Perimetry
(Greek peri around, around + metreo measure, measure) - a method of studying the visual field (the space simultaneously perceived by the eye with a fixed gaze and a fixed position of the head) using special devices - perimeters. The essence of the method is that the field of view (see) of the eye under study is determined in projection onto a concave spherical surface (arc or hemisphere), concentric to the surface of the retina, by presenting to the patient a test object of a given size, brightness and color at various points of the arc (hemisphere) ) and determining its position relative to the visual axis of the eye. With Perimetry, the gross distortion of the boundaries of the visual field, which is inevitable when projecting it onto a plane, is eliminated (see Campimetry).
Perimetry has been known since the time of Hippocrates (4th century BC). The founder of clinical perimetry is considered to be J. Purkinje (1825). He was the first to use an arc to study the visual field and showed the wedge, the value of P. in eye and neurological diseases. Aubert and Forster (H. Aubert, R. Forster, 1857) improved the Purkinje technique and developed the basic principles of clinical Perimetry. Perimetry and the equipment for its implementation received special development from the beginning of the 19th century. Modern Perimetry methods are of great importance for the diagnosis and prognosis of a number of diseases of the visual analyzer and brain.
Perimetry is used for diseases accompanied by changes in the boundaries of the visual field or focal loss within these boundaries - scotomas (see Scotoma). Such diseases include glaucoma, retinal pigmentary dystrophy, neuritis and optic nerve atrophy, thrombosis of the central retinal vein, as well as various brain lesions: tumor, arachnoiditis, circulatory disorders.
There are two main methods of P.: kinetic P. using a moving test object and static P., in which the test object is motionless.
Indications
Patients are prescribed computer perimetry if certain eye diseases are suspected, including:
- Increased intraocular pressure and glaucoma;
- Inflammation of the optic nerve head;
- Retinal damage and detachment;
- Vascular fundus abnormalities;
- Oncological diseases affecting the eye;
- Organic pathology of the central nervous system (hypertension, hemorrhagic stroke, tumor processes, multiple scerosis).
What diseases does it detect?
The method is used to identify ophthalmological defects and diseases:
dystrophic changes in the retina;- glaucoma;
- pathologies of the visual pathway and cortical centers due to trauma, stroke, development of neoplasms;
- hemorrhages in the retinal area;
- tumors, hemorrhages and inflammatory diseases of the brain.
- malignant neoplasms in the eyes.
Perimetry also helps to identify visual impairment associated with traumatic brain injuries, strokes, hypertension, neuritis, and ischemia.
IMPORTANT! Perimetry is included in the list of mandatory examinations when passing some professional medical examinations. Visual field testing is necessary when applying for a job, when an employee is required to be attentive.
Progress of the procedure
The patient himself is the main sensitive sensor that helps in performing computer perimetry. It is placed near a special eyepiece and fixes the gaze at a luminous central point. He puts his hand on the joystick. Light signals appear in the field around this target point in a chaotic manner and at different time intervals. The patient, seeing this flash, must immediately press the button. After this, the computer processes the data and compares the received signal with the location of the light mark.
Each eye is examined separately, that is, the procedure is repeated twice. The duration of the study does not exceed 20 minutes. During diagnosis, there are no external influences on the eye, so there is no risk of complications or side effects. The patient must be very careful and follow all instructions.
The result of computer processing can be displayed on the screen or printed in the form of a detailed map of the field of view. This information is very useful and valuable for an ophthalmologist.
Static (quantitative, quantitative) perimetry
Static (quantitative, quantitative) perimetry is carried out using a stationary test object, which is presented to the subject at predetermined points of the arc or hemisphere of the perimeter. The brightness of the test object gradually increases from subthreshold to threshold, at which it becomes visible to the patient. The method is highly informative.
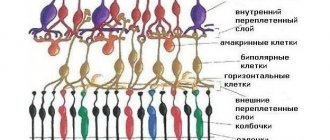
Conditions for performing perimetry. Kinetic and static P. are carried out under conditions of adaptation to different levels of arc illumination (adaptoperimetry): photopic (“daytime”), scotopic (“nighttime”) and mesopic (intermediate) levels. Light levels affect the light sensitivity of the retinal photoreceptors (cones and rods). Thus, under photopic illumination, the most sensitive to light are the cones located in Ch. arr. in the central zone of the retina. P. at this level of illumination makes it possible to identify defects in the central parts of the visual field. Under scotopic illumination, it is most advantageous to examine the peripheral parts of the retina, where under these conditions the sensitivity of the rods is highest. In practice, it is preferable to perform P. under mesopic illumination, that is, under conditions of simultaneous functioning of rods and cones. Color P. must be carried out under photopic illumination, since under these conditions the cone apparatus, which provides color vision, is most active.
Rice. 1. Perimetric form for recording the visual field: dotted lines indicate the normal boundaries of the visual fields of the right eye (dashed line with a dot) and the left eye (dashed line without a dot) when examined using a white test object.
When conducting Perimetry, psychology and preparation of the subject are of great importance. Before P., the patient must be explained the objectives and conditions of the study. Unnecessary irritants (light, noise) must be eliminated. To compare P.'s data obtained by different researchers or in the dynamics of the disease, it is important that P. is carried out under strictly identical conditions. The registration perimetric form (Fig. 1) should indicate the patient’s last name, first name, patronymic, date of examination, size, brightness and color of the test object, illumination of the perimeter arc (hemisphere), and pupil width of the subject.
What can autorefractometry reveal?
Autorefractometry helps detect visual impairments, such as:
- Myopia is an eye disease in which a person sees close objects well, even the smallest ones. In the distance, the picture looks blurry and the further away the object is, the blurrier it is visible. This is due to the elongated eyeball, in which the image arrives in front of the retina rather than through a specific area.
- Farsightedness is a refractive error in which a person sees objects both at a great distance and very close and blurred. The only exception is age-related farsightedness, in which the patient recognizes objects far away. This happens due to a shortened eyeball, in which the image passes not through a certain area of the retina, but into the plane behind it.
- Astigmatism is an ophthalmological disease that damages the cornea and lens. Because of this, a person can see some objects near and far well, but others poorly. The reason for this is the disruption of the spherical surface of the cornea and lens. In its normal state it has an even coating, but with astigmatism its sphericity is disrupted and images are focused in front of the retina, others after, and some in it, as it should be.
According to doctors, about 75% of people suffer from astigmatism, but not everyone pays attention to this, because
it may be quite small. This disease is diagnosed even at an early age. And the sooner correction and treatment begin, the higher the chances of getting rid of the disease.
What is eye pachymetry
Now there are two types of pachymetry in ophthalmology:
- optical;
- ultrasonic
The first option involves non-contact research, but is much less accurate. To conduct the second study, you will need a special ultrasound machine, which will be used to measure the thickness of the cornea. This procedure is called keratopachymetry.
In the case of optical pachymetry, the patient sits in front of a special slit lamp, on which a nozzle made of two plates is installed. It is this attachment that determines the thickness of the cornea in its different places.
Widely used for treatment and diagnosis - eye drops for dilating the pupil.
Autokeratometer with pachymetry function
The ultrasound technique involves contact of the ultrasound machine with the surface of the eye. To ensure that the procedure is painless, the doctor must use local anesthesia. Inocaine is usually used for this. When the anesthesia begins to take effect, the ophthalmologist touches the device to the eye, after which calculations appear on the monitor.
It is extremely important to use the device carefully, as applying too much pressure may cause distorted results. After the procedure has been completed, it is necessary to drip the eyes with moisturizers. This will help avoid irritation
It is very important to remain calm during the procedure as this will reduce the likelihood of corneal injury
This will help avoid irritation. It is very important to remain calm during the procedure as this will reduce the likelihood of corneal injury
After the procedure has been completed, it is necessary to drip the eyes with moisturizers. This will help avoid irritation
It is very important to remain calm during the procedure as this will reduce the likelihood of corneal injury
Ultrasound
When keratotopography is necessary is described in detail in the article.
Decoding the result
Based on the results of the examination, the doctor fills out a special form indicating the extreme points of limitation of the visual field.
The form is deciphered by a specialist, taking into account the following factors when assessing:
- number and size of blind spots;
- scotomas - areas that do not coincide with the periphery;
- the state of the retina in the central region of the visual field.
The interpretation of the examination results is carried out taking into account the individual characteristics of the structure of the visual system, so the interpretation of the readings is done by a doctor, and not by a computer program. The obtained data is combined into a complex, and only after a comparative analysis the state of the patient’s visual field is assessed.
The following indicators are considered normal:
- acceptable scotomas;
- absence of a certain number of areas in the field of view.
The following indicators indicate pathology:
- a large number and expanded blind spots;
- some scotomas are a sign of the onset of glaucoma;
- detection of narrowing of visual fields.
An important factor in assessing the results of perimetry is scotomas. This is the name for discrepancies between the contour and boundaries of the visual periphery. Scotomas can be:
positive – distinguishable by the patient;- negative – detected only during the examination;
- relative - representing a decrease in sensitivity, in which only large and bright objects are detected;
- absolute - in the case of complete loss of all objects from the field of view, regardless of their brightness and size.
By analyzing scotomas, a specialist makes a diagnosis. The detected boundaries of the narrowing of the visual field are considered by the doctor on an individual basis. With normal results, the number of scotomas is small. The presence of scotomas in places of vascular formations is also considered normal; they are called angioscotomas. Detection of other blind spots that do not correspond to the normal indicators is equivalent to deviations.
Graphically, a person’s visual field is represented as a three-dimensional visual hill, the boundaries of which are its base, and the height is the degree of light sensitivity of the retinal sectors. With normal vision, the height of the hill decreases from the center to the periphery.
Norm of peripheral boundaries:
- top – 50°;
- lower – 60°;
- internal – 60°;
- external – less than 90°.
IMPORTANT! Unilateral or bilateral, concentric or sectoral deviations from these indications indicate the development of pathologies. Paracentral scotomas indicate the development of glaucoma.
Advantages of visiting the Sfera clinic
Professor Eskina's clinic has a unique set of equipment that allows for accurate diagnosis and effective treatment. Our ophthalmologists perform perimetry using a modern automatic projection perimeter "AR-7000", manufactured by the Japanese company "Kowa".
It allows you to study the sensitivity of the retina at certain test points with high accuracy. Its advantage is that it is capable of presenting stimuli of different exposures, intensities and colors.
You can make an appointment with our ophthalmologists in Moscow by filling out a simple form on our website or by calling +7 495 139‑09-81.
Why do you need to measure the refraction of the eye?
Each of us has an individual structure of the lens and cornea, the relationship between them, unlike any others, hence the statement that the human optical system is unique. Throughout life, refraction changes and, along with it, the quality of vision. General trends will include:
- newborn babies are farsighted,
- by the age of 20, young people are one third farsighted, and about 40% suffer from myopia, the rest have normal vision,
- Natural aging of the body also affects refraction. Senile farsightedness (myopia) is a very common phenomenon.
Measuring refraction is very important when performing vision correction. It allows you to choose the right glasses and monitor the progress of treatment
This is of particular importance in childhood and adolescence (at this time, vision correction allows you to correct defects and preserve the child’s vision).
It is also important to monitor changes in refraction in old age; diagnostics will help monitor the treatment process or the level of vision loss. Measuring refraction will allow you to plan laser correction and determine its results
Measuring refraction will allow you to plan laser correction and determine its results.
Types of eye refraction
The human eye is very similar in structure to a camera. Light rays pass through the cornea, are refracted, then through the lens and are focused in the center of the retina on the macula (macula). If this is so, then this is the norm and they talk about 100 percent vision (ophthalmologists call it emmetropia). The images perceived at different distances (near and far) are clear and bright, a person sees equally well both in daylight and at dusk.
If the focus, as a result of a defect in the refraction of rays by the lens or cornea, is located in front of the retina (in the area of the vitreous body), they speak of myopia (myopia). With myopia, a person will have difficulty distinguishing objects that are far away and will see relatively clearly those that are close.
If the focus of refraction is behind the retina, then for such a patient close objects will be blurry and indistinct, but those that are far clearer. This type of vision is called hypermetry.
Another type of visual impairment is astigmatism. Here, as a result of the curvature of the sclera or lens, the rays are bent, which distorts the perceived image, causing a loss of clear vision in a certain area. Images may be blurry, unclear, or stretched out.
Myopia, hypermetry and astigmatism require correction and often treatment. In childhood, it is quite possible to preserve vision or even restore it; in old age, a correctly determined refraction will allow for adequate treatment and correction.
Types of diagnostics
The perimetry procedure is absolutely painless and safe for the person being examined; it is quickly performed and has almost no contraindications. The only exceptions are the presence of alcohol or drugs in a person’s blood and existing mental disorders.
Static perimetry
During this examination, a person concentrates his gaze with one eye on a fixed point, placing the chin part of his face on a retractable stand. The doctor will apply a protective bandage to the other organ of vision during the procedure. The ophthalmologist moves objects from the sides of the circle to the center mark at a speed of 20 millimeters per second. The patient's task is as follows: he must give a conventional sign as soon as he begins to observe a moving object. Receiving such a signal from the patient, the doctor records the moment when a moving object appears in the field of view of the subject, as well as the distance. Based on these data, he determines the perimeter of the subject’s visual field.
To set the internal boundaries, an element with dimensions of about one millimeter in length is selected. To clarify the outer perimeter, larger objects are used - at least three millimeters in diameter. Their movement is carried out along different section lines.
Such a diagnostic method requires special attention from the ophthalmologist, and such manipulation usually takes about 30 minutes.
Computer perimetry
Computer eye perimetry is more common today. And to carry it out, an electronic device is used, on which the doctor sets the focus. During the examination, the degree of illumination of the established point changes, but it itself does not move anywhere. As soon as the patient being examined gives the doctor a sign that he has concentrated his gaze on this pixel, the specialist puts the device into operation and different elements begin to be released from the point to the sides, differing from each other only in color. If a person begins to see a previously invisible object with peripheral vision, he presses a special key. After 15 minutes, the ophthalmological perimeter displays the results of the examination in the form of a graph on which the boundaries of the fields are indicated by numerical values.