Causes of the disease
The classification of cataracts is very simple.
There are congenital and acquired thorns. 1. Congenital cataract. The name itself suggests that leukoma in this case occurs in a person even before birth (during intrauterine development). Although the placental barrier is quite reliable, some bacteria and viruses still manage to overcome it. As a result of some inflammatory processes in the fetus, the cornea of the eye is affected.
2. Acquired thorn. This type of leukoma is much more common than the first. The formation of multiple scars often occurs due to keratitis (infectious inflammation of the cornea), as a result of injury or burns. Acquired leukoma on the eye, being a consequence of a corneal ulcer, is combined with thinning of the cornea of the organ of vision, as well as pathologies of intraocular pressure. This type of cataract is called ectatic leukoma (convex). The causes of cataracts can be burns and injuries to the cornea. Alkaline burns are extremely dangerous to vision. After this type of burn, the human eye is only capable of light perception. Types of ocular leukoma also differ in shape: cloud, spot, total lesion and others, depending on the severity of the clouding.
Basically, the cataract develops as a result of certain eye diseases. The cause of this disorder is processes that affect the deep layers of the cornea:
- Keratitis is the most common cause of leukoma because it affects the cornea directly. Keratitis can be superficial or deep. With inadequate treatment, deep keratitis provokes the appearance of a cataract. Superficial ones ulcerate and leave small opacities.
- Injuries. Damage to the cornea and the subsequent appearance of a cataract occurs due to burns of varying severity. Burns occur under the influence of high temperatures and aggressive chemicals (acids, alkalis). Alkali burns are more dangerous than acid burns.
- Diseases of the conjunctiva. Trachoma is a disease that affects the formation of leukoma of the eye. This disease often spreads to the cornea from the conjunctiva.
- Surgical interventions. Even after the simplest eye surgery, complications and injuries can develop, leading to scarring of the cornea and the subsequent formation of leukoma. This may include operations to remove pterygium, cataracts, etc.
- Congenital corneal opacity.
Symptoms and course of the disease
The thorn significantly reduces the quality of life of patients. In some cases, the disease is so severe that the patient loses the ability to see in the affected eye.
Initially, immediately after its appearance, the thorn gives the eye a specific porcelain color. Then, over time, changes occur in the lesion. Fatty tissue degeneration begins, blood vessels grow in, forming a network. Due to the accumulation of fat, the eye becomes yellowish in color.
In addition, in addition to visual impairment, there is a significant cosmetic defect, which can have a serious impact on the patient’s psyche (especially in childhood). In addition, patients often complain of decreased visual acuity and a “fog” appears before their eyes.
The extent of symptoms depends on the size of the lesion and where it is located.
Leukoma
An eyesore or in medical terms “leukoma” is a clouding of the cornea that forms as a result of scar changes. The lesion takes on a porcelain hue and can no longer transmit enough light, which affects the quality of vision. Over time, new vessels grow into the leukoma, and due to its fatty degeneration, the color changes from white to yellow. Typically, an eyesore has an uneven, rough surface. With significant thinning of the cornea, the lesion protrudes.
Leukoma symptoms:
- blurred vision;
- sand effect on mucous membranes;
- redness;
- pain;
- photophobia;
- lacrimation;
- discomfort from a foreign body in the eye.
Based on their shape, lesions are distinguished as spots, clouds, total opacities, and others. Depending on the severity of the cloudiness, there may be a stain or a cataract. The spot has a pearly color and definable boundaries. An eyesore is a late stage of ulceration, which is a scar at the site of the destroyed corneal epithelium.
Types of leukemia
- Congenital. In this case, the thorn is formed even before the person is born. The placenta reliably protects the child even from microorganisms that infect the mother, but sometimes the microbes penetrate the fetus. Inflammation during a child's developmental stage greatly affects the cornea.
- Purchased. Such opacities are much more common. The main reasons for their occurrence: various lesions of the corneal layer and conjunctiva, injuries and burns.
Among acquired leukomas, ectatic (convex) can be distinguished. This is a clouding that appears from ulceration of the cornea against the background of increased pressure inside the eye. The danger of an ectatic cataract lies in the severe thinning of the layers of the cornea.
Symptoms
The congenital form of the disease is often combined with glaucoma, cataracts, iris atrophy and other ophthalmological pathologies. The acquired form of leukoma does not develop immediately, as a complication of a long-term infectious and inflammatory process in the tissues of the eye. Patients complain of decreased vision, increased amount of tear fluid, pain and sensitivity to light. As the disease progresses, visual acuity decreases and the cornea acquires a characteristic milky-white hue.
Causes of cataracts
The main factor in the formation of leukoma is called various processes that change the structure of the layers of the cornea. Sometimes the cause is congenital opacification due to intrauterine inflammation.
Causes of eyesore:
- Keratitis. Inflammation of the cornea, due to its characteristics, is the most common cause of cataract development. Superficial inflammation without treatment turns into an ulcer and leaves only minor opacities, but deep keratitis leads to the formation of a noticeable leukoma.
- Injury. Negative changes in the layers of the cornea appear when the eyeball is burned. This may be the influence of high temperatures, radiation and chemical compounds. The appearance of a cataract is characteristic of an alkali burn, with deep damage to the cornea, when vision turns into light perception.
- Diseases of conjunctivitis. Diseases of the conjunctiva can contribute to the occurrence of leukoma, but trachoma is the main cause in this group. Trachoma is a chronic inflammation of the conjunctiva, which often affects the layers of the cornea, causing scarring of the eye. The cause of inflammation in the conjunctiva is usually the activity of chlamydia.
- Surgical intervention. The appearance of a cataract after surgery indicates that the intervention was carried out with errors, the cornea was injured and scarring began. A similar complication is typical for operations to remove the lens and pterygium.
Patient's recovery prognosis
The prognosis for the development of leukoma depends on the correctness and effectiveness of treatment, the presence of chronic diseases, and the patient’s health status. With timely treatment, the prognosis is favorable.
One hundred percent recovery is observed in patients with infectious leukoma. Modern medicine can not only restore the functioning of the eyeball, but also improve the quality of vision after illness.
In the event of pathology as a result of trauma, burns of various natures, the prognosis depends on the depth and level of damage to the visual organs.
In case of severe damage to the eyeball, protective intraocular lenses are used. Their action helps eliminate the symptoms of the disease, but does not restore vision.
The lack of effective therapy leads to the development of undesirable consequences and complications.
The acquired form of the disease causes thinning of the cornea, resulting in the development of ulceration. A white spot on the eye can provoke the development of complexes and emotional stress not only in children, but also in adults. Often, the absolute lack of therapy leads to complete, irreversible blindness.
Why is an eyesore dangerous?
The effect of leukoma on the functioning of the visual system varies. Most often, corneal clouding is accompanied by partial loss of vision, although sometimes complete blindness is diagnosed. When the cornea is clouded, the preservation of vision depends on the size of the lesion and its location.
The worst option is the location of the leukoma in the center, opposite the pupil. In this case, ophthalmologists recommend removal as quickly as possible to avoid complications. Peripheral opacities have almost no effect on vision. A small eyesore along the edge of the cornea may not appear in any way, so such opacities are most often detected directly in the ophthalmologist’s office.
Complications
The consequences of the disease are associated with the lack of timely treatment, which leads to the progression of leukoma. The patient may develop the following complications:
- deformation of the pupil due to its adhesion to the cataract;
- glaucoma (destruction of the retina due to increased intraocular pressure, which provokes the development of blindness);
- significant decrease in visual acuity;
- spasm of accommodation (impaired functioning of the visual muscles);
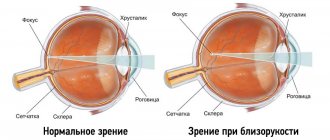
- severe myopia or myopia (poor discrimination of objects located at a far distance);
- strabismus (deviation of one or two eyes from the visual axis);
- nystagmus (uncontrollable eye shaking).
Only timely diagnosis and treatment of the cataract will help prevent the development of complications.
Examination for leukoma
Diagnosis of eye diseases always begins with biomicroscopy and ophthalmoscopy. Biomicroscopy involves external examination of the structures of the eye with a slit lamp. In the light of the lamp, you can see foci of cloudiness on the cornea. During the study, the ophthalmologist determines the characteristics of the leukoma: shape, size, depth of occurrence. Small lesions are detected only during biomicroscopy.
Ophthalmoscopy – examination of the structures of the fundus of the eye using lenses. The study allows you to evaluate the degree of turbidity and the reflex with transmitted light. For a more accurate diagnosis, corneal keratotopography is performed. This is a quick way to map the thickness of the corneal layer and identify any changes. Typically, keratotopography is prescribed to patients with refractive errors and keratoconus, but in the presence of a cataract, the method is also informative.
Diagnostics
An ophthalmologist can establish a preliminary diagnosis during examination of the patient. A whitish spot with a smooth or rough surface, sometimes convex, is visible to the naked eye.
Comprehensive diagnosis of cataracts is aimed at assessing the extent of scar changes and their precise localization. Patients may be prescribed the following techniques:
- Biomicroscopy. Shows the exact location of lesions, their structure, and the depth of tissue damage. It is also possible to determine the size of the cataract and assess its surface.
- Visometry. Assessment of visual acuity. Necessary to determine how pathology affects visual function.
- Keratotopography. A computer diagnostic method that allows you to examine all layers of the cornea and identify even the slightest pathological changes.
- Ophthalmoscopy. Used to determine the stage of advanced disease and the level of transparency of the cornea. Allows you to check fundus reflexes.
Based on the results obtained, the ophthalmologist makes a diagnosis and determines further tactics.
If the slightest defect appears on the visual analyzer, you should make an appointment with a doctor. Early diagnosis will help avoid irreversible consequences.
Treatment of corneal thorn
When treating leukoma, preference is given to surgical methods. This is the most reliable way to restore the functions of the cornea and return the patient to normal vision. Typically, keratoplasty is performed - replacing the damaged area with material from a donor.
Leukomas formed as a result of a burn are treated in different ways. It all depends on the characteristics and severity of the clouding. Severe epithelial destruction and nerve damage require the installation of protective lenses. This measure will not improve vision, but will relieve symptoms.
Medicines and traditional medicine recipes make it possible to reduce discomfort, but leukoma can be cured forever and completely only through surgery. If your leukoma is painful, you may want to talk to your ophthalmologist about using pain-relieving eye drops or traditional medicine before surgery.
Traditional methods of treating cataracts
- The herb eyebright has proven to be very effective in treating corneas. In the case of leukoma, prepare a tincture from which compresses are made: leave a tablespoon of the raw material in boiling water for 60 minutes. It is advisable to choose a porcelain container. After settling, the product is used for cotton or gauze compresses.
- Eyebright can also be prepared for oral administration. The recipe for making the tincture is simple: a teaspoon of herbs in a glass of hot water. The product is infused for 40-50 minutes and taken ¼ cup three times a day with meals.
- For leukoma, you can prepare a tincture of blue cornflower, eyebright, arnica and black elderberry. Mix a teaspoon of each raw material, pour a glass of hot water and leave for 2 hours. Strain the liquid twice using a linen cloth. The tincture is used to make compresses, eye drops, and a means for washing the eye mucosa.
- With a cataract, many people find it helpful to wash it with tincture of cumin and plantain. To prepare it, you need to take a teaspoon of the mixture and pour 250 ml of boiling water. After filtering, wash the eyes with the product several times a day.
Keratoplasty for leukoma
Leukoma can only be cured completely through surgery. During the operation, the patient is transplanted a cornea or part of it from a donor. Operations to transplant layers of the cornea are called keratoplasty; there is a partial or through replacement. The scope of work is determined in advance, taking into account the severity and structure of corneal opacification.
Keratoplasty is performed under local or general anesthesia. The doctor removes the cloudiness and replaces it with part of the donor cornea. To fix the implant, sutures are applied (for a period of 3-16 months).
The risk of rejection of a donor cornea is 20%, although this is a very rough estimate. Repeated transplantation is possible, although the chances of rejection in this case increase. To prevent complications, it is necessary to use various drops and eye ointments. In case of deterioration of vision, redness, pain and photophobia, you should visit an ophthalmologist. Testing is needed even if symptoms appear several months after the intervention.
Complications after keratoplasty:
- failure of sutures;
- infectious lesions;
- cataract;
- retinal disinsertion.
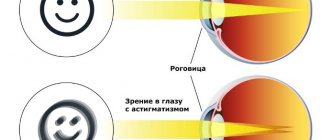
We can talk about the successful outcome of the operation no earlier than in a year. Due to the swelling of the graft, blurred vision remains at first. To help the cornea settle and prevent rejection, steroid drops are prescribed for several months. Sutures can be removed gradually, this helps to avoid astigmatism.
Prognosis and prevention
Timely surgical treatment can eliminate the cataract and restore vision.
Prevention of opacities involves protecting the eyes during potentially hazardous work, as well as proper treatment of inflammation of the cornea and adjacent structures. Any symptoms, even mild ones, should be a reason to contact an ophthalmologist if a person has recently suffered an eye inflammation or a burn.
Sources used:
- Age-related macular degeneration / S.A. Alpatov et al. - M.: GEOTAR-Media, 2010.
- Prevention of low vision and blindness in children / E.I. Kovalevsky. - M.: Medicine, 1991.
- Treatment of eye diseases. Vision correction. Optics / M.V. Kuropatkina. - M.: Ripol Classic, 2011.
- Department of Ophthalmology - University of Colorado
Varieties according to ICD-10 code
schematic drawing of retinal detachment
In ophthalmology, there are 2 forms of the disease: congenital and acquired.
- In the case of the congenital form, the cornea becomes cloudy due to etiopathogenetic factors (they just affect its transparency). The disease can occur due to burns. If you come into contact with chemicals, you need to take care of eye protection!
- If we consider the congenital form, it overtakes children whose bodies have been exposed to viral agents. Babies with congenital cataracts, as a rule, have diseases associated with the functioning of internal organs. More information about methods of treating myopia can be found here.