| This article includes a list of general recommendations, but it remains largely untested because it lacks relevant inline quotes . |
| Oculomotor nerve | |
| Orbital nerves. When viewed from above. | |
| Inferior view of the human brain with cranial nerves labeled. | |
| Details | |
| From | oculomotor nucleus, Edinger-Westphal nucleus |
| TO | higher branch, lower branch |
| Excites | Superior rectus, inferior rectus, medial rectus, inferior oblique, levator palpebrae superioris, sphincter pupils (parasympathetic), ciliary muscle (parasympathetic) |
| Identifiers | |
| Latin | oculomotor nerve |
| MeSH | D009802 |
| NeuroNames | 488 |
| TA98 | A14.2.01.007 |
| TA2 | 6187 |
| F.M.A. | 50864 |
| Anatomical terms of neuroanatomy [edit in Wikidata] | |
| Cranial nerves |
|
|
|
To the oculomotor nerve
third cranial nerve (CN III). It enters the orbit through the superior orbital fissure and innervates the extrinsic muscles of the eye, which allow movement of the eye and this lifting of the eyelid. The nerve also contains fibers that innervate the intrinsic muscles of the eye, which enable pupil constriction and accommodation (the ability to focus on close objects, as in reading). The oculomotor nerve originates from the basal lamina of the embryonic midbrain. Cranial nerves are also involved in the control of eye movement.[1]
Structure
The oculomotor nerve originates from the third nerve. nucleus at the level of the superior colliculus in the midbrain. The third nerve nucleus is located ventral to the cerebral aqueduct, on the preaqueduct there is gray matter. Fibers from two-thirds of the nerve nuclei, located laterally on either side of the cerebral aqueduct, then pass through the red nucleus. The fibers of the red nucleus then pass through the substantia nigra and exit through the intermaxillary fossa.
After exiting the brainstem, the nerve is covered by a sheath of the pia mater, and is attached to the continuation of the arachnoid. It passes between the superior cerebellum (below) and the posterior cerebral artery (above), and then pierces the dura mater anteriorly and lateral to the posterior clinoid process, passing between the free and attached borders of the tentorium cerebelli.
It crosses the cavernous sinus, over the other ophthalmic nerves, receiving along the way one or two filaments from the cavernous plexus of the sympathetic nervous system and a communication branch from the ophthalmic branch of the trigeminal nerve. As the oculomotor nerve enters the orbit through the superior orbital fissure, it then divides into superior and inferior branches.[1]
Higher department
To the highest branch
The oculomotor nerve or
superior division
, the smaller one, passes medially over the optic nerve. It supplies the superior rectus muscle and levator palpebrae superioris.
Lower branch
In the lower branch
The oculomotor nerve or
inferior division
, the larger one, is divided into three branches.
- One passes under the optic nerve to the medial rectus muscle.
- The other is to the inferior rectus muscle.
- The third and longest runs forward between the lower and lateral muscles. inferior oblique.
- A short thick branch extends from the third to the lower part of the ciliary node, and forms its short root.
All of these branches enter the muscles at their ocular surfaces, with the exception of the nerve leading to the inferior oblique muscle, which enters the muscle at its posterior border.
Cores
The oculomotor nerve (CN III) arises from the anterior part of the mesencephalon (midbrain). The oculomotor nerve consists of two nuclei:
- The oculomotor nucleus originates at the level of the superior colliculus. The muscles it controls are the striated muscle, the levator palpebrae superioris, and all the extraocular muscles except the superior oblique and lateral rectus.
- The Edinger-Westphal Nucleus stores parasympathetic fibers to the eye through the ciliary ganglion, and thus controls the pupillary sphincter muscle (affecting pupillary constriction) and the ciliary muscle (affecting the residence).
Sympathetic postganglionic fibers also connect to the nerve from the plexus on the internal carotid artery in the wall of the cavernous sinus and are distributed along the nerve, for example, to the smooth muscle of the superior tarsal muscle (Müller's muscle).
Myopia
Or in other words, myopia is poor discrimination of objects at a distance due to the image falling in front of the retina (and not on it). The picture becomes fuzzy and blurry.
Correction methods:
- Wearing contact lenses or glasses.
- Lens implantation.
- Laser correction.
- Lens replacement surgery.
- Corneal plastic surgery.
- Radial keratotomy.
If left untreated, myopia progresses rapidly, increasing the risk of significant vision loss.
Function
The oculomotor nerve contains GSE type axons, a common somatic efferent, that innervate the skeletal muscles levator superior palpebrae, superior rectus, medial rectus, inferior rectus, and inferior oblique (innervate all extrinsic muscles except the superior oblique and lateral rectus).
The nerve also includes GVE type axons, a common visceral efferent, that provide preganglionic parasympathetic input to the ciliary ganglion. From the post-ganglionic fibers of the ciliary ganglion through the short ciliary nerve they pass to the constrictor pupils of the iris and the ciliary muscles.
Spasm of accommodation
A person can clearly distinguish objects at a distance thanks to accommodation, which occurs when the lens, ciliary muscle and ciliary ligament are coordinated. Spasm is characterized by the appearance of persistent tension of accommodation even in cases where it is not necessary.
The list of causes of the disease is wide:
- Insufficient illumination of the work space.
- Excessive strain on vision.
- Short duration of night sleep, rare exposure to fresh air, lack of sports activities.
- Poor workplace equipment: the height of the writing table and chair does not correspond to the person’s height.
- Failure to maintain the optimal (30-35 cm) distance to the book when reading.
- Poor blood supply to the neck.
- Weakness of the neck and back muscles.
- Poor nutrition.
- Hypovitaminosis.
Associated symptoms:
- Frequent headache.
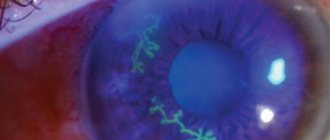
- Redness of the eyes.
- Cutting and burning in the eyes.
- Double vision.
- Blurry images at a great distance and reduced image clarity close up.
To treat the disease, drops that dilate the pupil are used, and a special set of exercises for the eyes is also recommended. If there is no effect from the above treatment, accommodation stimulation using laser, magnet and electricity is also used.
Clinical significance
Disease
Oculomotor nerve palsy, i.e., oculomotor nerve palsy, can occur due to:
- direct trauma,
- demyelinating diseases (for example, multiple sclerosis),
- increased intracranial pressure (leading to noncal hernia) due to a space-occupying lesion (eg, brain cancer) or
- spontaneous subarachnoid bleeding (eg, berry aneurysm), and
In people with diabetes and over 50 years of age, oculomotor nerve palsy in the classical sense occurs when the pupillary reflex is spared (or preserved). This is believed to occur due to the anatomical location of the nerve fibers in the oculomotor nerve; the fibers that control pupillary function are superficial and are not subject to ischemic injury characteristic of diabetes. In contrast, an aneurysm that results in compression of the oculomotor nerve affects the superficial fibers and manifests as third nerve palsy with loss of the pupillary reflex (in fact, this opening of the third nerve is considered an aneurysm - until proven otherwise - and should be investigated).[2]
Exam
Eye muscles
Cranial nerves III, IV, and VI are usually examined together as part of a cranial nerve examination. The examiner usually instructs the patient to keep his head still and follow only his eyes as a finger or flashlight outlines a large "H" in front of the patient. By observing eye and eyelid movements, the examiner can obtain additional information about the extraocular muscles, the levator superior palpebrae muscle, and cranial nerves III, IV, and VI. Loss of function of any of the eye muscles leads to ophthalmoparesis.
Because the oculomotor nerve controls most of the eye muscles, damage to it may be easier to detect. Damage to this nerve, called oculomotor nerve palsy, is known for its downward and outward
symptoms caused by the position of the affected eye (deviation of gaze to the side, down).
Pupillary reflex
The oculomotor nerve also controls the constriction of the pupils and the thickening of the lens of the eye. This can be checked in two main ways. By moving a finger towards a person's face to induce living, their pupils should constrict.
Light entering one eye should cause a similar narrowing of the other eye. The optic nerve neurons decussate at the optic chiasm with some overlap with the contralateral optic nerve tract. This is the basis of the "flashlight test".
Loss of vision and continued pupil dilation may indicate the presence of oculomotor nerve damage.
Heterophoria
Heterophoria, or hidden strabismus, causes a lot of inconvenience. Thus, when working with texts or objects at close range, eye fatigue occurs, and in some cases, double vision. The disease can be corrected only by constantly wearing prismatic glasses (no more than 2-3°). The main principle of making glasses for heterophoria is that the base of the prism should be directed in the opposite direction from the eye affected by the disease. For example, if a patient has an outward deviation of the eye, the doctor writes a prescription for glasses with prisms located inward.
What if, in addition to the pathology under consideration, the patient has both myopia and hypermetropia? No matter how difficult the situation may seem with these concomitant diseases, it is possible to eliminate heterophoria by decentering the corrective glasses. By reducing or increasing the interval between the pupils, optical glasses acquire the effect of a prism and the disease disappears.
Large degrees of heterophoria are corrected through surgery.
Recommendations
This article incorporates public domain text from page 884 of the 20th edition
Gray's Anatomy
(1918)
- ^ a b
Wilensky, Joel;
Robertson, Wendy; Suarez-Quian, Carlos (2015). Clinical Anatomy of the Cranial Nerves: The "Atop Olympus" Nerves
.
Ames, Iowa: Wiley-Blackwell. ISBN 978-1-118-49201-7.[ page needed
] - Oculomotor Nerve Palsy
at eMedicine
Nystagmus
The disease refers to uncontrolled eye movements. There are several forms of nystagmus:
- Horizontal.
- Vertical.
- Diagonal.
- Rotational.
The cause of the pathology lies in various diseases of the brain, namely its areas responsible for coordination. Somewhat less often, nystagmus is caused due to disturbances in the functioning of the vestibular apparatus, as well as in case of poisoning with narcotic substances and medications.
Like most pathologies associated with disorders of the oculomotor nerve, treatment consists of eliminating the underlying disease, against which the disturbing illness arose. Vitamins and antispasmodics can improve the patient's condition somewhat.
Oculomotor nerve palsy - causes, symptoms and treatment
Damage to the abducens nerve of the eye is one of the ophthalmological pathologies that have much in common with neurological disorders. With this disease, the movements of the eyeball are distorted. It often happens that it does not move, especially when you need to look to the right. Let's tell you more about this disease and its treatment.
In this article
- Pathogenesis of the disease
- Causes of abducens neuropathy
- Symptoms of pathology
- Diagnosis of abducens neuropathy
- Treatment of abducens neuropathy
Description of the pathology, development mechanism
The oculomotor nerve is part of the third pair of cranial nerves and consists of viscemotor and somatomotor (motor) fibers. Its main function is to provide motor ability to the eyeball. The nerve controls the following systems:
- Ciliary muscles;
- Sphincter of the pupil (provides its ability to expand and contract depending on the lighting);
- Optical-kinetic nystagmus (the ability to follow moving objects);
- Muscles to regulate the movement of the upper eyelids;
- Vestibulospectral reflex (the ability of the pupil to move when the head turns);
- Accommodation (change in the curvature of the eye lens depending on surrounding objects and phenomena).
Thus, damage to the optic nerve always entails a limitation in the functionality of the visual apparatus. The movement of the eye and pupil is limited or lost.
In turn, the lesion has its own reasons for occurrence or acts as a sign of another disease.
Men and women of all ages are at risk, but statistics show that children are more likely to suffer from oculomotor nerve palsy.
Anatomy of a nerve
The nerve responsible for eye movement has a mixed structure. This structural formation runs through several parts of the brain and provides innervation to several muscle groups.
When considering the features of the oculomotor nerve and its anatomy, it should be noted that it is divided into two parts:
- Motor. Connects the muscles that lift the upper eyelid and provide movement of the eyeball. These muscles connect to the central nervous system.
- Parasympathetic. Connects the muscles that cause the pupil to constrict and the lens to protrude and is also connected to the central nervous system.
Each nucleus of the oculomotor nerve is located in a specific part of the brain: in the aqueduct, on the superior colliculus, on the tegmentum. This formation is a two-neuron communication highway, thanks to which a large group of muscles functions simultaneously and continuously.
The oculomotor nerve contains a total of 5 nuclei, the arrangement of which provides innervation to the muscles that lift the upper eyelid and move the eyeball in the vertical and horizontal planes.
The muscles themselves that perform these functions are located in various areas near the organs of vision.
The oculomotor nerve, passing through the cranial structures, stops near the orbital part of the eye. In this zone it is divided into two parts:
- Upper. Provides eyelid movement.
- Bottom. It has a larger structure and is responsible for the work of other muscles.
The three nuclei form the accessory nerve, which innervates the muscles that provide movement of the pupil and the area near the eyelashes.
Thanks to the described anatomical features, this formation is responsible for the performance of visual functions and supports some human reflex abilities (in particular, pupil constriction to light and accommodation (adaptation) to changing lighting conditions).
Symptoms and signs of damage
In the early stages of oculomotor nerve paresis, there are practically no symptoms, which complicates its diagnosis and further treatment. With a longer course of the disease, the following symptoms gradually begin to appear:
- Drooping of the upper eyelid (partial or complete);
- Lack of reaction (constriction/dilation) of the pupil;
- Diplopia (double vision due to loss of motor ability of the eye);
- Divergent strabismus (occurs due to lack of resistance of the upper and lower muscles of the eyeball);
- Loss of focusing and adaptation to changes in the distance between the eye and the object;
- Loss of motor ability;
- Protrusion of the eye.
With extensive damage, immobility can become only part of the entire symptomatology of the disease if other cranial nerves are also damaged. In addition, oculomotor nerve palsy itself may be a symptom of a more serious systemic disease. Most often, the lesion affects only one eye.
Types of pathology
In medical practice, there are two main forms of the disease:
- Congenital. Occurs as a result of intrauterine disorders of the development of muscles and nerves, as well as damage or damage to the facial and oculomotor nerves during development;
- Acquired. May have neurological, mechanical (traumatic injuries, consequences of surgical operations), aponeurotic prerequisites.
Paresis also occurs as a result of the progression of systemic diseases. In such cases, therapy should be aimed not only at eliminating paralysis, but also at relieving its causes.
Causes, prerequisites and risk factors for damage
Systemic pathologies that can cause paresis and paralysis:
- Diabetes;
- Arterial hypertension, instability of blood pressure;
- Benign tumors and oncology;
- Cervical osteochondrosis and other diseases of the spine;
- Aneurysm;
- Long-term use of Amiodarone, anticancer drugs and medications for the treatment of cardiovascular diseases;
- Hematomas;
- Traumatic eye injuries, foreign body entry;
- Inflammatory diseases of the brain (encephalitis, meningitis);
- Ophthalmoplegic migraine;
- Flu;
- Diphtheria;
- Syphilis;
- Brain hemorrhage, stroke;
- Vasculitis;
- Myocardial infarction.
The presence of at least one of the listed diseases is a reason for a systematic medical examination with a mandatory examination by a neurologist and ophthalmologist.
Therapeutic methods
One of the most important measures in the treatment of oculomotor nerve palsy is constant monitoring of the patient. In this case, a therapeutic effect on the root cause of paralysis is mandatory. If intervention is unavoidable, the doctor selects one of the more radical methods.
Computer program
The main task of the computer program is to strengthen the muscles of the eyeball during the broadcast of special pictures. When viewing, patients experience increased nerve tension, due to which the body’s resources are mobilized and directed to improve their functioning. With systematic sessions, positive dynamics of treatment are observed.
Electrophoresis
Electrophoresis also gives good results of therapy. Before the session, electrodes are applied to the patient's closed eyes around the perimeter, as well as to the back of the head. The course of treatment consists of 15-20 sessions, the duration of which is no more than 20 minutes.
Adjuvant therapy
Drug treatment in relieving paresis is ineffective. At the same time, to improve the patient’s condition, special eye drops that improve blood supply and tissue nutrition, physical therapy, and vitamin complexes can be used. Patients are also prescribed wearing bandages, sessions of viewing stereo images, proper rest and nutrition.
Preventive measures
In order to prevent congenital anomalies of the visual system, a pregnant woman must follow the prescribed regimen and undergo routine examinations by the attending physician and ultrasound examinations. To prevent acquired lesions, it is necessary:
- Observe safety precautions at work;
- Avoid traumatic situations;
- Avoid complications in the event of infectious diseases;
- Systematically undergo examinations by an ophthalmologist (at least once a year);
- Monitor and promptly treat systemic diseases.
If you experience discomfort, pain, or deterioration in focusing, you should consult a doctor as soon as possible. A positive treatment outcome is possible if the disease is detected only in the early stages of its development.
Possible complications and consequences of paresis
As a rule, it is possible to eliminate the pathology within three to six months with timely and correct therapy. First of all, conservative methods are used for this. If no improvement is observed during the specified period, other therapeutic measures are also added. Congenital pathologies, as a rule, cannot be completely cured.
Oculomotor nerve palsy: causes, symptoms, diagnosis, treatment
Vision allows you to see the world around you and navigate space much easier, and a person who begins to experience problems with vision sometimes feels helpless. There are many reasons for vision problems, one of them is oculomotor nerve paresis.
Anatomy of cranial nerves
To understand how damage to the oculomotor nerve occurs and disruption of its functionality, you need to know how all cranial nerves are structured.
There are twelve pairs of cranial nerves in the human body. Each of them has its own number, name and performs a specific function.
Among them there are: olfactory, visual, trigeminal, trochlear, oculomotor, facial, sublingual, accessory, glossopharyngeal, vagus, abducens and vestibulocochlear.
The functionality of most of them is clear by their name, and in this regard it becomes clear what kind of violations a person will have if their work is changed. They all extend from the brain stem, as evidenced by their location.
Functions of the oculomotor nerve
This nerve is considered mixed; before entering the orbit it is divided into two branches. The upper branch, in turn, also divides and goes to the upper eyelid. The lower branch is considered more powerful; these are the so-called infraorbital nerves, which themselves are quite strong and allow innervation of the inferior rectus muscle.
Due to the fact that the nerve is mixed, it consists of different fibers - these are directly motor and parasympathetic. The nuclei of the oculomotor nerves have cell groups that give certain impulses and allow the functionality of this nerve.
Impulses, passing through certain channels, go to the muscles, which allow them to move. For example, one of the parasympathetic nuclei reaches the internal muscles of the eye, these muscles allow you to narrow the pupil. The unpaired nucleus of Perlia allows for normal accommodation of the eyes, this nucleus.
unlike paired eyes, it is common to two eyes at once.
Due to the innervation of four of the six extraocular muscles, a person can move the eyeball, that is, without turning the neck or body, he can see what is on the side. This function includes all movements, including raising, lowering and, if necessary, turning.
The essence of the problem
Understanding how important the work of the oculomotor nerve is, it becomes clear that any damage will affect the patient’s quality of life.
Damage to this nerve can be either complete or partial.
It is quite difficult to determine the disease in its first stages, this is due to the fact that the disease practically does not manifest itself and even during examination additional diagnostic methods may be needed.
It is worth noting that damage to the nuclei of a given nerve in different locations will have different effects and be felt by the patient.
The problem with this pathology is that isolated damage to a cranial nerve is quite rarely observed, this also applies to the oculomotor nerve. Typically, such disorders involve damage to the brain stem, which is a serious problem.
There are quite a few reasons for such a lesion, for example, it could be a previous heart attack, hemorrhages, found tumors or infections that have affected the body. In fact, there are a lot of specific diseases that cause this to happen.
With obvious damage to the oculomotor nerve, the symptoms are noticeable not only to the patient himself, but also to the people around him, because this can cause strabismus and other unpleasant symptoms.
Possible problems
The symptoms of damage to the oculomotor nerve are very diverse, and each individual lesion is accompanied by its own characteristics.
Upper eyelid ptosis
This manifestation of the disease is characterized by drooping of the upper eyelid. This problem can occur in both adults and children and is quite common. Some patients consider this a minor change, but in fact the pathology requires urgent diagnosis.
In addition to the fact that ptosis can be caused by a problem with the oculomotor nerve, there are many other diseases that need to be taken no less seriously. Diagnosis occurs almost immediately if a child is born with such a pathology, but if this change occurs during life, many may not contact specialists for a long time.
This problem may be related to muscle tone, ligaments and nerves. When neurogenic ptosis occurs, it is most often due to abnormalities that have occurred in the oculomotor nerve.
Paralysis develops for various reasons, it can be tumors, diabetic neuropathy, intracranial aneurysm.
With such a lesion, the patient experiences internal ophthalmoplegia, as well as pathology of the extraocular muscles.
There are situations when a person develops a corneal ulcer, then ptosis will become a necessary measure and it is induced artificially; this approach is considered part of the treatment measures.
With a drooping eyelid, this pathology is usually distinguished by the degree of its severity, therefore there are such concepts as partial, incomplete, and complete drooping of the eyelid. The symptoms of this pathology are clearly visible, irritation of the eye occurs, the person needs to make an effort to open the eyelid, sometimes it comes to the point that he has to throw his head back. Possible squint and double vision.
Exotropia
There is another problem that can be caused by oculomotor nerve palsy. Like ptosis, these are not only disorders that affect the functionality of the eye, but also aesthetic changes.
Divergent strabismus is usually divided into two large groups, which, in turn, have subtypes. There are concepts of permanent and periodic divergent strabismus. The permanent may be sensory, innate or secondary. Periodic divergent strabismus is divided into basic, excess of divergence and weakness of convergence.
In addition to the fact that paresis may be the cause, this problem also arises with paralysis, diseases of the central nervous system, all kinds of injuries, including mental ones, as well as due to infectious diseases and developmental anomalies. As a result, it is not always possible to say that it was paresis that caused the pathology.
Symptoms of this problem are noticeable visually, as the person squints slightly in one eye. The direction may be towards the nose, the other eye or temple.
The peculiarities of the manifestation of this pathology and paresis of the oculomotor nerve are that the pupil in most cases is directed outward, and due to the lack of resistance it is slightly lowered.
Also symptoms are a violation of binocular vision, the eye sees worse, but does not lose its former mobility.
Diplopia
In simple words, this pathology is called double vision. The problem is largely considered a manifestation of paralysis of the extraocular muscles, which can also occur with paresis. But as for the latter, this pathology is considered rather subjective for the reason that double vision is not constantly observed, but only when the patient looks with both eyes at once.
There are quite a few reasons for the occurrence of pathology, so the patient will necessarily need to undergo diagnostics to determine the presence of a particular ailment. The main symptoms of this problem are double vision, dizziness, and problems may arise with determining the location of individual objects in space.
Midriaz
With this pathology, an unnatural dilation of the pupil occurs, which increases under the influence of various factors.
One of the reasons for such unnatural expansion may be a violation of the oculomotor nerve. This is because this nerve is part of the reflex arc of the pupillary reflex to light.
In this regard, when the attending physician tries to influence the pupil with light, it does not react in any way.
Other violations
In addition, other abnormalities are observed in cases of oculomotor nerve disorders. A person’s accommodation is impaired, that is, the perception of objects that are at different distances.
Convergence paralysis. When a person examines an object in front of him, he closes his eyeballs and thus can examine all the necessary details. With paresis, this function is impaired, that is, the patient cannot turn the eyeballs inward. Symptoms also occur when the eyeball moves in different directions. A person cannot turn it up, in, down.
Considering the fact that eye movement is carried out due to the movement of three nerves, that is, oculomotor, abducens, and trochlear nerves, disturbances in their functioning will also be noticeable to the patient.
For example, if the movement of the eyeball inward will be almost impossible with paresis of the oculomotor nerve, then when paresis of the abducens nerve occurs, a person will have problems with movement outward.
Diagnostics
Before starting treatment, it is necessary to make sure that paresis is the cause of these symptoms. If only the trochlear and abducens nerves are affected, then such a change rarely becomes a manifestation of serious diseases.
A patient with various visual impairments must first consult a doctor and tell about all the symptoms. Then there will be all sorts of tests from the ophthalmologist, which will show the eye's reaction to light, how the patient can move the eyeballs, as well as his quality of vision. You will need a CT and MRI, but these examinations are not always carried out.
Treatment
The attending physician will tell you how best to treat the disorder, but there are quite common ways to restore the innervation of the eye. Such problems are treated with the help of electrophoresis, the duration of each procedure usually lasts up to 20 minutes, and about 15 sessions are required, they are carried out every day without skipping.
Various physiotherapeutic methods are used that allow impulses to be applied to the affected area. But the negative side of this effect is that some procedures have virtually no positive effect. Treatment with folk remedies is more likely aimed at preventing this disease than at eliminating the problem that has arisen.
If you notice the first symptoms, be sure to consult a doctor, get examined and, if necessary, begin treatment.
Symptoms of damage to the oculomotor nerve
- Ptosis (drooping eyelid);
- Diplopia (double vision) is a phenomenon that occurs when looking at an object with both eyes;
- Exophthalmos (protrusion of the eyeball);
- Divergent strabismus (strabismus is a position of the eyes characterized by non-crossing of the visual axes of both eyes on a fixed object; with divergent strabismus, the squinting eye deviates towards the temple);
- Mydriasis (dilation of the pupil) – lack of reaction of the pupil to light, the pupil on the affected side is dilated;
- Paralysis of accommodation (the ability of the eye to change the refractive power for the ability to clearly see objects at different distances from it), as a result of which the quality of vision at different distances is impaired;
- Convergence disorder (convergence of the visual axes of the eyes in relation to the center), characterized by the inability to fix the gaze on a nearby object;
- Restrictions on the movement of the eyeball (down, up, in);
- Hyperkinesis (tremor, chorea) – pathological rapid involuntary muscle contractions;
- Ataxia (impaired coordination of movements of various muscles).
Asthenopia
A feeling of fatigue that occurs with prolonged visual stress. Asthenopia is caused by wearing incorrectly selected glasses and lenses.
Symptoms:
- Burning and pain.
- Tearing.
- Fatigue.
- Headache.
Treatment as such for asthenopia is not prescribed, but there are preventive measures. These include eye massage, performing a set of exercises during breaks at work, as well as using high-quality equipment in the workplace.