The cornea is the outer transparent, light-refracting part of the eye, which has a convex shape and is formed by fibrous elements: stroma, anterior limiting and posterior membranes, epithelium and endothelial cells. The cornea is nourished by diffusion through Bowman's membrane, which separates the stroma (the main part of the cornea) from the anterior epithelium. The top layer ensures the delivery of oxygen, regulates the volume of intraocular fluid and protects the cornea from external factors: sunlight, dust particles, chemical components contained in shampoos and other cosmetics.
The normal thickness of the cornea is about 0.6 mm (in the peripheral part - about 1.2 mm). But in some conditions, for example, keratoconus, this indicator may differ significantly from the average values. Treatment and correction of a thin cornea is carried out in various ways, most of which are eye microsurgery methods.
Inflammation of the cornea of the eye
Keratitis is an eye disease that develops as a result of an inflammatory process in the inner sphere of the eye. The disease can affect one eye or both at the same time.
Pathology can manifest itself in people of different age categories. It occurs as a result of injuries, when infection gets on the surface of the eyeball, metabolic disorders, and chronic diseases.
As a result of the development of pathology, clouding of the cornea, redness of the mucous membrane of the eyeball, and increased lacrimation are observed. There is a deterioration in the quality of vision and painful sensations.
The inflammatory process can affect the lower and upper eyelids, cornea, orbit, conjunctiva, and mucous membrane of the eyes. The disease can develop independently, or as a complication of conjunctivitis, blepharitis, dacryocystitis.
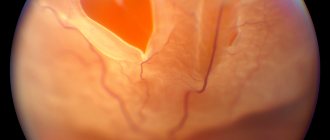
The inflammatory process of the cornea leads to the formation of deep scars. Their formation can cause deterioration in visual acuity and changes in the structure of the eye tissues.
Symptoms of corneal diseases
Diseases of the cornea account for approximately a third of all pathologies of the visual system. Signs of corneal disease, as a rule, are: photophobia, lacrimation, pain, and a general decrease in visual acuity.
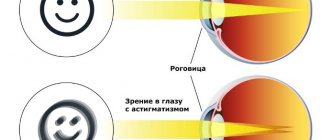
Clinical symptoms of corneal diseases are a violation of the shape, integrity and transparency of the cornea, as well as its refractive power. Here are a few of its types:
- A steeper cornea shape than normal and an increase in refractive power indicate the presence of myopia.
- Flattening of the cornea and a decrease in its optical power is a sign of farsightedness
- Abnormalities in the shape of the cornea in various planes indicate astigmatism
- Thinning of the cornea occurs with the development of keratoconus
- Keratitis is a viral infection that manifests itself as infiltrates in the anterior layers of the cornea.
Keratitis - symptoms of this pathology
The manifestations of the disease depend on the causes of its occurrence. At the initial stages of development, the symptoms do not differ from other infectious ophthalmological diseases. With further development of keratitis, specific symptoms arise that are characteristic of this disease.
Symptoms can be subjective:
- painful sensations;
- photophobia;
- activation of lacrimation;
- sensations of the presence of a foreign object in the eyes, a burning sensation;
- involuntary closing of the eyelids;
- deterioration of visual acuity.
There are obvious changes:
- cloudiness, roughness of the cornea;
- decreased eye shine, swelling and redness;
- the occurrence of ulcers in the eye tissues;
- the appearance of a white spot on the cornea;
- development of purulent foci;
- the appearance of tubercles on the cornea;
Additionally noted:
- swollen lymph nodes;
- headache;
- skin rashes.
With further development of the pathology, tree-like, brush-like blood vessels become visible on the surface of the eyeball. A strong painful spasm in the eye can radiate to the lower and upper jaw and spread to the face. When the face is affected, swelling and redness are observed.
Symptoms of eye keratitis
You can suspect that you have this terrible disease if you have a combination of symptoms such as:
- discomfort turning into pain;
- headache;
- photophobia;
- hyperemia of the sclera;
- blepharospasm (the eyelids close spastically, and it is difficult for the patient to open his eyes);
- increased secretion of tear fluid;
- purulent discharge;
- formation of infiltrate;
- fog before the eyes;
- change in corneal transparency. Its deformation, loss of sensitivity and shine are also possible;
- the appearance of ulcers, erosions;
- decreased visual acuity.
Different forms of keratitis have similar symptoms. In order to determine what exactly caused the disease, you need to consult an ophthalmologist.
Main types of inflammatory processes
Depending on the provoking factors, several types of corneal inflammation are distinguished.
- Fungal. Occurs as a result of a fungal infection. It is difficult to diagnose and treat. The fungal infection penetrates deep into the eye tissues, where medications do not penetrate well.
- Vernal keratoconjunctivitis. Develops in spring. The cause of eye disease is an allergic reaction caused by environmental factors.
- Bacterial. As a result of the penetration of pathogenic microorganisms onto the surface and inside the eyeball, ulcers and scars are formed on the surface of the cornea. The cause of the disease may be an infected eye injury or improper use of contact lenses.
- Onchocerciasis. Occurs due to the development of an allergic reaction. Affects the anterior and posterior parts of the eyeball.
- Creeping ulcer. Develops against the background of severe ulceration of the cornea and purulent inflammation. The disease is characterized by the appearance of a painful syndrome, swelling, redness, and infiltrate formation.
- Non-ulcerative. The inflammatory process occurs when contact lenses are systematically used and pathogenic microorganisms penetrate the surface of the eye.
- Photokeratitis. It is an occupational disease. Develops in people who regularly come into contact with natural or artificial radiation. As a result, damage to the upper membrane of the eyes occurs.
https://medglaza.ru/zabolevaniya/bolezni/vospalenie-rogovitsy.html
Types of keratitis
Depending on the causes of the problems, there are several types of inflammatory processes that cause damage to the cornea of the eye. Treatment will depend solely on what exactly caused the inflammation.
Exogenous factors include fungal infections such as actinomycosis and aspergillosis, bacterial diseases of the eye appendages, and a number of viral problems.
Endogenous causes of the development of keratitis include neurogenic, vitamin deficiency and hypovitaminosis problems. They are also caused by specific infections: syphilis, brucellosis, tuberculosis, malaria and others. But there are also atypical causes: filamentous keratitis, recurrent erosion, rosacea keratitis.
The variety of types and forms of inflammation of the cornea depends on the localization of the process, its cause and stage. A clear classification is necessary to prescribe the most effective treatment for a particular case.
Depending on the degree of damage:
- superficial keratitis – mild degree of damage, the infiltrate resolves without a trace;
- stromal (deep) – leaves opacities of varying degrees, up to a cataract.
Depending on the location of the infiltrate:
- central (the infiltrate is located in the central part of the pupil, on the visual axis, partially or completely blocking the field of view);
- paracentral (the infiltrate is located in the projection area of the iris);
- peripheral (infiltrate is located in the limbus area, does not impede vision).
Keratitis is classified according to several criteria.
If you experience burning or itching in your eye, you should definitely see an ophthalmologist.
In ophthalmology, two types of corneal inflammation are defined:
- Superficial keratitis;
- Deep keratitis.
Superficial keratitis affects only the upper layer of the mucous membrane. This disease does not leave scars and can be treated quite well. Deep keratitis is much more difficult to treat and forms scars on the cornea that reduce vision.
List of eye diseases in humans:
- hereditary problems with the development of the membrane;
- inflammatory processes – keratitis;
- keratectasia - anatomical disturbances in the size and shape of the cornea;
- the beginning of dystrophic or degenerative processes;
- benign and malignant formations;
- receiving various injuries.
Causes of the disease
The development of pathology occurs as a result of exposure to provoking factors. Viral, fungal, and infectious diseases can cause keratitis.
The main causes of infectious diseases:
- pathogenic microorganisms: treponema pallidum, Pseudomonas aeruginosa, tuberculosis bacterium;
- viral diseases: chicken pox, measles, herpes, adenoviruses;
- fungus;
- chlamydia;
- parasites: flatworm, amoebiasis, toxoplasma.
Mechanical factors:
- traumatization;
- burn of the mucous membrane.
Develops against the background of chronic diseases:
- autoimmune diseases: rheumatoid arthritis, periarthritis nodosa;
- deficiency of vitamin A, C, B1, B2;
- allergic reaction to dust, flowering plants, pet hair, household chemicals, medications;
- trigeminal nerve dysfunction;
- metabolic disorders: diabetes, gout;
- weakened immunity.
The development of an inflammatory process of the cornea can occur against the background of various ophthalmological diseases:
- blepharitis;
- conjunctivitis;
- barley;
- meibomite;
- erysipelas;
- eyelid abscess;
- furuncle;
- dacryocystitis;
- canaliculitis.
Failure to follow the rules for using contact lenses can cause keratitis. As a result, damage to the cornea, penetration of dust, bacteria, and infection are observed.
Vitamins, the lack of which impairs vision
Our body needs vitamins for normal functioning. Among them there are those whose lack affects the way we see. It is known, for example, that the absence (or too little amount) of vitamin A can cause deterioration of twilight vision (night blindness). B vitamins and the well-known vitamin C are also necessary for good vision. These vitamins reduce the risk of developing diseases such as cataracts, glaucoma, and in the case of an existing disease, slow down its progression.
Necessary medical diagnosis
If keratitis develops, you should consult an ophthalmologist. He conducts a survey of the patient, a visual examination of the eyes, and determines the level of vision. Using diagnostic methods, he will determine the cause of the pathology and prescribe a course of treatment.
To carry out diagnostics, the patient's eyes are instilled with anesthetic drops.
Their actions are aimed at eliminating painful sensations. They help relax muscles and promote normal eyelid opening.
Effective diagnostic methods include:
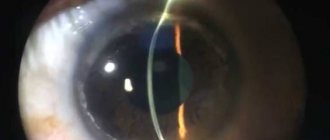
- Biomicroscopy. The eyeball is examined using a slit lamp. The study helps determine the nature and area of corneal damage.
- Ophthalmoscopy. It is carried out to determine the depth of damage to the diseased eye.
- Fluoroscein test. The eyes are instilled with sodium fluorescein solution. Damaged areas of the cornea are painted green. The method helps to determine the presence of ulcers and erosions.
- Bacteriological culture. A smear is taken from the bottom and edge of the ulcer. The result of his study indicates damage to the eyeball by pathogenic microorganisms.
- Allergy test. Helps determine the presence of an allergic reaction of the patient and identify the allergen.
If necessary, an examination is carried out by a pediatrician, gynecologist, urologist, phthisiatrician, venereologist.
How to preserve vitamins in foods?
How to make sure that the eye receives everything it needs and copes with visual loads? Firstly, you need to ensure that your diet is balanced. Please note that vitamins are destroyed when heated (this especially applies to vitamins B2 and C). Therefore, in order to preserve the vitamins and vegetables that contain them, it is recommended not to boil them, but to pour boiling water over them and then wrap them up. However, if you boil them, keep the boiling time as short as possible. Secondly, the necessary vitamins can be obtained by taking special vitamin complexes.
For many of us, the second way is simpler and more accessible. Remember that you should not get carried away with taking one of the vitamins in large quantities without first consulting a doctor.
Possible complications and consequences
Without treatment, keratitis can be accompanied by complications. The development of the inflammatory process leads to the appearance of scars. Accompanied by clouding of the cornea and deterioration in the quality of vision. Inflammation can affect the vascular network of the eyeball. Subsequently, secondary glaucoma develops.
The amoebic form of keratitis is difficult to treat with medication, as it damages not only the cornea, but also the deep eye tissues. The progression of the pathology leads to complete loss of vision.
Complications of the disease include:
- formation of a cataract on the affected eye;
- corneal abscess;
- purulent formations in the anterior eye chamber;
- development of inflammation on the conjunctiva, iris, sclera, ciliary body;
- purulent damage to all structures of the eyeball;
- hernia of Descemet's membrane;
- glaucoma.
Keratitis is often mistaken for conjunctivitis. Improper treatment of the disease can cause a sudden deterioration in visual acuity and blindness.
Comprehensive treatment of the disease
Therapy consists of complex drug treatment in a hospital setting:
- Detoxification therapy. It consists of removing intoxication and cleansing the body. During treatment, drinking plenty of fluids is recommended.
- Systemic therapy. Depending on the causes of the disease, a course of antibiotics, antifungal, antiparasitic, antituberculosis, and antiallergenic drugs is prescribed. Injections of Aloe Extract will help prevent corneal clouding. A course of multivitamins will help strengthen the immune system and eliminate vitamin deficiency.
- Local treatment. To localize the inflammatory process, eye drops, ointments, and gels are used. Their action is aimed at eliminating inflammation and neutralizing the source of infection.
- Physiotherapy. Physiotherapeutic procedures will help speed up the process of recovery and healing of the cornea: magnetotherapy, phonophoresis, electrophoresis.
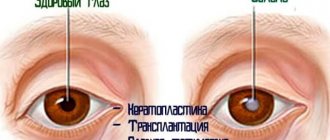
In case of severe damage to the cornea, additional treatment methods are used: cryoapplication, laser coagulation, diathermocoagulation. If keratitis does not respond to drug treatment, they resort to surgical intervention: keratoplasty, replacing the damaged cornea with an artificial one.
Alternative therapy methods
Some experts approve of the use of non-standard methods of therapy at the initial stage of development of keratitis. This allows us to reduce the negative impact of medications on the human body. In more severe forms of the disease, a combination of traditional medicine with conservative methods is permissible.
1. Corneal crosslinking is a surgical intervention that eliminates keratonus. During the procedure, the doctor cuts off the top layer of the cornea, then the eyes are irradiated with ultraviolet light and treated with antibacterial drops. Over the next 3 days after the operation, it is important to constantly wear special lenses.
2. Keratectomy - removal of small opacities in the central region of the cornea. Surgery is used, and in some cases laser treatment of the cornea is used. The formed defect heals on its own after the operation.
3. Keratoplasty (cornea transplant) is used for:
- problems with corneal transparency;
- presence of astigmatism;
- eye injury, acute keratoconus and keratitis;
- to strengthen the corneal tissue and improve the condition of the eyes in preparation for optical keratoplasty.
Folk remedies
In combination with drug treatment, traditional methods are used; herbal medicines include natural ingredients that have antibacterial, septic, and anti-inflammatory effects:
- To prepare the product, you need to wrap 2 aloe leaves in a piece of paper and put them in the refrigerator for 1 week. Then squeeze the juice from the plant and add 1 mummy tablet. The finished medicine is dripped onto the mucous membrane of the eye twice a day.
- Instillation of sea buckthorn oil will help eliminate photophobia. It is necessary to instill eye drops for a week, two drops every hour. Then the time interval between procedures is increased to 4 hours.
- White clay lotions will help speed up the healing process. You need to apply clay to a damp cloth and place it first on the back of your head, then on your forehead and sore eyes. The duration of the procedure is 3 hours, the frequency is 2-3 times a day.
- A herbal decoction compress will help relieve inflammation. To prepare it, you need to chop and mix a spoonful of yarrow, tea rose, and bay leaf. Pour a glass of boiling water over the herbal mixture and leave for 1 hour. The eyes are washed with the prepared solution 4-5 times a day.
Before using folk remedies, you should consult your doctor. You should not self-medicate, as this may worsen the disease.
How to properly treat eye keratitis at home
Treatment of any form of eye keratitis directly depends on the cause of the inflammatory process. Only a doctor can make a correct and accurate diagnosis and, accordingly, prescribe appropriate treatment. Therefore, at the slightest sign, immediately contact a specialist. But is it possible to cure keratitis?
The sooner you start treating keratitis, the fewer complications people will have after this disease. In the case of a long-term process, if keratitis does not go away for a long time, it is possible to prescribe additional examination and surgery to replace the retina. There are completely curable forms and partially transferred to the remission stage - it all depends on the cause and the possibility of its elimination.
How long it takes to treat eye keratitis depends on the cause. From a couple of weeks to months and even several years. To speed up the process as much as possible, you need to consult an ophthalmologist in time and strictly follow all doctor’s prescriptions.
Drug treatment
Traditional therapy includes a general treatment regimen and etiotropic (causal) one. Different types of root causes and pathogens imply different treatment regimens and medications.
Etiotropic treatment:
1. Bacterial cause - antibiotics are prescribed in the form of eye drops or tablets for keratitis caused by pathogenic microflora:
- Levomycetin;
- Phloxal;
- Gentamicin;
- Tobrex;
- Tsipromed;
- Erythromycin;
- tetracycline ointment;
- antiseptic solutions (furacilin, chlorhexidine).
2. Viral keratitis - antiviral drugs:
- Interferon;
- Immunoglobulin;
- Zirgan;
- Zovirax;
- Florenal;
- Oftalmoferon.
3. For the fungal form, the following is prescribed:
- Fluconazole;
- Natamycin;
- Triazole;
- Amphotericin.
4. For severe ulcerative keratitis:
- Kanamycin;
- Lincomycin;
- Neomycin;
- Monomycin;
- Streptomycin-potassium chloride complex;
- Olethetrin.
General treatment plan:
1. Mydriatics are drugs that affect the constriction and dilation of the pupil. Used to prevent scarring and fusion:
- Cyclomed;
- Atropine;
- Adrenalin;
- Scopolamine;
- Tropicamide.
2. Painkillers:
- Quinine;
- Morphine;
- Diphthal.
3. Steroid anti-inflammatory:
- Hydrocortisone;
- Dexamethasone.
4. Regenerating agents:
- Actovegin;
- Kornegel.
5. A course of multivitamin complexes:
- Decamevit;
- Supradin.
6. To reduce intraocular pressure during swelling:
- Diacarb;
- Pilocarpine.
All medications, as well as the regimen for their use, must be prescribed by a doctor; do not self-medicate.
Folk remedies
Traditional treatment of keratitis in combination with folk remedies will help get rid of the pathology at home. Be sure to discuss all methods with your eye doctor.
Folk remedies:
- Treatment with sea buckthorn oil. Effective for meibomian keratitis, when the secretion of the sebaceous gland is disrupted.
- A decoction of eyebright herb is drunk three times a day. To do this, pour 5 tablespoons of dry eyebright with a liter of boiling water and let it brew.
- Honey is a natural antiseptic. Dilute in water 1:2 and use as eye drops.
- Decoctions of chamomile, calendula, sweet clover, and birch leaves are used for eye washes and warm lotions.
- Aloe juice is effective as a sorbent; it draws out inflammation.
- For viral keratitis, instill 1% aqueous tincture of propolis.
Prevention to prevent symptoms
You can speed up the healing process and prevent the development of the disease with the help of preventive measures.
The main preventive measures include:
- Maintaining hygiene rules. After walking, visiting public places, or contacting pets, you must wash your hands. Contact of dirty hands with eyes should be avoided. It is not recommended to have contact with sick people.
- Correct use of contact lenses. When wearing lenses for vision correction, you should follow your doctor's recommendations. Store lenses in a special container with liquid, do not wear them for more than 5 hours and after the expiration date.
- Compliance with safety regulations. When working with dust, shavings, chemicals, or in bright lighting, personal protective equipment should be used. When working at the computer for a long time, wear safety glasses and take short breaks.
- Treatment of eye diseases. Keratitis can develop against the background of other eye diseases.
- Therapy of chronic diseases. It is necessary to promptly treat viral, colds, infectious, fungal diseases, and chronic pathologies of internal organs. This will help avoid complications such as inflammation of the cornea and damage to other organs.
- Avoiding eyeball injuries.
- Strengthening the immune system. Exercising, walking in the fresh air, and swimming help strengthen the body's protective functions. A balanced diet will help eliminate vitamin and mineral deficiencies.
Keratitis is an eye disease that occurs both independently and against the background of other pathologies. Treatment consists of the complex use of traditional therapy and folk methods. Before starting, you should consult an ophthalmologist.
Keratitis: what is it?
The cornea is a very strong, transparent shell of the eyeball that protects the iris, pupil and lens. It consists of five layers, depending on the damage to a particular layer, one can judge the consequences of scarring, as well as the transparency of the resulting stain.
Inflammation of the cornea of the eye occurs with the formation and accumulation of an infiltrate, in which cells of the immune system fight the source of inflammation. Leukocytes, antibodies, and lymphocytes are released from the bloodstream, which are opaque; they determine the color of the infiltrate.
As a result of the pathological process, corneal ulcerative formations appear, which are manifested by acute pain, since the membrane is saturated with nerve endings. If the inflammation is located within the first, outermost epithelial membrane and treatment occurs on time, the transparency of the cornea of the eye is not impaired. This layer is prone to rapid regeneration.
The more advanced the process, the deeper and more dangerous it becomes. The ulcers begin to scar, forming scars, the infiltrate thickens, smoothly flowing into a spot, which has three outcomes:
- A cloud is a transparent, slightly foggy formation.
- The spot is a translucent formation.
- A thorn is an aggressive, opaque formation.
Inflammation can spread to the internal structures of the eye, to the iris or lens, depending on what is the causative agent. Keratitis in children occurs in the same way, only all the symptoms are more pronounced. There is significant redness of the eye, the entire vascular network is clearly visible, this is explained by the need to increase blood supply at the site of inflammation to transport protective cells.
Superficial edge view
A disease accompanied by inflammation of the cornea of the eye is one of the complications after diseases of the eyelids or mucous membrane of the eyes. During the course of the disease, the nutrition of the cornea is disrupted due to compression by swollen eyelids.
Infiltrates (formations from parts of blood and lymph cells) appear as a result of damage to the eye and the penetration of microorganisms into the wound. They tend to resolve, as does slight clouding of the cornea.
Ulcers that form at the site of infiltrates may also disappear over time. With insufficient treatment, ulcers can transform into one large one, and in this case the process of treatment and recovery is delayed.
Stages of keratitis
The first sign of the onset of the inflammatory process is the appearance of infiltrates. The normally transparent and smooth shell becomes rough and cloudy. At the same time, its sensitivity decreases. Within a few days, vessels grow into the resulting infiltrate.
At the second stage, erosion of the cornea of the eye begins, and tissue necrosis begins in the central part of the infiltrate. The emerging ulcer may be located only in the area of the primary lesion, but there are situations when it can damage the entire protective shell in a few hours.
Having passed into the third stage, inflammation of the cornea of the eye begins to regress. During the process, the ulcer is cleaned, its edges are smoothed, and the bottom is lined with white scar tissue.
Traumatic keratitis
The cause of the disease is non-penetrating trauma to the cornea, foreign body entry into the cornea of the eye, eye contusion, chemical burns, thermal burns, and ultraviolet radiation burns.
Symptoms of the disease:
- during the course of the disease, vessels grow into the cornea;
- in the case of superficial traumatic keratitis, dichotomous branching of vessels is observed;
- in the case of deep traumatic keratitis, the branching of the vessels is direct with germination into the cornea;
- erosion forms on the cornea of the eye, accompanied by pain and lacrimation;
- twitching of the upper eyelid is observed.
Treatment in children
The most dangerous consequences and severe treatment of inflammation of the iris caused by gonococcus. A child becomes infected during natural childbirth from a mother with gonorrhea, or the infection is introduced into the eyes later, while caring for the baby without observing the rules of personal hygiene. But how herpetic keratitis is treated will help you understand the information in the link.
The disease manifests itself on the second or third day after birth with swelling of the eyelids and purulent discharge from the eyes. The eyelids are closed, it is difficult even for a doctor to open them. After a confirmed diagnosis, therapy is carried out in a hospital.
Treatment is complex, with the use of antibiotics and strict adherence to all doctor’s prescriptions. If the cause of inflammation is chlamydia, transmitted to the child from the mother or through the dirty hands of others, antibiotics and specific drugs are also prescribed.
Treatment is carried out in a hospital under the supervision of doctors. Untimely cessation or ineffective treatment threatens a recurrence of exacerbation of the disease and serious consequences, including the child’s blindness. Inflammation caused by viruses often occurs after acute respiratory viral infections.
No specific treatment is prescribed; antiseptic eye treatment is sufficient. It is also important to maintain and enhance immunity. The disease goes away after 2 weeks without consequences. The exception is the herpes virus. If keratitis is caused by it, then specific treatment is prescribed using antiviral drugs.
Treatment of keratitis
There are several main types of keratitis:
- Viral. In most cases, it is caused by the herpes virus entering the eye. It is characterized by the appearance of all typical symptoms in a pronounced form.
- Bacterial. This type is not so noticeable in the early stages of development, but is more common, especially among those who use contact lenses (due to non-compliance with preventive measures and hygiene).
- Fungal. One of the most dangerous forms, in which perforation and ulceration of the cornea is observed.
- Amebic. It is caused by the protozoan Acanthamoeba and requires immediate treatment, as in its advanced form it can lead to loss of vision. Characterized by a large amount of infiltrate.
- Also, a large amount of infiltrate is observed with purulent keratitis. Treatment for this type of disease is long and difficult, all the symptoms of the disease manifest themselves most clearly.
Sometimes inflammation of the cornea of the eye occurs due to exposure to sunlight. This is photokeratitis, in which purulent discharge may be present in small quantities.
Treatment of herpetic keratitis
Basically, treatment of this form occurs in a hospital setting, since these procedures require supervision by doctors.
Antiviral medications (Valacyclovir, Acyclovir, Idoxuridine) are usually used.
Herpetic keratitis is treated with electrophoresis. Under the influence of current, the processes of destruction of the cornea are stopped. The procedure is performed in several sessions until a new layer of epithelium appears on the cornea.
Treatment of viral keratitis
In such cases, treatment is aimed at eliminating the virus that causes inflammatory processes. Complex antibacterial and antiviral therapy is used. The basis of treatment is the instillation of antiviral drops into the affected eye, injections are also performed, and some types of medications are taken orally by patients.
Viral keratitis is treated with the following medications: gatifloxacin, ofloxacin, levofloxacin, moxifloxacin.
Treatment of fungal keratitis
Fungal keratitis is caused by pathogenic microflora, which under certain conditions leads to the development of inflammatory processes.
Keratitis is a disease that, with the right approach in the initial stages, can be quite easily treated with folk remedies at home.
There are several effective folk recipes.
Decoction of eyebright
Three tablespoons of this plant are poured into 0.5 liters of boiling water and allowed to infuse for six hours, after which the product is filtered and the finished composition is consumed internally three times a day (half a glass).
Eye drops can also be prepared from eyebright: the herb is poured with two hundred grams of water (eyebright is taken in the amount of one teaspoon), after which the mixture is boiled for three minutes.
The product is infused and cooled for three hours, after which it can be instilled into the eyes (drops are instilled at night, three drops are enough).
The doctor determines the disease based on general studies, such as visometry, slit-lamp examination, ophthalmoscopy, keratometry and other manipulations. But identifying a disease does not mean the end of the diagnosis.
It is important for a specialist to understand the cause of the pathology. To do this, additional tests are taken from the patient (blood PCR for the virus, corneal smear, allergy tests), and if necessary, consultations with a neurologist, phthisiatrician, therapist, allergist are prescribed.
In acute cases of the disease, recovery takes place in a hospital setting under the constant supervision of a doctor. When the crisis has passed and the threat of vision loss has subsided, therapy can be completed at home, but still regularly visiting an ophthalmologist.
An insidious disease that is important to begin treating in a timely manner is temporal arteritis.
Treatment is prescribed individually and is usually carried out in several areas:
- General therapy. In case of infection, antibiotics, antiviral, antifungal or antiparasitic drugs are used. If there are common diseases, the main efforts are directed at them.
- Local medicines. Typically, drops or ointments are used on the eyes to reduce discomfort and inflammation, stimulate healing, and provide prevention or treatment of deep organ damage.
- Additional procedures. Physiotherapy (electrophoresis, phonophoresis), laser coagulation can help speed up recovery. Often taking medications is accompanied by support with complex vitamins.
Keratitis, especially of a viral and fungal nature, is quite difficult to treat. Often, an abundance of medications remains ineffective, and procedures are delayed. In no case should you quit therapy halfway or engage in independent experiments, since the development of the disease threatens complications, including complete loss of vision.
There is another modern method - cross-linking, proposed only about 20 years ago. Its essence lies in the treatment of the cornea with UV radiation, which makes it possible to relieve swelling, destroy pathogens, and restore transparency in one session. But the method has its contraindications, and therefore requires prior consultation with a doctor.
Even with successful treatment, a relapse can be followed by periods of exacerbation, with the course of the disease getting worse each time. In extreme and severe cases, the patient may be offered keratoplasty - surgical replacement of the membrane with a graft.
Instructions for using Vitabact eye drops are presented here.
1. Fungal inflammation must be treated with antifungal drugs.
2. Herpetic inflammation - under no circumstances should corticosteroid ointments be used for treatment.
Treatment of eye keratitis must be carried out in a hospital and lasts five days. Continues at home if necessary. If a patient has keratouveitis in parallel with keratitis, the symptoms of the disease can persist for up to several months.
Drug treatment
To achieve a speedy recovery, local and systemic therapy is used.
Systemic therapy necessarily implies:
- taking medications designed to destroy pathogens. For purulent inflammation, antibiotics are prescribed (Ciprofloxacin, Ceftriaxone, Moxifloxacin). For viral nature of keratitis - Acyclovir. Fungal keratitis is treated with Voriconazole, Fluconazole, Itraconazole;
- detoxification measures (droppers with saline or Rheosorbilact, drinking plenty of fluids);
- prescribing antihistamines to reduce swelling (Zyrtec, Zodak, Desloratadine).
Additionally, the patient is prescribed aloe extract to improve the trophism of the affected tissues and multivitamin complexes.
Keratitis of any nature requires local treatment. For this purpose, use:
- eye drops containing antibiotics (Tobrex, Floxal);
- eye drops with an antiseptic (Oftamirin, Okomistin, Albucid), which will not only have a detrimental effect on pathogenic microorganisms, but will also prevent the addition of a secondary infection;
- Okoferon drops, if the cause of the disease is a virus;
- Zovirax (ointment), if the causative agent of keratitis is the chickenpox virus or herpes;
- drops with corticoids (Maxidex, Sofradex, Tobradex), which prevent damage to the deep layers of the cornea;
- ointments or gels that accelerate regeneration processes (Lakropos, Korneregel, Vidisik).
Drug treatment of ocular keratitis is usually supplemented with physiotherapy (phonophoresis, electrophoresis, magnetic therapy).
Parenchymal keratitis requires specific treatment. The first stage is preparation - taking iodine preparations, then administering Bioquinol intramuscularly. The second stage is treatment with penicillin for 14 days. Along with the antibiotic, mydriatics (Atropine, Irifrin, Cyclomed), yellow mercury ointment, dionine solution and corticosteroid drugs are prescribed locally.
Surgery
The indication for surgery is the presence of ulcers on the cornea of the eye. To eliminate tissue defects, modern microsurgery methods are used: laser coagulation and cryoapplication. If a scar has formed, keratoplasty is performed.
In advanced forms of the disease, when the inflammatory process cannot be stopped by conservative methods, they resort to removing the eyeball.
Treatment of keratitis with folk remedies
Traditional medicine suggests treating diseases of the cornea with compresses, lotions, and steam baths.
- To prepare the mixture, you need to boil potatoes “in their jackets” (1 piece), mash them, add one egg yolk. Then add boiled milk until a paste forms. The resulting mixture is applied on a cotton cloth to the closed eye for 20 minutes. Repeat the procedure three times a day.
- You can wash the inflamed organ with a solution of honey at the rate of 1 tsp. per 200 ml of boiled water.
- Sea buckthorn oil helps relieve pain and reduce photophobia. It is recommended to instill 1 drop every hour in the first days of illness, then every 3-4 hours.
- A decoction of eyebright is taken orally. It is prepared like this: 3 tbsp. dry herbs are poured with boiling water and left for 6 hours, then passed through cheesecloth. The prepared solution is stored at a temperature not exceeding 10 degrees. Take 100 ml 2-3 times a day. Course 30 days.
It is important to remember that you should not risk your health and self-medicate! Any therapy should be carried out only under the supervision of a doctor!
When prescribing treatment, the doctor is guided by the cause of the disease. Treatment should be carried out in a specialized hospital. The duration of the course depends on the severity of the disease and can last from two to four weeks. Treatment is mainly medicinal and only for ulcers is surgery or corneal correction using a laser indicated.
To reduce pain, pupil dilation agents and drugs that lower intraocular pressure, as well as local painkillers, are used. For infectious keratitis, antibiotics in the form of drops and ointments, as well as sulfonamide drugs, are indicated.
If the process has gone too far, then antimicrobial drugs may be prescribed orally or by injection. The administration of drugs into the conjunctiva is also indicated.
When treating inflammation of the cornea, vitamins of group “B” and “PP” are mandatory. For viral inflammation, the doctor prescribes treatment with special medications containing interferon, for example Ganfort eye drops.
The allergic form of keratitis is treated with antihistamines in combination with anti-inflammatory drugs. If inflammation of the cornea is a consequence of tuberculosis or hepatitis, then complex treatment is used under the supervision of a doctor of the appropriate specialization.
Physiotherapeutic procedures are used to treat corneal inflammation. Electrophoresis with antibiotics on closed eyelids or using eye baths helps destroy pathogenic microflora.
The course of treatment can last 15-30 procedures. In addition to electrophoresis, magnetic therapy and UHF are used in the treatment of keratitis.
Physiotherapy is not used for purulent keratitis, as well as for general contraindications. Sea buckthorn oil, celandine and aloe are used as folk remedies.
The juice of these plants, when dropped into the eyes, relieves swelling and reduces pain.
If the disease is advanced and ulcerations appear on the cornea, doctors resort to keratoplasty. This surgical operation allows you to restore reduced visual functions.
The use of folk remedies at home is allowed only after consultation with an ophthalmologist. Self-medication can lead to negative consequences.
Before starting therapy, the specialist conducts an examination, during which he identifies the degree of development of the disease and its features. The first thing the doctor does is collect anamnesis. The specialist must know whether the person has recently suffered from infectious diseases. This is necessary to identify the cause of keratitis and prescribe appropriate treatment.
To treat the disease in question, hospital treatment is required. Treatment methods directly depend on the type of disease the patient has.
Types of pathology:
- An inflammatory process provoked by fungal pathogens. Treatment consists of using agents that kill the fungus.
- Inflammation of the cornea of the eye caused by a herpes infection. The use of antiherpetic agents is necessary. The use of corticosteroid medications is prohibited.
- Keratitis caused by a foreign body entering the eye cavity. The foreign object must be removed.
- Bacterial inflammation of the cornea requires antibiotic treatment. Injections, dressings, eye ointments and oral medications are used.
- Pathology accompanying syphilis or tuberculosis requires treatment of the underlying disease.
- Inflammation as a consequence of wearing contact lenses for vision correction. This type of pathology requires the abandonment of lenses.
- Viral keratitis is treated with pharmacological agents with an antiviral effect.
- Allergic inflammation of the cornea involves identifying the allergen and eliminating it.
If there are ulcerative lesions on the surface of the cornea, surgical intervention is performed. The operation is called keratoplasty, but it allows not only to restore the cornea, but also vision.
Surgical treatment is also indicated in cases where conservative methods do not give a positive result within 30 days.
Conservative therapy does not always give positive results. Therefore, patients with progressive pathology of the cornea are offered surgical intervention. There are several surgical treatment methods:
- Corneal crosslinking is an operation designed to treat keratoconus and performed on an outpatient basis. The patient's eyelids are dilated, the eyes are numbed, and the outer epithelium is removed by soaking the underlying corneal layers with riboflavin. Then the eyes are irradiated with ultraviolet light, antibacterial drops are instilled and lenses are put on, which must be worn for three days after cross-linking.
- Keratotomy is an operation performed using a scalpel by making a radial incision into the cornea. As a result, its surface is leveled, which is the purpose of keratotomy.
- Keratoplasty is a tissue transplantation of the stratum corneum to eliminate deformities and injuries, congenital or acquired during life. There is a risk of developing graft disease, which consists of rejection of the transplanted portion of the cornea and a sharp decrease in vision.
The cornea of the eye is an important component of the visual apparatus. When the integrity, shape, thickness and transparency of the cornea are impaired, significant deterioration occurs, and sometimes even complete loss of vision, up to the loss of the eye.
Therefore, if you experience any discomfort in your eyes, consult a doctor immediately. He will help identify the cause of the ailment and prescribe adequate treatment.
With this approach, you will not only maintain the health of your visual organs, but also maintain good visual acuity.
Antibacterial and anti-inflammatory agents:
- Antibacterial drugs can be used for corneal infections after preliminary studies (Torbex, Tsiprolet).
- Topical glucocorticoids are used to suppress inflammation and limit scarring, although inappropriate use can support microbial growth (Sofradex, Maxitrol).
- Systemic immunosuppressive drugs are used for some forms of severe peripheral corneal ulceration and thinning associated with systemic connective tissue damage (Advagraf, Imuran).
1. Artificial tears (“Taufon”, “Artelak”) should not contain potentially toxic (for example, benzalkonium) or preservatives that increase corneal sensitivity (for example, thiomersal).
2. Closing the eyelids is an emergency measure in neuroparalytic and neurotrophic keratopathies, as well as in eyes with persistent epithelial defects.