full examination by the attending physician.
Features of complicated cataracts
Initially, such a cataract develops in the back of the lens (posterior capsular cataract), including due to the fact that its back wall is not protected by the epithelium, so decay products penetrate into the lens most easily in this place.
Gradually, the clouding, initially weakly expressed, increases in size and becomes less and less transparent, eventually completely covering the back of the lens capsule. A cup-shaped cataract occurs, in which the main surface and core of the lens remain transparent, but vision decreases. The turbidity gradually spreads to the core.
Much less often, a swelling complicated cataract is detected, which is characterized by the fact that the size of the lens increases while the anterior capsule contracts.
Treatment
In most cases, the disease is treated surgically, the most common method being ultrasound phacoemulsification of cataracts. This operation is performed using a special ultrasound device, the tip of which is inserted into the anterior chamber of the eye through a micro-incision (approximately 2-3 mm). Under the influence of ultrasonic vibrations, the natural lens is crushed into small parts and turned into an emulsion. Through a system of tubes, the masses are carefully removed from the eye. After removal of the lens, a special intraocular lens (artificial lens) of a certain optical power is placed.
Advantages of this treatment method:
- Instant recovery after surgery;
- Painless;
- Does not require surgical sutures;
- Performed under local anesthesia.
It should be noted that in the surgical treatment of cataracts, the correct choice of artificial lens is important. The right choice is the key to successful treatment! In the ophthalmology department of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, lenses from the most advanced companies are implanted - Alcon, Bausch&Lomb, Human optics and others. For cataract surgery, both “standard” or “ordinary” lenses and high-tech lenses (or premium lenses) are used - toric, multifocal, multifocal-toric, which correct not only corneal astigmatism, but also provide high visual acuity at different distances .
Etiological classification
Due to their occurrence, acquired cataracts can be divided into several subgroups:
- Age.
- Traumatic.
- Complicated.
- Radiation.
- Toxic.
- Cataracts arising as a consequence of existing endocrine diseases (hypothyroidism, diabetes mellitus and diabetes insipidus, other metabolic changes).
Complicated cataracts are observed when other pathologies are added to the underlying disease: glaucoma (can form due to uveitis - inflammation of the choroid), retinal pigmentary degeneration, high degree of myopia (myopia) and some other ophthalmic pathologies.
The most common cataract that occurs due to metabolic disorders is diabetic. It is typical for young people suffering from severe diabetes mellitus and occurs in both eyes at once. It is characterized by a rapidly progressing nature of development. Adequate and complete treatment with insulin and other antidiabetic drugs can temporarily slow down the development of cataracts.
Classification by degree of maturity
The following classification refers to the division of the disease according to the degree of maturity:
- Initial.
- Immature.
- Mature.
- Overripe.
Primary cataract
At the earliest stage, there is an accumulation of a large amount of excess fluid in the lens, the so-called “hydration of the lens.” Liquid accumulates between the fibers of the cortical layer of the lens along the localization of the cortical sutures. “Water gaps” appear. As a result, specific cortical opacities are formed.
Immature cataract
Further development of the disease is characterized by the progressive development of opacification towards the capsules and the central zone of the lens. While in the initial stage of cataract the clouding is localized along the equator, i.e. outside the optical zone, and it could not affect visual acuity in any way, in the immature stage the clouding already partially or completely covers the visual zone, which leads to a significant deterioration vision.
Mature cataract
During further development, the clouding spreads completely to the entire cortex of the lens, all zones are affected.
Some ophthalmologists divide this stage into:
- Almost mature - most zones of the lens cortex are affected, the patient can see no more than two lines of the table, visual acuity ranges from 0.1-0.2% to hundredths of a percent (the patient can only count the number of fingers in front of the eyes).
- Mature stage – total clouding of the lens, visual acuity drops to the level of light perception.
Overmature cataract
With further development of the disease, the fibers of the lens disintegrate. There is a liquefaction of the cortex, the capsule becomes folded. The bark acquires a characteristic milky white color. The core of the lens, located in a liquid medium, falls down due to its own gravity. The lens at this stage looks like a bag.
Complicated cataract
The reasons for the addition of certain complications to the underlying disease can be various primary pathologies.
Anterior uveitis in the chronic stage is the main cause of secondary cataracts. At the very beginning, a polychromatic (multi-colored) sheen can be identified in the posterior pole region. After uveitis is relieved, further development may stop. If attempts to relieve uveitis are unsuccessful, the opacification will progress until the formation of mature cataracts.
With an exacerbation of angle-closure glaucoma, small, grayish-white opacities of subcapsular and capsular localization may form in the projection of the pupil. In other words, as a consequence of an exacerbation of glaucoma, local degeneration (destruction) of the epithelium develops.
High myopia (myopia) can lead to the development of opacification under the posterior capsule, accompanied by sclerosis of the nucleus. The normal course of uncomplicated myopia does not lead to the formation of cataracts.
Retinal dystrophies of hereditary origin (Leber amaurosis, retinitis pigmentosa, Stickler syndrome, “spiral atrophy”) are sometimes accompanied by opacities in the posterior capsule. Cataract removal can lead to improved vision even with significant degenerative changes in the retina.
Treatment of complications
Postoperative cataract complications require the participation of highly qualified doctors in the treatment. Any patient needs to develop an individual technique. Most often, conservative therapy is carried out for 10-12 days and it turns out to be very effective.
Secondary cataract is a common late postoperative complication. The reason for its formation is the transformation of unremoved epithelial cells of the lens into lens fibers. The operation involves creating an opening in the posterior capsule (posterior capsulostomy). The traditional method consists of surgical removal of the film mechanically, but a more gentle method is YAG - laser capsulostomy, which is not accompanied by mechanical invasion of the eye cavity.
Irvine-Gass syndrome (cystoid macular edema) can occur as a result of phacoemulsification of cataracts. Occurs in approximately 1% of cases. Therapy is carried out by prescribing corticosteroid drugs, angiogenesis inhibitors, and NSAIDs. If conservative treatment is ineffective, then surgical treatment is indicated - vitrectomy.
The most difficult complications to treat are those requiring repeated surgery. It is in such severe cases that the need for vitrectomy can be attributed. The essence of the treatment is the removal (extraction) of the entire vitreous body or that part of it in which the greatest concentration of opacities is concentrated, interfering with visual acuity. The operation is carried out in several stages. As a result, a secondary lens is formed, which is able to fully restore the patient’s vision.
If pathological changes are noted in the postoperative period, adhesions or scars form in the retinal area, this is an indication for laser treatment.
Surgeries to treat glaucoma can often lead to complications. In such cases, a one-stage two-stage operation is performed, aimed at treating both pathologies at once. The first step to remove glaucoma is non-penetrating deep sclerectomy. The second stage involves cataract removal (ultrasonic phacoemulsification and simultaneous implantation of an intraocular lens).
Treatment of cataracts at the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency
In the ophthalmology department of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, doctors use the most modern equipment:
- Surgical combine from DORC, which is designed for cataract surgery and retinal pathology. It has high accuracy, provides excellent clinical results, and a quick rehabilitation period.
- Infiniti phacoemulsifier from Alcon, designed for cataract surgery. A high-tech, multifunctional phacoemulsifier that ensures the highest level of surgical performance and shortens the postoperative period;
The professionalism and extensive experience of doctors will help to diagnose cataracts early and carry out the necessary treatment:
- Our center performs operations of any complexity, even at the most advanced stages of the disease;
- Taking into account the presence of a multidisciplinary hospital, resuscitation and anesthesiology service, we perform operations on somatically severe patients with a risk of developing cardiovascular complications;
- We guarantee an individual approach to each patient. The treatment method is selected based on the causes of the disease and the stage of its development, the characteristics of the body, taking into account the wishes of the patient.