In every person's eye there is a conjunctiva, which covers the sclera and is washed by tear fluid, which removes foreign particles from the surface of the eye. A healthy mucous membrane of the eye is always transparent and thin. But when the conjunctival membrane grows on the cornea, pterygium develops. This triangular formation, also called the pterygoid hymen, most often grows on the side of the nose. The disease often occurs in residents of countries with a large number of sunny days a year. Ocular pterygium can affect both eyes.
Reasons for the development of pterygium
There is currently no exact list of reasons that trigger the formation of conjunctival growths. However, the risk of developing the disease increases due to the following factors:
- Excessive exposure to naturally occurring ultraviolet radiation on the visual organs.
- Dust in the eyes or irritation for other reasons.
- Exposure to strong winds.
- Heredity.
- Spending a long time at the computer.
- Constant inflammatory processes of the conjunctiva.
Such manifestations cause intensive vascular growth. With their prolonged growth, the volume of epithelial tissue increases. Fibroblasts then penetrate into the cornea, generating connective tissue. All neoplasms become one, which is called pterygium.
Treatment methods
If Pterygium is diagnosed, drug treatment has only an auxiliary effect: it reduces signs of irritation and helps restore the visual organ after surgery.
The radical method of curing pterygium is surgery.
The lack of progression and small size of the pterygium make it possible to refuse treatment. In this case, the growth is removed at the request of the person due to a cosmetic defect.
Surgical removal
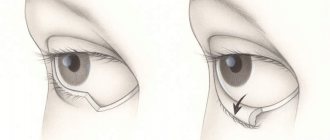
The basis of treatment for the disease is removal of the pterygium. It is performed on an outpatient basis under local anesthesia. Relapses are possible.
Options for removing pterygium using surgical methods:
- The pterygium is replaced with an amniotic membrane or autograft.
- The mucous membrane is sutured to the sclera in the form of a fold.
- The healthy edges of the mucous membrane are connected to each other.
The first two options are the most popular, because they give good results and rarely cause relapses.
The tissues are connected with absorbable suture material or biological glue. After surgery, the eye is covered with an aseptic bandage, which must be changed as it becomes dirty. It can be removed one day after surgery.
In the postoperative period, it is necessary to protect the operated eye from harmful influences. For 2–4 weeks you need to wear sunglasses and instill the prescribed drops. During the week, it is forbidden to wet your eyes (wash your face, swim in bodies of water). It is recommended to avoid physical activity for 2 weeks.
In the video, the professor talks about surgical treatment of the disease.
Laser removal
In modern ophthalmology, preference is given to removing pterygium with a laser. Laser removal causes less trauma to eye tissue and prevents the development of infectious complications. The essence of the operation is the same as with the surgical method, only the surgical instruments are replaced by a laser beam. He excises pathological tissues and seals vessels.
Drug therapy
Medicines are prescribed in the postoperative period to quickly restore the eye and prevent complications. Duration of therapy is 2 weeks.
Local forms of antimicrobial drugs are prescribed to prevent infection, anti-inflammatory drops to relieve redness, moisturizing drops to protect the eye and accelerate healing.
- Antibacterial drops: “Albucid”, “Levomycetin”, “Tobrex”; at night - Tetracycline ointment.
- Anti-inflammatory drops: Diclofenac, Indocollir.
- Moisturizing drops: “Artificial tear”, “Visine”.
Constant exposure to adverse factors on the eye requires the prophylactic use of moisturizing drops.
ethnoscience
It is impossible to get rid of pterygium of the eye using folk remedies alone. Traditional treatment helps relieve symptoms of dryness, irritation, soothes the mucous membrane, and fills it with vitamins.
- Chamomile. Rinsing the eyes with chamomile decoction will relieve inflammatory symptoms. 2 tbsp. l. chamomile pour 200 ml of water. Cook in a water bath for 30 minutes. Warm, strained broth is used to rinse the eyes 3 times a day.
- Tea. Black tea helps reduce eye redness and relieves fatigue. Used for rinsing or compresses. Brew loose leaf black tea, cool, strain from the leaves. Rinse your eyes 3 times a day. It is convenient to use tea bags as a compress.
- Seaweed. Add 3 tbsp to 1 liter of boiling water. l. seaweed, stir, pour into a thermos, let it brew for several hours. Pour the cooled solution into an ice tray. Rub the cubes over your eyelids once a day at night.
- Clay. Mix clay with water, bring to a thick consistency. Form small clay cakes, wrap them in cloth and apply to your eyes. Duration – 1 hour.
It is recommended to drink juices from carrots, beets, and blueberries every day. You can mix them or drink them separately. Eating raw vegetables and berries is beneficial; they are rich in vitamins that are beneficial for the visual organ.
Types of pterygium
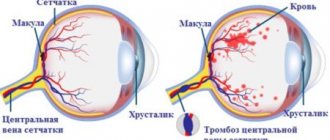
Pterygium can be stationary or progressive. The second of them differs in that the head of the tumor protrudes above the cornea. In this case, the vessels, which are full of blood and twist in different directions, form a complete network. Based on their condition, the degree of progression of the disease is determined:
1st degree. Minimal likelihood of progression. The pterygium has an atrophic and transparent appearance. Through it you can see the vessels of the episclera.
2nd degree. The vessels are poorly visible through the pterygium. The growth protrudes and looks translucent.
3rd degree. The activity of the pterygium increases. It becomes cloudy, making it impossible to see the vessels through it.
Depending on the clinical manifestation, the following stages of pterygium are distinguished:
- At this stage, only the limbus (the area where the cornea and sclera connect) is affected. In this case, the patient does not experience discomfort.
- Between the limbus and the edge of the pupil (in the middle of the distance between them) the head of the pterygium is located. Irregular astegmatism develops before it. A slight degree of regular astigmatism is formed in the optical zone. In this case, vision may decrease to 0.9–0.7.
- The localization of the head of the pterygium changes. Now its location is the edge of the pupil. The cornea thickens, causing vision to drop to 0.5.
- Vision indicators at this stage are 0.3–0.2. Severe astigmatism develops. The head of the pterygium is located in the central corneal region.
- The head of the pterygium extends beyond the center of the cornea and grows further. Vision becomes below 0.1. In this case, a cataract may develop. In some cases, the conjunctiva fuses with the eyelids or lacrimal organs.
Depending on the stage of pterygium, certain signs of the disease are revealed.
The pterygoid hymen can be true (primary) or false (secondary). True pterygium is characterized as a manifestation in older people as a result of negative environmental influences. The cause of the false form of the disease is the formation of scars due to mechanical damage to the conjunctiva (trauma, burns, inflammatory processes). False pterygium does not tend to progress, but its localization is possible in any area of the visual organs.
Classification of pathology
Pterygium can be progressive or stationary. The diagnosis is made based on the condition of the patient’s blood vessels:
- first degree – the formation is transparent and atrophic, progression is minimal;
- second degree – partial viewing of vessels with a protruding formation;
- third degree - the formation is opaque and highly active, the network of vessels is clearly visible.
Symptoms of pterygium
Initially, pterygium does not cause discomfort. Its first stage is expressed as a minor cosmetic defect. As the disease progresses, the following symptoms appear:
- Corneal opacity in the peripheral area.
- A cloudy growth appears on the cornea, which is most often located on the side of the nose.
- Pterygium irritates the nerve endings inside the eyelid. Because of this, there is a feeling of a foreign body in the eye.
- The neoplasm not only lacks the tear film, but also damages the one located in the healthy area of the eye. Because of this, the visual organs become irritated and the patient experiences the symptom of “dry eye”.
- Vision gradually decreases due to impaired penetration of light to the eye receptors.
The inflammatory process with pterygium is accompanied by itching, redness, swelling and abundant secretion of the lacrimal glands.
Diagnosis of pterygium
Pterygium is easy to identify visually. Subsequent studies are aimed at identifying the characteristics of the disease. The following diagnostic methods are used:
- Biomicroscopy. With its help, the size and extent of spread of the tumor is determined.
- Ophthalmoscopy is intended to identify the stage of the disease. Refractometry and visometry pursue the same goals.
- Crystallography. It is a study of tear secretion function in order to identify further spread of the disease and the possibility of its relapse.
- Keratotopography. In this way, the degree of ptyrygium and its shape are determined.
- Fluorescein angiography. Method for identifying vascular changes.
Treatment is prescribed in accordance with the results obtained.
Treatment of pterygium
Conservative and surgical methods are used to treat pterygoid hymen. In the absence of discomfort and changes in visual functions, the tumor is removed only if the patient wishes. In this case, medications are prescribed that replace tears and medications that stop inflammation. The essence of the conservative method is to exclude the possibility of tissue growth to the corneal area. One of the possible schemes for such treatment looks like this:
Only surgery can definitively cure pterygium. In this case, a laser or graft is used. In the first stages, the pterygoid hymen can be removed by exposing the growth to a laser beam. If the disease has spread to such an extent that the membrane of the eye has become severely damaged, the affected area is replaced with a graft. After surgery, antibacterial and anti-inflammatory drugs are used. It is worth noting that surgical intervention can lead to a number of complications. These include the development of infection or diplopia, the formation of scar tissue and graft rejection. Here is a possible clinical picture for pterygium:
It is clear from the commentary that in some cases even surgery cannot guarantee recovery.
Folk remedies against pterygium
The purpose of folk remedies for pterygoid hymen is to reduce symptomatic manifestations. For these purposes, wipe the eyes with brewed tea or chamomile infusion, which help stop the inflammatory process. Clay compresses and herbal drops have an excellent effect. Folk remedies should be used as an addition to the main treatment on the advice of a doctor.
Surgery to remove pterygium
Before deciding on surgery, the ophthalmologist needs to fully see the clinical picture of the disease. Ophthalmic surgery can be called the only effective way to eliminate pterygium today. The pterygoid hymen is cut with a thin blade under local anesthesia. Then the doctor performs conjunctival plastic surgery and applies an aseptic bandage to the eye. The operation takes only 30 minutes and is performed on an outpatient basis. After removal of the pterygium, the area of the cornea remains opaque or translucent.
Prevention of pterygium
Pterygium is very difficult to cure. Therefore, it is better to try to reduce the risk of its development. Prevention of the disease involves following these rules:
- Protect your eyes from exposure to sunlight.
- Follow safety precautions when working with chemicals.
- Try to limit exposure to dust on your eyes.
- Do not touch your eyes with dirty hands to avoid infection.
- Working at the computer should alternate with rest.
If it was not possible to avoid the formation of a hymen, you should immediately consult a doctor.