Content:
- 1 Structure of the ciliary muscle
- 2 Accommodation mechanism
- 3 Innervation of the act of accommodation
- 4 Accommodation study
- 5 Determination of accommodation reserves and their stability
- 6 Study of convergence, its reserves and sustainability
- 7 Signs of accommodation spasms
- 8 Causes of accommodation spasms
- 9 Types of accommodation spasms 9.1 Artificial accommodation spasm
- 9.2 Physiological spasm of accommodation
- 9.3 Pathological spasms of accommodation
Description
↑ Structure of the ciliary muscle
The question of the mechanism of accommodation is the subject of a large number of scientific studies and theories.
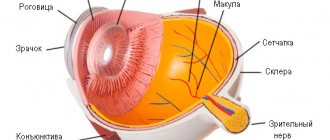
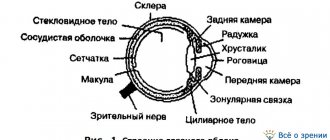
When an object approaches a constant light-refracting optical system, the image it creates will move away from it and, conversely, when the object moves away from the eye, the image will approach the retina (Fig. 1).
In the accommodation of the human eye, according to Helmholtz's theory, there are two parts - active and passive. The active part is carried out by the ciliary, or accommodative, muscle, the passive part is carried out by the ligament of Zinn and the lens.
The ciliary muscle, located in the ciliary body, belongs to the smooth muscles and consists of three types of muscle fibers with at least double innervation. In cross section, it has the shape of a triangle, becoming thinner towards the flat part of the ciliary body. The presence of the muscle gives the ciliary body its characteristic (in cross-section) triangular shape.
The muscle fiber bundles are located in three directions: meridional, circular (or equatorial) and radial.
The meridional fibers (Brücke muscle) are located under the sclera itself, parallel to it and form
the outer part of the ciliary muscle. Originating from the inner layers of the choroid and the border plate of the vitreous, they stretch to the limbus, where they attach to the scleral spur and partly to the trabeculae. Circular fibers (Müller's muscle) are located in the anterior internal part of the ciliary body in the form of separate ring-shaped muscle bundles. From the scleral spur, radial fibers (Ivanov's muscle) diverge in a fan-shaped manner to the pars plana and processes of the ciliary body.
The structure of the ciliary muscle
The ciliary muscle is formed at the equatorial part of the eye, in the area where the pigment tissue of the suprachoroid is located. Near the serrated edge of the retina, the muscle elements become more numerous and form peculiar loops, which are the initial section of the ciliary muscle.
The organ is formed by three types of fibers:
- Circular, located inside the ocular structure and without attachment. Their second name is Müller's muscles. The type of innervation of these structures is parasympathetic.
- Meridional (Brücke muscles), connected to the sclera. Such fibers have the greatest length, reaching 7 mm, parasympathetic innervation.
- Radial (Ivanov's muscles), acting as the basis of the organ. By contracting, these muscles move most of the ciliary body towards the root of the iris. Ophthalmologists consider the innervation of the radial muscles to be sympathetic.
The blood supply to the ciliary muscle is due to the presence of four anterior arteries. Venous outflow is provided by several veins located in front.
↑ Accommodation mechanism
Helmholtz (1855) believed that during the rest of the ciliary muscle, the ligament of Zinn is “tight. It is connected on one side with the ciliary body, and on the other with the lens bag and exerts some pressure on the latter. As a result of this action on the lens capsule, the ligament of Zinn does not allow it to take on a more convex shape, which it could have due to the elasticity of its fibers.
The accommodative muscle, during its contraction (the immobile beginning of the muscle at the skeleton of the angle of the anterior chamber of the eye), pulls the posterior part of the ciliary body and the anterior part of the choroid anteriorly. At the same time, the fibers of the zinc ligament relax, the forces tensing the lens capsule decrease, and due to elasticity it becomes more convex.
Helmholtz noted the following changes in the human eye during accommodation:
- constriction of the pupil during accommodation for near, dilation during disaccommodation (found by Scheiner back in 1619).
- Moving forward (into the anterior chamber) the center of the anterior surface of the lens and the pupillary edge of the iris.
- The surfaces of the lens become more convex during accommodation (the anterior one is larger than the posterior one) and less convex during disaccommodation. This was noted by Scheiner (1619) and Descartes (1619) (cited by M?tze, 1956). The first accurate studies of this phenomenon were given by Langenbeck (1849) and Kramer (1854; cited by Mütze) and independently by Helmholtz (1655). The thickness of the lens increases with accommodation by 0.4
mm (from
3.6
to
4.0
mm). - During accommodation, the peripheral belt of the iris moves slightly posteriorly, so that a depression of the anterior chamber is formed (especially in children). Gulstrand clearly observed this phenomenon using a corneal microscope, as well as the forward movement of the central part of the anterior surface of the lens. In addition, Hess (1903, 1909) observed that the lens moves downward by 0.25-0.3
mm during accommodation (Hess's phenomenon) and that with small movements of the eye there is a tremor of the lens.
These observations provide very significant support for Helmholtz's theory, as they confirm the relaxation of the fibers of the ligament of Zinn during accommodation.
↑ Innervation of the act of accommodation
Many studies have been devoted to the question of the essence of the accommodation process. For theory and clinical practice, questions about the innervation of the accommodative process and the essence of the “rest” state of the accommodative muscle are of paramount importance.
Back in 1866, Trautveter found that when the oculomotor nerve is irritated, the Purkinje-Sanson figures decrease, which indicates a decrease in the radius of curvature of the lens surfaces. This confirmed the idea that accommodation is carried out using parasympathetic innervation (as part of the oculomotor nerve).
This view was shaken after the publication of the results of the experiments of Mogakh and Doyon (1891), according to which a decrease in the Purkinje-Sanson images was observed during irritation and an increase when the cervical sympathetic trunk was cut. This observation showed that there is a double innervation of accommodation: the oculomotor nerve for close distances, the sympathetic nerve for distances.
Both opponents and defenders of this view appeared in the literature. Thus, Hess and Heine (1898) were unable to confirm with their experiments the participation of the sympathetic nerve in the innervation of accommodation. Lokshin (1938) on 20
animals after excision of part of the cervical sympathetic trunk on one side could not skiascopially find changes in the refraction of the eye.
However, the hypothesis of double innervation of the act of accommodation has found many supporters and over time their number is increasing. Poos (1928) used ephedrine, cocaine, and adrenaline in the form of drops or subconjunct injections, which irritate the sympathetic nerve. In all his experiments, under the influence of drugs irritating the sympathetic nerve, a mild paresis of accommodation was observed, which proved the presence of sympathetic innervation.
Cogan (1937) skiascoped the eyes of animals before and after stimulation of the sympathetic nerve. He also received evidence of the presence of sympathetic innervation, because refraction when irritated by the sympathetic nerve changed towards hypermetropia. Castelli (1935) 29
a person found accommodation paresis from
1.0
to
3.0
D after using adrenaline. I. S. Shimkhovich (1941), T. K. Dzharakyan (1946) obtained a clear distance from the nearest point of clear vision under the influence of subconjunctival injections of adrenaline.
S.I. Polner (1946) in the clinic led by prof. E. Zh. Tron, studied accommodation using the ergograph of A. V. Lebedinsky and N. I. Zimkin (1936) before and after the action on the eye 5%
cocaine solution drop by drop
3
times a day and adrenaline (
1:1000
) in the form of subconjunctival injections.
These observations allowed him to identify the occurrence of accommodation paresis with an average of about 2.0
D and thereby confirm the participation of the sympathetic nerve in the innervation of accommodation.
A. V. Lebedinsky (1948), summing up numerous studies of this issue, came to the conclusion that there is an undoubted presence of double innervation of the act of accommodation. Somewhat later, Meesmann (1952) and Monje (1952) came to the same conclusion. Both authors confirmed the opinion expressed by A.V. Lebedinsky (1948) that adrenaline can limit the experimental tension of accommodation.
They write that irritation of the parasympathetic nerve causes contraction of the ciliary muscle, while the use of sympathomimetic substances weakens the muscle. These authors propose to consider the relaxation of the accommodative muscle not as passive, as it was previously considered, but as an active process. By this they revise the concept of rest of the accommodative muscle, believing that its state when installed at a distance depends on the tone of the autonomic nervous system, taking into account the state of the antagonists - the sympathetic and parasympathetic nerves.
Thus, the generally accepted idea that the accommodative muscle is at rest at distance should indeed be reconsidered. Recognition of the presence of antagonistic innervation of the ciliary muscle entails the recognition that when one part of it is relaxed (for example, the circular one), the tone of the second increases.
Even V.P. Odintsov (1938) wrote that, although accommodation is understood as the ability of the eye to enhance refraction, “strictly speaking, the reverse process should also be included in the phenomena of accommodation - weakening of refraction, necessary for transferring vision from closer to more distant objects.” .
In this regard, the work of the Baku Ophthalmological School, led by prof. U. X. Musabeyli. The increase in refraction (towards myopia) obtained by U. X. Musabeyli and K. A. Adigezalova-Polchaeva (1958) when the eye is exposed to agents that block the sympathetic nervous system is another proof of the correctness of the issue of antagonistic autonomic innervation of the ciliary muscle. U. X. Musabeyli recommends that in order to determine the true refraction, in addition to atropine, which paralyzes the annular part of the ciliary muscle (Müller’s muscle), also use adrenaline, which stimulates accommodation into the distance.
Innervation
— Two types of fibers: radial and circular receive parasympathetic innervation as part of short ciliary branches from the ciliary ganglion. Parasympathetic fibers originate from the accessory nucleus of the oculomotor nerve and, already as part of the root of the oculomotor nerve, enter the ciliary ganglion.
- Meridian fibers receive sympathetic innervation from the plexus located around the carotid artery.
— The ciliary plexus, which is formed by the long and short branches of the ciliary body, is responsible for sensory innervation.
↑ Study of accommodation
The study of accommodation must be carried out in the form of determining its volume using the formula: A = (1/p)-(1/a)
, where
a
is further,
p
is the closest point of clear vision. Since a depends on the static refraction of the eye, the study comes down to determining the nearest point of clear vision using a conventional accommodometer.
More indicative for studying the influence of visual work on accommodation is the study of its stability, the study of which began in 1914. Lancaster and Williams (cited by N.I. Zimkin, 1937) found that the closest point of clear vision during long-term fixation of the test through 20—40
minutes begins to move away. Howe (1935) and Berens (1932) applied the ergographic principle for this purpose. The ergographic method, developed by A. M. Zimkina, N. I, Zimkin and A. V. Lebedinsky (1932), consists of continuously recording on a kymograph the positions of the nearest point of clear vision by maximally approaching and slightly moving away the test object (Fig. 2) .
Under 1
By the 1st closest point of clear vision on the ergograph, these authors understood the position of the Landolt optotype in front of the eye, at which the gap in the optotype ceased to be visible, by the
2nd
- the position corresponding to the moment the gap appeared when the optotype was moved away.
When the optotype is reapproached, the accommodation voltage again reaches its maximum value. The difference between the position of the 1st
and
2nd
points in young people is
2-4
cm, in older people it can reach
10-20
cm (Fig. 3).
With a stable nature of accommodation, the ergogram remains horizontal, i.e., the distance of the nearest point of clear vision from the eye does not change.
If stability is insufficient (Fig. 4), they change as the distance between 1
1st and
2nd
points of clear vision, and their distance from the eye - the oscillation curve becomes wider and acquires an ascending character.
Our clinic uses a simplified method for determining the stability of accommodation using a conventional accomodometer.
The examiner marks on the scale of this device the moment the test object disappears (1
-th point) and the moment of its appearance when moving away from the eye (
2nd
point). With the difference in readings for these points and their distance from the eye, a curve of accommodation stability is constructed. This technique is quite suitable for practical purposes; easily applicable in any conditions; limited to the use of such a simple device as an accomodometer; allows you to do without a recording ergograph.
N.I. Pilman in the book “Practical Issues of Pediatric Ophthalmology” (1967) writes that “eye ergographs are still of little use for everyday work. For practical purposes, it is enough to determine the reserve of accommodation and convergence and their stability using the method of A. I. Dashevsky.”
↑ Determination of accommodation reserves and their stability
To rationally characterize the state of accommodation and convergence and their stability, the reserves of these functions should be determined separately. We introduced this rule in 1940 and consists of studying accommodation reserves when turning off convergence and vice versa.
In front of the eye (refractive errors are completely corrected, the second eye is covered with a white shield) a concave glass is placed with a force of 0,5—1,00
. The subject, transformed by this into a slight hypermetrope, experiences some difficulty in reading the last line on the table to determine visual acuity, but now reflexively, through the appropriate strain of accommodation, strengthens his refraction and thereby overcomes the effect of a negative glass placed in front of the eye.
Since the eye-plus-glass system again becomes emmetropic, his visual acuity again reaches 1,0
within a few seconds.
This “load” continues by adding 0.5-1.0
D each time until the maximum number of diopters that the eye can overcome with the help of its accommodation is reached.
This number of diopters does not always correspond to the age-related volume of accommodation in a given person; in healthy eyes it can be equal to 2/3
to
3/4
of this volume.
Once the accommodation reserve (expressed in diopters) has been quantified in this way, the stability of accommodation should be studied. The strongest negative glass with which visual acuity is equal 1,0
, leave in front of the eye for
3-5
minutes.
If the stability of accommodation is satisfactory and the accommodative muscle is able to withstand this rather long-term load, then visual acuity will always remain equal to 1.0
(or its original value, if before the study it was less than
1.0
).
If the stability of accommodation is insufficient, the latter quickly relaxes, the caused reflex tension disappears, and the optical system “eye plus glass” again becomes hypermetropic; At the same time, visual acuity decreases. The more hypermetropia increases due to the weakening of accommodation tension, the less visual acuity will be. If we plot time (in minutes) on the abscissa axis, and visual acuity on the ordinate axis, we get a graphical characteristic of the state of accommodation stability. With stable accommodation, the curve will be horizontal; with unstable accommodation, it will be inclined (Fig. 5).
The main advantage of this method is the ability to study the reserves and stability of accommodation while completely excluding the influence of convergence (each eye is examined separately).
Muscular apparatus of the eye
Description
Nature created the eye to be spherical.
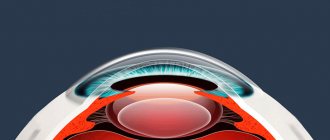
Therefore, it can easily rotate around three axes: vertical (left to right), horizontal (up and down) and the optical axis of the eye. There are three pairs of extraocular muscles around the eye, which rotate the eye accordingly. The muscles themselves are controlled by signals coming from the brain. Oculomotor muscles
, perhaps the fastest-acting in the human body.
When examining, for example, a painting, the eyes move spasmodically, making up to 120 leaps per minute, and the duration of one leap is only a few hundredths of a second. In addition to such jumps, the eye continuously makes small but very fast oscillations (up to 120 per second). They are extremely important for the functioning of the eye itself, especially when viewing small objects. As soon as the close examination stops, the vibrations themselves disappear. According to some scientists, the oculomotor muscles have another motor function - they can help the lens of the eye focus the image on the retina when objects are at different distances from the eyes. The muscles slightly “stretch” or “compress” the eyeball, thereby moving the retina of the eye, moving it away from or closer to the lens. The ciliary muscle
“works” with the lens itself .
To obtain images of near and distant objects on the camera plate, you have to focus the camera by moving the lens forward or backward. A similar phenomenon occurs in the human eye - focusing of the image on the retina, called accommodation
. But it is carried out not by moving the lens, but by reducing or increasing its refractive power due to a change in the curvature of the lens itself. The main role in this process belongs to the above-mentioned ciliary muscle located around the lens (Fig. 2).
Rice. 2.
Accommodation system. The left half of the figure corresponds to the state of the lens during resting accommodation, i.e. looking into the distance, the right half corresponds to the state of the lens when viewing objects at a close distance, the lens takes on a more convex shape.
The ability of the eye to accommodate is examined using ocular ergography.
, allowing you to accurately determine the degree of visual fatigue. It was introduced into ophthalmological practice to assess the state of accommodation by Soviet ophthalmologists led by E. S. Avetisov (Moscow) and V. V. Volkov (Leningrad). Ergography is carried out using a special device. Ergography has also proven to be a valuable method for identifying dynamic refractive disorders of the eye in children and adolescents with myopia, as well as for assessing visual performance in individuals engaged in delicate and precise production operations.
Accommodation of the eye
- the most important regulator of vision function, but with age the power of accommodation gradually decreases, because the lens itself becomes less elastic. A phenomenon called senile farsightedness, or presbyopia, occurs. Due to weakening of accommodation, a person tends to move a book or newspaper away from his eyes (to facilitate the work of the ciliary muscles) or resorts to glasses with convex lenses. In contrast, with myopia (due to the elongation of the longitudinal axis of the eye and weakness of the ciliary muscle), images of objects are focused not on the retina itself, but in front of it. This is why myopic people tend to bring everything closer to their eyes: they use glasses with concave lenses to reduce the refractive power of the lens (Fig. 3).
Rice. 3.
On the left is the course of rays (from top to bottom) in a normal, far-sighted and myopic eye. On the right is the course of rays with glasses. The image is focused on the retina
From all that has been said, it becomes clear how important it is to train the ciliary muscles, as well as the muscles surrounding the eye, to preserve them from premature weakening.
—-
Article from the book: Train your eyesight | Demirchoglyan G.G.
↑ Study of convergence, its reserves and sustainability
When studying convergence, it should be taken into account that its maximum tension can be studied by determining binocularly the position of the nearest point of convergence, for which both accommodation and convergence are important. It is interesting that in the process of visual work, the binocular closest point significantly approaches the eyes, remaining in this position even after an hour of rest.
A weak prism is placed in front of one refractively corrected eye (base towards the temple), usually with a force of 10—12
prism diopters (A).
The subject notes the bifurcation of a small lamp located at a distance of 2
to
5
m from him. The prism deflects the beam towards its base. In the eye, the beam falls on the temporal part of the retina, and since in the eye, in front of which there is no prism, the light beam goes to the central fovea of the macula, double vision occurs.
To help the patient notice diplopia, a red glass can be placed in front of the other eye (although this is not necessary). Quite quickly, both images of the lamp merge into one due to additional contraction of the internal rectus muscle of the eye, in front of which the prism is placed.
This contraction is necessary to turn the eye inward so that the light beam deflected by the prism hits the direction of the central fovea of the macula and both beams end up at the corresponding points of the retinas of both eyes. Then take a stronger one (at 2—3?
) prism, diplopia is again obtained, the two images are again achieved to merge into one, and this continues until the strongest prism is found, which can still be overcome with the help of additional convergence caused by the fusion reflex.
With asthenopia caused by weakened convergence, the subject sometimes cannot overcome the diplopia created by applying even a weak prism. by force in 1—:2—3?
. The same thing happens with false and progressive myopia.
To determine the stability of the maximum strength of convergence found in this way, leave a prism in front of the eye for 5
minutes. After every minute, the prism is removed and placed again in front of the eye. With satisfactory stability of convergence, double vision is easily overcome every time; with unstable convergence, persistent diplopia occurs; in the second case, the force of the prism that the subject under study can overcome is determined in the manner described.
If we plot prism diopters on the ordinate axis, and time in minutes on the abscissa axis, we get a graphical characteristic of the stability of convergence. With stable convergence, the curve will be horizontal, and with unstable convergence, it will be inclined (Fig. 6).
In this way, the reserves and stability of convergence are determined independently of accommodation, because the study is carried out at a large distance and for each eye separately.
↑ Signs of accommodation spasms
An accommodation spasm should be considered an involuntary contraction of the ciliary muscle, i.e. its involuntary tension. Usually spasms of accommodation are bilateral, although cases of “anisospasms” are certainly not uncommon. Spasms of accommodation have been known for a long time. Leading ophthalmologists XIX
centuries recognized their great clinical significance. However, later ophthalmologists stopped paying attention to many signs indicating the presence of spasms of accommodation. As a result, a number of previously known signs of accommodation spasms are now forgotten.
We present in a slightly adapted form the signs of spasms of accommodation described by one of the founders of Russian ophthalmology, E. V. Adamyuk (1881).
- Decreased vision, noticed recently, mostly under the influence of intense exercise.
- Rapid fatigue when working at close range, pain in the eyes and their surroundings, photophobia, increased tear production, desire to bring the book closer to the eyes. These signs of asthenopia appear both with hypermetropia and with increased refraction to myopic with a decrease in visual acuity.
- Reducing the volume of accommodation. E. V. Adamyuk defined it by the distance from the nearest point of clear vision. We have described a more modern and accurate method for determining accommodation reserves (A.I. Dashevsky, 1940, 1962, 1970, 1971).
- In case of myopia, the application of positive lenses causes a deterioration in distance visual acuity; with a spasm of accommodation (false myopia), no deterioration in visual acuity is observed after a short time; sometimes there is a slight increase (due to passive relaxation of the spasm) in visual acuity.
- Attaching positive lenses for true axial myopia forces the text to be brought even closer to the eyes at a close distance. With a spasm of accommodation, reading is possible even at a great distance (due to relaxation of the spasm).
- Repeated determinations of refraction on the same day, and even more so on different days, reveal a constant refraction in case of myopia, and an unstable refraction in case of accommodation spasm.
- E.V. Adamyuk recommends that after determining the refraction, transfer the subject to a dark room for a few minutes and repeat the study again. With myopia, the refraction will remain the same; with a spasm of accommodation, it will be weaker due to relaxation of the ciliary muscle.
- This symptom should be called the symptom of E. V. Adamyuk.
- More than 90
years ago, E. V. Adamyuk paid special attention to the most important symptom of asthenopic phenomena and their consequences - spasm of accommodation - weakness of the internal rectus muscles. True, he did not describe a method for determining the weakness of convergence. The weakness of convergence can best be judged by the state of the convergence reserve (A.I. Dashevsky, 1940, 1962, 1970, 1971). - The main symptom of accommodation spasm is a decrease in refraction at the height of cycloplegia.
Diseases of the ciliary muscle and their symptoms
The ciliary muscle may develop the following pathologies:
- paresis, manifested in the form of partial paralysis, arising against the background of damage to the organs of vision;
- spasm of accommodation, causing false myopia and other visual impairments;
- cyclitis, provoking the inflammatory process.
If the organ in question experiences a pathological condition, the person experiences a variety of negative symptoms. The patient may complain of:
- reduced visual acuity;
- pain, burning in the eyeballs;
- recurrent pain;
- dizziness;
- excessive fatigue of the visual apparatus.
Frequent manifestations of disorders in the area of the ciliary muscle are redness of the conjunctival membrane, dry eye syndrome, and a sensation reminiscent of small objects getting into the eyes.
The ciliary muscle is especially sensitive to regular eye overload that occurs during prolonged periods of time at the computer, hours of watching TV, and reading in low light. In such situations, a phenomenon called accommodation syndrome is often observed.
↑ Causes of accommodation spasms
Among the causes of spasms of accommodation, E. V. Adamyuk (1881) put in first place blurred vision due to various optical imperfections of the eye (mainly ametropia, clouding of the cornea, vitreous body, etc.), i.e. vision in circles of light scattering.
For better visibility, you have to bring objects closer to your eyes; increased accommodation and convergence can lead to a spasm of accommodation. Poor lighting when working at close range also leads to this.
All causes leading to weakening of the sympathetic or irritation of the oculomotor or trigeminal nerve (due to a reflex effect on the oculomotor) often cause miosis and a parallel increase in accommodation.
Children suffering from chronic intoxication, and therefore a general weakening of the body, usually develop a neurasthenic syndrome, accompanied by irritability, tearfulness, fatigue, sleep disorders, attention exhaustion, etc. With chronic intoxication in children, the balance between irritable and inhibitory processes is disturbed (R.A. Kalyuzhnaya, 1965) with a predominance of either inhibitory states of the cerebral cortex (for example, with a focal infection in the oral cavity and nasopharynx) or an irritable process (for example, with chronic tuberculosis intoxication). This leads to various disorders in the area of the autonomic centers, hypothalamus, endocrine glands, etc.
R. A. Kalyuzhnaya (1965), having studied the functional state of the autonomic nervous system in children during various chronic intoxications, found that with a short time from the onset of tonsillogenic and other intoxications, a high level of sympathetic activity is usually observed; over a longer period of time, sympathetic effects decrease, and a relative predominance of parasympathetic reactions appears. Consequently, with chronic intoxication in children, autonomic dystonia consists of a decrease in sympathetic activity and a relative predominance of parasympathetic activity.
If, due to tonsillogenic, rheumatogenous, tuberculogenic, helminthic, hepatogenic (especially after Botkin's disease) and other chronic intoxications in the body, a predominance of parasympathetic over sympathetic innervation is established, this cannot but affect the state of accommodation of the eye. The predominance of parasympathetic activity (innervation of the Müller muscle) over sympathetic activity (innervation of the Brücke muscle) necessarily leads to the predominance of the accommodation mechanism for near over accommodation at distance.
Under unfavorable hygienic conditions, chronic intoxication, accompanied by vegetative dystonia, expressed in the prevalence of parasympathetic innervation, creates favorable conditions for the occurrence of spasms of accommodation. Therefore, chronic intoxication of the body, especially in children, is one of the most important factors contributing to the development of resistance to spasms of accommodation (V. A. Asabina, 1971).
Among other reasons, special mention should be made of the low reserves of accommodation and convergence identified by E.V. Adamyuk. They are especially low in eyes with astigmatic refraction. Measurement of accommodation and convergence reserves carried out by A.F. Nedelka (1970) in children with astigmatism showed a sharp decrease compared to the age norm.
The occurrence of false myopia is usually attributed to the school period of life. However, cases of pseudomyopia have also been described in preschool children, which is facilitated by the visual load that appears at this age, previous general diseases and many other factors.
The causes of spasms can be divided into the following groups:
- state of the body: intercurrent diseases, chronic intoxication with weakening of the body, vegetative dystonia, ametropia, instability and other disorders of binocular vision, insufficiency of fusional and other functional reserves, etc.;
- environmental factors: poor lighting when working at close range, incorrect posture, bringing the text too close to the eyes, improper daily routine (work and rest), a sharp reduction in time in the fresh air, etc.;
- heredity or hereditary predisposition to spasmodic conditions.
Already V.I. Dobrovolsky (1868) believed that the development of accommodation spasm with emmetropia or hypermetropia contributes to the appearance of visible myopia - pseudomyopia. In his opinion, more 80%
cases of weak myopia (up to
0.5
D) are caused by a spasm of accommodation. At the same time, he reported that with myopia, spasm can be detected at any degree in 60% of cases. He found spasms of accommodation not only with low, but also with high myopia.
The data of V.I. Dobrovolsky were confirmed by Schr?der (1874), who found spasms of accommodation with myopia in 77%
, H?sch and Schiess, who found spasms of accommodation in
81
and
85%
of persons with mild myopia, respectively.
Currently, the opinion about the presence of spasms in a large percentage of cases of myopia is confirmed by many authors. Ticasi Sato (1957) showed in his works the high prevalence of pseudomyopia among Japanese students. K. A. Adigezalova-Polchaeva (1959, 1963) observed spasms of accommodation in 97%
of people with a low degree of myopia, in
72%
a moderate degree of myopia, and in
62%
of people with a high degree of myopia.
Asthenopia - symptoms and treatment
The doctor develops a comprehensive treatment strategy based on the patient’s individual indications and the stage of development of the disorder:
- In the compensation phase, in the absence of pathological changes, patients are recommended to give their eyes the necessary rest during visual stress: every 35-45 minutes, take a break for 15-20 minutes;
- In the subcompensation phase, patients are prescribed hardware treatment - laser stimulation to stabilize the work of the ciliary muscle, the use of a special synoptophore instrument for training the eye muscles, and therapeutic glasses. Glasses will help you get rid of the consequences of accommodative spasms and select the right tools for optical correction of myopia and farsightedness.
- In the decompensation phase, more serious measures will be required: the choice of glasses or contact lenses and eye drops. Drops for asthenopia:
- mydriatics - to relax the muscles responsible for contraction and dilation of the pupil;
- drops with antibacterial and antihistamine effects - used for infectious diseases of the eye;
- tear drops - for severe dryness of the mucous membranes;
- keratoprotectors - in the presence of microtraumas of the cornea.
When using drops, it is important to know that they differ in composition and properties. The dosage and duration of therapy must be observed. Some drops have no restrictions on the duration of use, others are addictive. Medicines for asthenopia are selected by an ophthalmologist.
When treating asthenopia, it is important to consider the main points:
- the correct choice of means of correcting visual impairment (glasses or contact lenses);
- eye drops to reduce the tone of the ciliary muscle and eliminate spasm of accommodation, use one drop every day or every other day at night for a month;
- proper nutrition containing sufficient amounts of vitamins;
- compliance with the work and rest regime.
Vitamins and traditional treatment
The benefits of taking vitamin complexes for asthenopia have not been proven. It is likely that symptoms of eye strain can be alleviated by taking blueberry extract and fish oil, but further research into the effectiveness of these products is needed [12].
Homeopathy
Homeopathy is a type of alternative medicine; there is no scientifically proven evidence of its effectiveness.
Physiotherapeutic treatment
To train accommodation reserves, hardware treatment methods are used: laser stimulation, color pulse therapy, magnetic therapy, electrical stimulation. However, there is no clear opinion about the effectiveness of physiotherapeutic treatment in the medical community.
Surgery
There is no surgical treatment for asthenopia.
Features of treatment depending on the form of the disease
In the case of symptomatic asthenopia, correction is carried out simultaneously with the treatment of underlying concomitant diseases. Treatment of the muscular form of ocular asthenopia begins with the elimination of strabismus (using orthoptics, diploptics) and correction of myopia. In the asthenic form, the cause should be determined and eliminated, the immune system should be strengthened, work and rest regime should be observed, and nutrition should be nutritious. The neurogenic form is treated by a neurologist.
Treatment of asthenopia takes a long time. When treating children, preventive measures and limiting visual load are of particular importance.
To relax the eye muscles, special daily exercises are performed. A set of eye exercises is chosen by an ophthalmologist based on the form of asthenopia.
Set of exercises
People whose activities regularly involve eye strain are recommended to do the following exercises daily:
Exercise 1. Closing your eyes. While sitting, close your eyes for five seconds, then open both eyes at the same time. Repeat seven times. Taking it will help relax the eye muscles, strengthen the muscles of the eyelids and normalize blood circulation.
Exercise 2. Blinking. While sitting, look straight ahead and blink intensely for a minute. Exercise normalizes blood supply to the eyes.
Exercise 3. Moving your gaze . Performed while standing. Look into the distance for a few seconds, then bring your index finger to your face at a distance of thirty centimeters from your eyes. Move your gaze to the tip of your finger and hold for five seconds. Lower your hand. Repeat ten times.
Exercise 4. Eyelid massage. Take a comfortable position on a chair, close your eyes and gently massage your eyelids with your fingertips. When massaging the upper eyelid, they move from the inside out, the lower eyelid - in the opposite direction. Perform for one minute. The procedure relaxes muscles and stimulates blood circulation.
Exercise 5. Alternating eye exercises. While standing, place your index finger at a distance of thirty centimeters from the eyes along the midline. Look closely at the tip of your finger for five seconds. Then, with the palm of your second hand, close your left eye, without taking your eyes off the object with your right eye. Then remove your palm and look at your finger for five seconds. Repeat the manipulation with the other eye. Repeat five times.
Exercise 6. Horizontal eye movements. Stand up and move your right hand to the side in a half-bent position, extending your index finger. Slowly move your hand to the side in the opposite direction, while carefully watching your finger. Then return your hand to its original position without taking your eyes off it. Do it ten times. Exercise helps strengthen the muscles responsible for horizontal eye movement.
Exercise 7. Pressing on the eyelids. Sitting on a chair, place three fingers on your closed eyes. Gently press on your eyelids for two seconds, then remove your hands. Repeat five times. Taking it helps improve the circulation of intraocular fluid.
Exercise 8. Fixation of gaze. Take a comfortable position on a chair and unfocus your gaze for five seconds, then move it to the tip of your nose. Repeat six times. Exercise improves the ability to keep your gaze on objects.
Exercise 9. Vertical eye movements. While standing, raise your half-bent arm up and extend your index finger. Fix your gaze on it and slowly move your hand down, then return to the starting position. Do it ten times. The technique strengthens the muscles responsible for the vertical movement of the eyeballs and trains the coordination of the visual apparatus.
Exercise 10. Circular movements. Sitting, the head is motionless. Raise your eyes up and move clockwise, and then in the opposite direction. Repeat five times.
Exercise 11. Movements in different directions. Standing, head motionless. Raise your gaze as high as possible, then lower your gaze. Look left and right. Repeat eight times. The exercise trains the visual apparatus.
Exercise 12. Static voltage. Sitting, the head is motionless. Close your eyelids and look up, then down, turn right and left. Do six times [4][3].
↑ Types of accommodation spasms
Spasms of accommodation are artificial, physiological and pathological (A.I. Dashevsky, 1962, .1968).
↑ Artificial spasm of accommodation
caused by the use of miotics - pilocarpine, eserine, armin, etc.
↑ Physiological spasm of accommodation
caused by contraction of the ciliary muscle to improve distance vision with hypermetropia and astigmatism. This is a long-term tension of the ciliary muscle, which disappears after eliminating the cause of the spasm, i.e., after correcting hypermetropia or astigmatism or eliminating previously allowed overcorrection with negative lenses. The spasm can relax during sleep, with distraction, etc. d.
A distinctive feature of physiological spasm or accommodation tension is an increase in refraction to emmetropia with an increase in visual acuity to 1.0.
↑ Pathological spasms of accommodation
They can be persistent (with ametropia) and true. The former are not true tonic muscle spasms. Tension of the accommodative muscle, caused by the need for self-correction of hypermetropia or astigmatism, is pathological if it becomes persistent. With visual fatigue, persistent spasm can also occur in emmetropes (false myopia), while complaints characteristic of accommodative asthenopia are observed. Persistent spasms of accommodation can only be relaxed with the help of mydriatics or special orthoptic treatment.
The main feature of pathological scasms of accommodation is a decrease in visual acuity due to false myopization.
True spasms of the ciliary muscle are almost always of central origin. With very persistent true tonic muscle spasms of accommodation, it is very rare to achieve full visual acuity with the help of correction.
Continued in the next article.