Features of pathogenesis
Due to a long period of hypertension and pressure, a narrowing of the retinal vessels occurs.
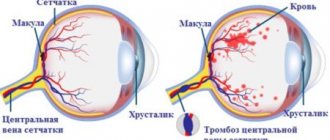
Because of this, blood microcirculation is disrupted, multiple blood clots appear, which close the lumen of the vessels. This all leads to oxygen starvation, as a result of which the retinal vessels of both eyes become fragile, similar to glass. In weak areas, blood vessels rupture and hemorrhage occurs.
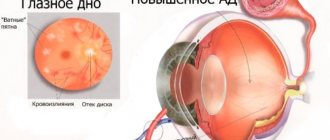
Pathogenesis At first, hypertensive retinopathy does not show any symptoms. When changes in the vessels of the fundus of the eye already occur, they narrow, eye pressure increases (ocular hypertension), patients begin to complain of worsening vision, pain in the eyes.
“Floaters” also appear before the eyes, blurred contours, and certain fields of vision disappear. As hypertensive vascular angiopathy progresses, patients begin to complain of nosebleeds and yellow spots in the eyes, blood in the urine and joint pain.
Symptoms
At the initial stage of development of the disease, there are no obvious manifestations. Unpleasant sensations arise a little later; they consist of deterioration of vision and the flickering of stars or “floaters” in the eyes.
Retinal angiopathy of the hypertensive type begins with changes in the small vessels of the distal retina. Then sclerosis occurs, while their lumen narrows, they become tortuous and in places empty in the arterioles.
These changes are accompanied by symptoms indicating retinal damage: hemorrhage and blurred and poor vision.
What are the features of the disease
Hypertensive angiopathy or angioretinopathy is a pathology affecting small ocular vessels located in the retina. It consists in deformation of the lumens, accompanied by expansion and bending of blood vessels, venous and arterial. Hypertension, which provokes GAS, negatively affects the entire vascular system, so patients usually have damage to both eyes.
Attention!
Hypertensive retinal vascular angiopathy is now diagnosed in very young people. But most often it occurs in patients over 30 years of age and in pregnant women.
Hypertension affects a variety of organs; the eyes are just one of the victims of this common disease. When the visual apparatus is damaged, first of all, its most functional element, the retina, suffers. The main danger of hypertensive angiopathy syndrome is rapid and irreversible loss of vision. According to ICD-10 (international classification of diseases), GAS is not a separate disease, but a background one. ICD code: I79.2*.
Hypertensive retinal angiopathy: what is it?
This term means damage to small vessels located in the fundus of the eye. The cause of the development of the disease is arterial hypertension of various forms. The occurrence of hypertensive retinal angiopathy is often accompanied by deterioration of the patient's vision.
Disease or symptom?
There is debate among modern specialists about whether it is appropriate to say that hypertensive retinal angiopathy is an independent diagnosis. At its core, this pathology does not act as a separate disease, being one of the manifestations of arterial hypertension, just as diabetic angiopathy is a consequence of diabetes mellitus.
This is what hypertensive angiopathy of the retina looks like during examination:
On the other hand, the course of this problem can be so intense that it bothers the patient much more than other manifestations of the body’s disease. Thus, a clear relationship between the progression of hypertension itself and hypertensive angiopathy of the retina has not been established. This means that eye disease can develop both in patients with critically elevated blood pressure and in patients in whom it is slightly elevated.
According to many experts, the explanation for this is the individual structural features of the blood vessels of the eyes. If they have direct anastomoses with large arterial trunks, the risk of developing hypertensive type angiopathy increases sharply. However, this does not mean that hypertension is guaranteed not to cause pathology in the organs of vision in the presence of a scattered type of vascular branching.
Today in medicine it is customary to call hypertensive retinal angiopathy the main diagnosis if its manifestations are most intense compared to other symptoms and the course of hypertension itself. In some cases, patients with this diagnosis receive a disability group. If the clinical picture looks different, retinal angiopathy is regarded as a complication of arterial hypertension.
conclusions
Retinal angiopathy is not an independent disease, which can complicate its treatment program depending on the identified causes. It is not recommended to allow complications and let the situation arise, as this can lead to serious consequences, including complete loss of vision.
The information on the site is presented for informational purposes; be sure to consult an ophthalmologist.
- Tatyana: High degree amblyopia: causes and treatment of the disease What a short period of childhood in which you can still be caught...
- Anastasia: Eye exercises to improve vision - popular exercises Some exercises are not entirely clear how they work, I wanted...
- Masha: How can you improve your vision? If you make sure that your eyes are not overworked, then how can...
- Angelina: Vision table - what tables are there and how are they used to test human vision? Timely diagnosis of any disease is important, not only...
- Maria: Conjunctivitis in a child: symptoms, treatment and prevention Children quite often have conjunctivitis, this happens ...
Causes and mechanism of development
- Individual characteristics of a person - congenital malformations of retinal vessels;
- Smoking;
- Excessive alcohol consumption;
- The presence of various diseases - atherosclerosis, autoimmune pathologies, diabetes mellitus;
- Having excess weight and obesity;
- Exposure to harmful production factors;
- Eating disorders with large amounts of animal fats and fast carbohydrates.
As the disease develops, small formations of the retina - venules and arterioles - may be affected. The process is aggravated by the effects of atherosclerotic vascular damage, which is typical for almost all people suffering from hypertension.
When the structure of large vessels is disrupted, hypertensive macroangiopathy develops.
The development of angiopathy has several stages:
- As a result of increased pressure, retinal vasospasm occurs.
- Atherosclerotic vascular damage progresses.
- After this, inflammation develops and the functioning of the blood coagulation system is disrupted. This leads to the formation of microscopic blood clots that disrupt the nutrition of the retina.
- Due to oxygen starvation, a number of reactions develop, which culminate in vascular hyalinosis. This makes them more fragile.
- In the weakest places of the vessels, hemorrhages and ruptures occur.
Hypertensive retinal angiopathy develops exclusively when blood pressure increases above normal levels. This may be due to hypertension or any symptomatic arterial hypertension. The severity of the pathology is influenced by the following reasons:
- Duration of arterial hypertension;
- Individual features of the structure of blood vessels and the type of their branching;
- The presence of background conditions and diseases: diabetes mellitus, vascular atherosclerosis, intracranial pathology, endocrine diseases;
- Harmful professional conditions that require constant strain on the visual analyzer;
- Toxic influences from the environment.
In people with the same level of increased pressure, even with the same duration of hypertension, the manifestations of retinal angiopathy will have different degrees of severity.
The main links in the mechanism of development of the disease are:
- Spasm (narrowing) of the retinal arteries;
- Progression of atherosclerotic lesions in the vascular wall;
- Accelerated formation of small blood clots;
- Hyalinosis of blood vessels, which leads to persistent and irreversible narrowing (a vessel like a glass tube);
- Angiopathy and fragility of blood vessels, which ends with their frequent ruptures and hemorrhages;
- Disruption of the blood supply to the retina, resulting in its ischemia and destruction of varying degrees.
Arterial hypertension at a young age much more often ends in hypertensive retinal angiopathy.
Often a person develops hypertensive angiopathy of the retina of both eyes at once. The disease progresses slowly. Vascular pathologies provoke a narrowing of the lumen of the arteries, disruption of blood flow. Such changes are visible to a specialist if the fundus of the eye is carefully examined.
Stages
Hypertensive retinal angiopathy, developing and progressing, goes through three stages. As a result of the pathology, the condition of the visual organs worsens, and the vessels and retina are gradually affected.
Stages of retinal angiopathy according to the hypertensive type:
- Functional changes in retinal vessels. Blood circulation in the eyeballs is impaired. The eye arteries expand, and the veins, on the contrary, become narrower. The patient does not experience any discomfort at this stage, the destructive processes pass painlessly. It is impossible to guess the problem; a diagnosis at this stage can only be made by an ophthalmologist during an examination of the fundus.
- Organic change in the retina. This stage is called hypertensive angiosclerosis. There is a change in the structure of the walls of blood vessels - they become denser, preventing normal blood flow.
- Organic damage to the retina and optic nerve. This stage has its own name - hypertensive retinal angioretinopathy. At the final stage, blood circulation is critically impaired. Nutrition does not reach the end points of the ocular system, which is why exudate accumulates in the fundus of the eye, which provokes inflammatory processes in the retina.
Why does the disease occur?
Retinal angiopathy of the hypertensive type is the result of a long-term or chronic increase in blood pressure. In this case, the pressure at which the systolic readings exceed 140 mmHg is considered high. Art. (in some cases, 135 mm), and diastolic values are more than 90 mm Hg. Art.
Thus, there may be many reasons that can influence the development of angiopathy. These are, in particular:
- genetic predisposition;
- excess weight;
- poor nutrition;
- frequent overwork;
- hard physical labor;
- lack of mobility, work that requires prolonged visual strain;
- lack of calcium and magnesium in the body;
- presence of bad habits;
- individual structural features of blood vessels;
- type of vessel branching.
Sometimes hypertension and its consequence hypertensive angiopathy occur due to some other diseases. They can be provoked by pathologies of the central nervous system and disorders of the endocrine system.
If hypertension is not treated promptly, structural changes begin in the walls of blood vessels. Subsequently, blood circulation deteriorates, and some internal organs begin to function poorly. The situation with angiopathy can be complicated by:
- head injuries;
- osteochondrosis (especially of the cervical spine);
- blood and bone marrow diseases;
- heart failure;
- diabetes;
- violation of metabolic processes;
- age-related changes in blood vessels.
External factors that can lead to pathological changes in are:
- harmful working conditions (especially if the work involves welding metal);
- toxic effects from the external environment.
Prevention
The main preventive measure of GAS is blood pressure control. This is especially important for people who have a hereditary tendency to hypertension.
Preventative measures will help prevent the disease:
- do exercises every day; ride a bike, walk, run at an easy pace.
- eat right;
- do not drink alcohol;
- maintain normal weight;
- take vitamins;
- control your psycho-emotional state, avoid stress;
- get plenty of rest and sleep.
There is no need to take any special measures to prevent GAS - the above recommendations should be followed by any person who cares about their health.
Traditional medicine
To treat angiopathy, the following methods are used by healers:
First method
Take 100 grams of St. John's wort, chamomile, yarrow, birch buds, immortelle and mix everything. After this, 1 tablespoon of the mixture is added to half a liter of hot water and left for 20 minutes.
Then strain everything and add water to make half a liter of infusion. Drink 1 glass in the morning on an empty stomach and at night (after drinking a glass of infusion in the evening, you should not eat or drink). Take every day until the entire collection is used.
Second recipe
Stir 1 teaspoon of white mistletoe, already ground into powder, in 250 milliliters of boiling water and leave to steep overnight. Take 2 tablespoons 2 times a day, 3-4 months.
Third way
Take horsetail (20 grams), knotweed (30 grams), 50 grams of hawthorn flowers and mix everything. Then stir 2 teaspoons of the mixture into 250 milliliters of hot water and leave for half an hour. Take 1 tablespoon half an hour before meals 3 times a day for a month.
Regime and nutrition during illness
Patients are recommended to be active and prescribed a diet aimed at maintaining the normal functioning of the retina and reducing the risk of high blood pressure.
Foods with large amounts of carbohydrates, cholesterol and salt are excluded from the diet. The menu is designed in such a way that it is rich in vitamins, minerals and trace elements that are necessary for the retina, blood vessels and the entire body.
Exclude from the diet:
- fat;
- roast;
- salty;
- spicy;
- alcoholic drinks;
- fast food and deep-fried food;
- semi-finished products;
- flour products;
You need to use:
- dairy products;
- fruits and vegetables;
- greenery;
- eggs;
- various types of cereals;
- boiled, baked and steamed meat and fish of low-fat varieties.
- legumes;
- whole wheat bread;
- limit fluid intake.
Treatment of angiopathy is very simple. It comes down to the treatment of hypertension. Photo- and laser coagulation of newly formed vessels have a good effect in neutralizing the consequences of an advanced stage of angiopathy.
Neutron radiation is used experimentally on the hypothalamic-pituitary-adrenal system. Vitamins P, E, hormones, anti-sclerotic agents, oxygen therapy, and anticoagulants also help.
For prevention, you need to monitor the general condition of the body and lead a healthy lifestyle. No specific actions are required for the eyes, since retinal angiopathy is an echo of either a genetic abnormality, trauma, or congenital anomalies and vascular diseases.
One way or another, it is just an echo, a signal to listen to the general state of the body.
How to treat retinal vascular angiopathy
Despite its most serious consequences, GAS is treatable. The sooner it starts, the simpler the treatment, and the higher the chances of cure.
Which doctors should I contact?
Usually the first doctor a patient with angiopathy turns to is a general practitioner. A patient comes to him complaining of feeling unwell and high blood pressure. After examining the patient, the therapist draws appropriate conclusions and refers him to an ophthalmologist for further examination.
If necessary, the patient is prescribed a consultation with a cardiologist. It is usually necessary if the patient has any heart disease. In some cases, you have to seek help from a neurologist.
Medicines
GAS requires comprehensive treatment aimed at treating the underlying causes and consequences of the disease. The main goal of drug therapy is to stabilize blood pressure.
Medications for high blood pressure:
- Capoten or Spirapril - to inhibit the production of renin, which increases blood pressure;
- Atenolol or other β-blockers - to slow the heart rate by lowering distal pressure;
- Hydrocortisone and other diuretics - to remove excess fluid;
- Corinfar and other drugs that increase the lumens in blood vessels.
Treatment of the disease
Retinal angiopathy of the hypertensive type is a very serious disease and often leads to blindness, so you should not try to cure it at home yourself, but you must consult a specialist.
The doctor will conduct a thorough examination and make a diagnosis. As therapy, medications are prescribed that lower blood pressure, anticoagulants and medications that improve metabolic processes in the retina.
A complex of vitamins is also credited. It is imperative that each patient is given dietary nutrition, physiotherapeutic methods and folk remedies therapy.
Treatment of hypertensive retinal angiopathy is primarily aimed at treating the underlying disease, i.e. hypertension.
To improve the condition of the retina, the following is prescribed:
- Vasodilators are vasodilators that act primarily on the vessels of the brain and eye (Cavinton, Xavin, Stugeron);
- To eliminate hypoxia, inhalations with oxygen or carbogen are prescribed;
- To thin the blood and prevent thrombosis, antiplatelet agents are prescribed - acetylsalicylic acid Cardio, Detromb, CardiASK, Klopidex.
- To protect against free radicals - antioxidants - alpha-tocopherol, vitamin C, Veteron, Diquertin;
- Angioprotectors - Doxium;
- For the resorption of hemorrhages - the enzymes Wobenzym and papain.
Only an integrated approach can improve the condition of the retina. Without treatment of the underlying disease, be it hypertension or symptomatic hypertension due to renal pathology, retinal angiopathy will not go away on its own and will only get worse.
Physiotherapeutic methods
Hypertensive angiopathy responds well to physiotherapeutic treatment methods. For this, laser therapy and exposure to a magnetic field are widely used. Laser therapy is based on the use of optical radiation of red and infrared radiation in pulsed or continuous mode.
Benefits of the method This method improves metabolic processes in the affected eye structures, and in combination with drug treatment helps preserve visual functions for a long time. The procedure will help relieve spasms and improve blood microcirculation.
Magnetotherapy is a physiotherapeutic method that is based on the effect of a magnetic field on the eyes. It relieves spasm, swelling, and has a resolving effect. Also, using this method, retinal photoreceptors are stimulated, microcirculation, metabolism and conductivity of retinal cells are improved.
Magnetic therapy is used for degenerative disorders in the retina, inflammation of the optic nerve, diseases of the retinal vessels and increased eye pressure.
Treatment
Therapy is aimed at eliminating the root cause of the pathological condition. If angiopathy occurs against the background of arterial hypertension, the doctor writes a referral to a cardiologist. The doctor prescribes medications that can stabilize blood pressure levels and reduce the risk of bleeding in the retinal vessels and small capillaries.
Diabetic therapy
If angiopathy is associated with diabetes mellitus, then the underlying disease is treated and attempts are made to prevent the development of complications.
The causes and consequences of glaucoma must be taken into account.
So, what medications can an ophthalmologist prescribe:
Cost from 50 rub.
- vasodilators (Cinnarizine, Vinpocetine, etc.);
- vitamin complexes (narrowly targeted drugs, vitamins for the eyes are used).
- drugs that improve blood microcirculation (mainly drops, such as Taufon).
Drops
List of medications that improve blood microcirculation in the eyeballs:
| Name: | Operating principle: |
| Emoxipin | Available in the form of drops, it is used to treat hemorrhages in the cornea. Has a protective function. By class it is considered an angioprotector. |
| Mildronate | Available in capsule form, it helps improve blood circulation and normalize the functioning of the heart and vascular system. Helps to recover after an illness or heavy physical activity. |
| Trental | Available in tablet form, it improves blood microcirculation and is considered a vasodilator. |
About vitamins for age-related farsightedness, which should be used first, is described here.
As a physical therapy, an ophthalmologist may recommend undergoing a course of magnetic therapy or laser treatment (retinal light).
Treatment with folk remedies
As a complement to basic therapy, doctors often recommend the use of alternative medicine. For angiopathy of the vessels of the eye, you can use the following folk remedies:
- Well-washed parsley leaves must be chopped using a blender. The resulting mass should be squeezed out through gauze and the remaining juice should be taken orally 2 times a day, 1 tablespoon.
- take 100 grams of birch buds, immortelle, St. John's wort, chamomile and yarrow, mix. Pour a tablespoon of the resulting herbal mixture with 2 cups of boiling water and leave for 20 minutes. You need to add water to the strained broth so that you get 0.5 liters. Take 1 glass in the morning and evening.
- Add 1 tablespoon of cumin seeds and 1 teaspoon of blue cornflower leaves to a glass of boiling water, boil for 5 minutes. Take the resulting decoction 100 ml 2 times a day.
- Add 1 tablespoon of dill seeds to a glass of boiling water, let the product brew for 1 hour, then take 100 ml of the decoction 3 times a day before meals.
To restore vision in case of retinal angiopathy, it is recommended to take tea from currant leaves or rowan fruits. Nutrition plays an important role in the treatment of pathology.
It is necessary to limit the consumption of easily digestible carbohydrates, fatty and fried foods, and avoid caffeine and animal fats.
Diagnosis of pathology
The complex of examinations for diabetes mellitus includes an annual examination by an ophthalmologist.
If changes in the eyes have already been identified, an examination is carried out every six months. Diagnosis of angiopathy and other eye changes caused by diabetes mellitus does not cause difficulties in most cases. The examination begins with checking visual acuity and tonometry.
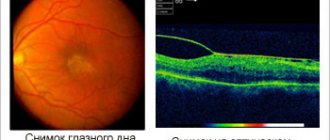
Next, 1-2 drops of midriacil, a special drug that dilates the pupil, are instilled into the conjunctival sac. After 10-15 minutes, when the pupil dilates, an examination is performed at a slit lamp using high-diopter lenses. It is during biomicroscopy under conditions of mydriasis that most changes in the retina and its vessels, hemorrhages, and edema are revealed.
The diagnosis is made by an ophthalmologist after an examination in cases where expansion and darkening of the walls of the venous bed are visible, and their course changes (becomes tortuous).
At the same time, the arterial bed also undergoes changes - the walls of the arterioles become thinner, the lumen narrows. Along the vessels there is often a white stripe - deposition of lymphocytes and blood plasma cells. In the initial stages, such changes often occur in the periphery of the fundus and may be missed when viewed through a narrow pupil.
There is no direct relationship between the stage of the disease and the level of blood sugar and the duration of diabetes. Some patients who have had type I diabetes for more than 20 years and have an average sugar level of 10-12 mmol/l do not experience significant complications. And, on the contrary, patients with low glucose levels of 7-8 mmol/l and a “experience” of the disease of 2-3 years can have severe complications.
In many specialized ophthalmological clinics, photographic recording of the condition of the fundus is carried out to further monitor the dynamics of the disease.
If diabetic macular edema, retinal detachment, or neovascularization is suspected, optical coherence tomography (OCT) is recommended.
This examination method allows you to see the retina in a section, which was impossible for a long time and made it difficult to make a diagnosis and decide on treatment tactics.
Another informative examination method is fluorescein angiography of the retina, which allows you to accurately show the places where blood is leaking from the vessels. This method is recommended after laser coagulation of the retina, as well as in the presence of SUI.
Diabetic angiopathy of the lower extremities: treatment and symptoms
Diabetic angiopathy refers to lesions of large (macroangiopathy) and small (microangiopathy) vessels that occur in patients with diabetes mellitus.
More often, the process involves the brain, visual analyzer, urinary system, heart, and vessels of the lower extremities. Diabetic angiopathy of the lower extremities (ICD-10 code – I79.2*) is one of the most common manifestations of the pathological process. It appears in 70-80% of patients and causes the formation of ulcers, gangrene and forced amputations of the legs. The article discusses the symptoms and treatment of diabetic angiopathy of the lower extremities.
Features of the disease
The development of damage to the circulatory system against the background of diabetes mellitus is accompanied by:
- compaction of vascular walls;
- lipid and cholesterol deposits on the endothelium;
- thrombus formation;
- decrease in vascular lumen;
- formation of swelling and increased exudation;
- disruption of the trophism of cells and tissues up to their death.
Since capillaries have the smallest lumen among all arterial-type vessels, they suffer first. This means that the process of damage begins with the toes, feet, then moves to the legs and reaches the thighs.
Clinical picture
Symptoms of diabetic angiopathy of the lower extremities depend on the course of the pathological process:
- Stage I – there are no visual changes, the patient has no complaints, instrumental and laboratory examinations show the development of an atherosclerotic process in the vessels;
- Stage II - the appearance of the so-called intermittent claudication - a specific symptom that is characterized by the need to stop while walking due to severe pain in the legs, which disappears during rest;
- Stage III – pain syndrome appears even in the absence of load on the legs, requiring constant change of position in bed;
- Stage IV - the formation of painless ulcers and dead areas on the skin due to serious disturbances in the trophism of tissues and cells.
Atherosclerosis is one of the manifestations of diabetic leg angiopathy
Accompanying symptoms characteristic of damage to the blood vessels of the legs in diabetes mellitus:
- feeling of burning, tingling, “goosebumps”;
- formation of spider veins;
- pale skin;
- dry skin, peeling, hair loss;
- brittle toenails;
- development of swelling.
Diabetic foot
One of the most severe complications of leg vascular angiopathy. It can develop in insulin-dependent and non-insulin-dependent types of the disease. It manifests itself as purulent-necrotic processes, the formation of ulcers, and damage to bone and tendon structures. The process involves the innervation system, muscular system, and deep tissues.
Often occurs against the background of the addition of infectious microflora, trauma, or fungal infections. Incorrectly selected shoes and bad habits are common provoking factors of pathology.
Diabetic foot symptoms:
- wounds, ulcerations on the legs due to diabetes mellitus;
- thickening of the nail plates;
- fungal infection on the feet;
- itching;
- pain syndrome;
- lameness or other difficulties encountered while walking;
- change in skin color;
- swelling;
- the appearance of numbness;
- hyperthermia.
Diabetic foot – deep damage to the bone-tendon structures against the background of the “sweet disease”
Diagnostics
With such problems, you can contact an angiosurgeon or endocrinologist. After examination and collection of complaints, the doctor prescribes laboratory, instrumental and hardware assessment of the following indicators:
- biochemical screening – glucose, creatinine, urea levels, blood clotting status;
- ECG, echo CG at rest and with exercise;
- X-ray examination;
- arteriography of the lower extremities - assessment of patency using a contrast agent;
- Dopplerography - ultrasound examination of the condition of blood vessels;
- in the presence of purulent discharge from an ulcer - bacteriological examination with an antibiogram;
- determination of transcutaneous tension - assessment of oxygen levels in the tissues of the extremities;
- computer capillaroscopy.
Important! Diagnostic procedures are carried out not only to make a diagnosis, but also during treatment to assess the condition of the vessels over time.
Features of treatment
The basis of therapy is to maintain blood sugar levels within acceptable limits. The insulin-dependent type of diabetes mellitus requires injections of the pancreatic hormone (insulin) in accordance with a regimen developed by an endocrinologist. It is necessary to observe the injection time, dosage, and conduct self-monitoring using a glucometer.
For type 2 diabetes, hypoglycemic drugs are used:
- Metformin - helps improve the sensitivity of body cells to insulin, increasing the absorption of sugar by tissues. Analogs - Glycon, Siofor.
- Miglitol - inhibits the ability of intestinal enzymes to break down carbohydrates into monosaccharides. The result is no increase in sugar levels. Analog – Diastabol.
- Glibenclamide (Maninil) – promotes the activation of insulin synthesis.
- Amaryl - stimulates the production of a hormonally active substance, which helps reduce the amount of sugar.
- Diabeton - the drug enhances the production of insulin, improves the rheological properties of blood.
Important! At the same time, you need to adhere to a low-carbohydrate diet by adjusting your diet.
Cholesterol-lowering agents
The drugs can be used both as part of therapy and to prevent the development of diabetic angiopathy of the lower extremities. Medicines should be taken with laboratory tests of biochemical blood parameters over time.
| Drug name | Active substance | Features of the action |
| Aterostat | Simvastatin | Reduces cholesterol and lipoprotein levels, contraindicated in renal failure, children, pregnant women |
| Zokor | Simvastatin | Normalizes the amount of triglycerides and total cholesterol levels. Take with caution in cases of liver or kidney pathology, increased levels of transaminases in the blood serum, or alcoholism. |
| Cardiostatin | Lovastatin | Reduces the liver's ability to form cholesterol, thus controlling its level in the blood |
| Lovasterol | Lovastatin | Analog of Cardiostatin. Not used during pregnancy, breastfeeding, severe renal failure |
| Liptonorm | Atorvastatin | Increases the protective mechanisms of the vascular wall, inactivates the process of cholesterol formation |
Antihypertensive drugs
Against the background of a decrease in blood pressure, vasodilation occurs, an antiarrhythmic effect. Blood circulation improves slightly. Products used:
- Nifedipine,
- Corinfar,
- Kordipin,
- Equator,
- Binelol,
- Nebilet.
Corinfar is a representative of a group of medications that lower blood pressure
The mechanism of vasodilation is based on the fact that receptors located in the walls of the arteries and heart are blocked. Some of the drugs can restore heart rhythm.
Angioprotectors
The action of this group of medications is aimed at improving blood supply to the tissues and cells of the body, as well as increasing the resistance of the walls of blood vessels.
- Pentoxifylline (Trental) - the drug helps to dilate blood vessels, improve blood supply, and increase the action of the protective mechanisms of the endothelium.
- Troxevasin – prevents lipid oxidation, has an anti-exudative effect, and stops the development of inflammatory processes.
- Niacin - by dilating blood vessels, the drug helps reduce total cholesterol levels.
- Bilobil - normalizes the permeability of vascular walls, participates in the restoration of metabolic processes.
Antiplatelet agents
The drugs block the biochemical processes of thrombus formation, preventing blockage of the vascular lumen. The following representatives showed effectiveness:
- Aspirin,
- ReoPro,
- Tirofiban,
- Chime,
- Dipyridamole,
- Plavix.
Source: https://sosudy.info/diabeticheskaya-angiopatiya-nizhnih-konechnostey
Diagnosis of fundus changes
An ophthalmologist examines a patient. Conducting a fundus examination is an important step in diagnosing angiopathy. The most popular technique is ophthalmochromoscopy, which allows for the assessment of eye vessels.
They are more difficult to view in red light than in red light. This especially applies to arterial vessels. When a person has hypertension, they narrow, so when examining the eyes in red light, they may not be noticed.
To see the state of blood flow, ultrasound examination of blood vessels may be useful. Doppler helps to assess the changes that have occurred in them.
If angiopathy appears in a child, it must be diagnosed as early as possible, because the disruption of blood flow in the retina is quite active. The characteristic features of the disease can be seen by carefully examining the capillary network of the fundus.
The diagnosis is made after examining the fundus. For this purpose, various options for ophthalmoscopy are performed. The identified changes determine the stage of the process:
- Retinal angiopathy of the hypertensive type in the initial stage - dilatation of venous vessels against the background of narrowed arterioles (4:1 when the norm is 3:2). They become tortuous and branch at an obtuse angle (Gwist's symptom);
- Angiosclerosis is a thickening of the arterial vessels of the retina with loss of elasticity (symptom of copper or silver wire). The result of these changes is angiopathy of the type of compression of veins by arteries;
- Retinopathy is the impregnation of retinal tissue with blood components and minor hemorrhages. They lead to its immediate destruction;
- Neuroretinopathy is the spread of pathological changes from the retina to the optic nerve, which manifests itself in the form of blurred contours and swelling.
If necessary, the following can be performed:
- Doppler ultrasound of eye vessels;
- Fluorescein angiography of the retina;
- Ophthalmodynamometry (measurement of blood pressure in the arteries and veins of the retina;
- Rheoophthalmography (graphic recording of eye blood flow).
These methods make it possible not only to detect vascular disorders, but also to evaluate their precise characteristics, which may be required to draw up a treatment plan.
To make an accurate diagnosis, the doctor must perform a fundus examination. For this purpose, various types of ophthalmoscopy are performed. By identifying abnormal changes, it is possible to determine the stage of development of the pathological process.
The initial stage of hypertensive angiopathy is accompanied by dilation of venous vessels and narrowing of arterioles. They become crimped, and this happens at an obtuse angle.
Diagnosis and diagnosis
Making a diagnosis is not particularly difficult; you just need to contact an ophthalmologist. The doctor will examine the vessels of the fundus.
To detect changes, it is enough to conduct only one examination, but if necessary, the doctor may recommend an ultrasound of the eyes. Intraocular pressure is also measured, which helps eliminate the possibility of developing glaucoma.
The treatment and diagnosis of retinal angiopathy in a child is described in the article.
Classification and causes of pathology development
Since retinal angiopathy is a manifestation of an existing disease, its classification is based precisely on the etiological factor. Taking this into account, pathology is divided into the following types:
- Primary (hypotonic). It is a consequence of the influence of a pathological factor on the vessels of the fundus directly. In infants, this factor may be trauma during childbirth, structural features of blood vessels, or hypoxia. Whereas in adults, the primary form of angiopathy is the result of malfunctions in the vegetative-vascular system (neurocirculatory dystonia), or more precisely, in the mechanism for regulating vascular tone.
- Secondary (background), which, in turn, is divided into:
- diabetic. In this case, the cause is diabetes. Metabolic disorders lead to the accumulation of mucopolysaccharides, which causes the lumen of blood vessels to decrease and blood flow to slow down. As a result, the trophism of eye tissue suffers. At the same time, the walls become thinner and become more permeable, that is, the risk of hemorrhages increases significantly;
dysoric, or Morel's angiopathy. Occurs in people suffering from Alzheimer's disease. The cause of the development of pathology is amyloid deposits on the vascular walls;
- hypertensive or hypertensive retinopathy. As a result of increased pressure, the vessels become branched, the arteries narrow in places, the lumen of the veins expands, and point hemorrhages are observed. In advanced cases, the tissue of the retina and eyeball suffer (it becomes cloudy). All of these vascular changes are reversible provided the pressure level is normalized;
- traumatic. This form most often occurs due to injuries in the cervical spine or brain, in the chest area (with sharp compression). The cause of angiopathy is increased intracranial pressure or compression of blood vessels in the spine;
- youthful. The causes of this pathology of the vascular bed of the fundus, also called Eales disease or proliferating retinitis, have not yet been clarified. Angiopathy develops at a young age and manifests itself in the form of hemorrhages in the retinal tissue and vitreous body, inflammation in the blood vessels. This can lead to glaucoma, cataracts, or even retinal detachment. This form is considered the most difficult to treat;
- mixed. This form is the result of the impact of several pathological factors of different nature on the vessels of the fundus.
Risk factors for the occurrence of pathology are bad habits, old age, and harmful working conditions.
Angiopathy during pregnancy
Due to the fact that during pregnancy the amount of blood in the vessels increases, their walls expand and become weaker - this is where angiopathy begins. GAS is very common in pregnant women; this pathology is especially characteristic of the third trimester. This is a temporary phenomenon that goes away on its own in 90% of cases.
GAS does not depend on the type of birth - the disease occurs both in pregnant women for the first time and in multiparous women. Symptoms usually appear in the 6th month of pregnancy, in 90% of cases - in the 9th month.
Features of GAS in pregnant women:
- Disturbances in the functioning of the retina occur somewhat differently than in other patients. In pregnant women, the arteries usually narrow due to late toxicosis. As soon as it stops, the spasms disappear.
- Pregnant women practically do not experience retinal atherosclerosis and ischemia.
- The prognosis is more favorable than for GAS caused by hypertension.
- There is a danger of miscarriage.
- There is a risk of blood vessels rupturing during contractions. A caesarean section may be recommended.
What is it and the ICD-10 code
Angiopathy does not have a code according to the ICD-10 international classification, since it is not considered an independent disease. The code is assigned to the disease that led to the development of the pathological condition.
Causes and classification
Angiopathy has several causes. The names in the vessels appear against the background of:
- Traumatic injuries to the chest or cervical spine. Which leads to impaired blood flow and hypoxia.
- Arterial hypertension is, simply put, high blood pressure. When blood pressure levels increase, the small capillaries of the retina cannot withstand the load and burst. Hemorrhages occur, which can lead to a decrease in visual acuity, changes in the vessels and their course.
- Arterial hypotension is low blood pressure that occurs against the background of significant dilation of veins and large vessels, leading to the formation of blood clots in the vessels of the retina.
- Cervical osteochondrosis is a disease that leads to impaired blood flow to the brain and increased intracranial pressure.
- Diabetes mellitus is a pathology of the endocrine system, characterized by increased blood sugar levels. In the absence of adequate therapy, diabetes mellitus leads to thickening of the membrane walls and affects the condition of the retinal vascular network.
- Traumatic brain injury - leads to disruption of brain function, increased intracranial pressure, and the development of hypoxia. In this case, angiopathy occurs as a consequence of the injury.
- Pregnancy and childbirth - changes in blood vessels can appear during pregnancy or occur after a difficult birth. In this case, the condition is subject to correction, but only if the cause of the pathology has been established.
- Autoimmune diseases and diseases of the hematopoietic system are nonspecific causes. Against the background of such diseases, changes in the retinal vessels occur quite rarely.
What is presbyopia in this material?
The video shows a description of the disease:
There are several types of angiopathy, it happens:
- hypertensive—occurs when blood pressure or intracranial pressure increases;
- hypotonic – develops against the background of low blood pressure and blood clots;
- diabetic - the main cause is diabetes mellitus or an increase in blood sugar levels (can be diagnosed in children of the first year of life or newborns);
- background – occurs against the background of changes in the condition of the vessels of the retina of the eyes, with a long course it is dangerous for complications;
- traumatic – a consequence of injuries suffered, injuries that occur when blood flow to the brain is disrupted;
- juvenile - appears in children during puberty. The exact cause has not been established. It manifests itself as a sharp loss of visual acuity, develops quickly and can cause glaucoma or retinal dystrophy.
Angiopathy of both eyes is diagnosed more often. But there are cases when the vessels change in only one eyeball. This may indicate a slow progression of the pathology.
Another pathology is hypertensive angiopathy of the retina of both eyes.
Other retinal diseases (H35)
H35.0 Background retinopathy and retinal vascular changes
Changes in the retinal vascular pattern Retinal. microaneurysms. neovascularization. perivasculitis. varicose veins
vascular sheaths. vasculitis Retinopathy. NOS. background NOS. Coates. exudative. hypertensive
Proliferative vitreoretinopathy Excludes: proliferative vitreoretinopathy with retinal detachment (H33.4)
H35.3 Macular and posterior pole degeneration
Angioid stripes {amp}gt; Cyst {amp}gt; Drusen (degenerative) {amp}gt; Macula Hole {amp}gt; Wrinkling {amp}gt; Quonta-Junius degeneration Senile macular degeneration (atrophic) (exudative) Toxic maculopathy If it is necessary to identify the drug causing the lesion, use an additional external cause code (Class XX).
H35.4 Peripheral retinal degenerations
Retinal degeneration. NOS. lattice. microcystic. palisade. resembling a cobblestone street in appearance. reticular Excludes: with retinal break (H33.3)
H35.5 Hereditary retinal dystrophies
Dystrophy. retinal (albipunctate) (pigmented) (yolk-like). tapetoretinal. vitreoretinal Retinitis pigmentosa Stargardt disease
H35.6 Retinal hemorrhage
H35.7 Retinal layer splitting
Central serous chorioretinopathy Detachment of the retinal pigment epithelium
H35.8 Other specified retinal disorders
H35.9 Retinal disease, unspecified
Changes in the retinal vascular pattern
Retinal:
- microaneurysms
- neovascularization
- perivasculitis
- varicose veins
- vascular sheaths
- vasculitis
Excludes: proliferative vitreoretinopathy with retinal detachment (H33.4)
Angioid stripes of the macula
Drusen (degenerative) macula
Age-related macular degeneration (atrophic) (exudative)
If it is necessary to identify the drug that caused the lesion, use an additional external cause code (class XX).
Retinal degeneration:
- NOS
- lattice
- microcystic
- palisade
- resembling a cobblestone street in appearance
- reticular
Excludes: with retinal tear (H33.3)
Central serous chorioretinopathy
Detachment of the retinal pigment epithelium
In Russia, the International Classification of Diseases, 10th revision (ICD-10) has been adopted as a single normative document for recording morbidity, reasons for the population's visits to medical institutions of all departments, and causes of death.
ICD-10 was introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. No. 170
The release of a new revision (ICD-11) is planned by WHO in 2017-2018.
With changes and additions from WHO.
Dystrophy:
- retinal (albipunctate) (pigmented) (yolk-like)
- taperetinal
- vitreoretinal
Symptoms
The initial stage of development of any form of retinal angiopathy is not accompanied by severe symptoms, which makes timely diagnosis of the problem difficult. Primary signs that may indicate the presence of pathology include:
- blurred visible image;
- flashing “flies” before the eyes;
- short-term darkening;
- deterioration of near visual acuity.
As the disease progresses, the patient may complain of the following symptoms:
- pulsation in the eye area;
- frequent migraines;
- ophthalmotonus;
- pain, pain in the eyes;
- nosebleeds;
- light flickering;
- narrowing of the field of view.
Symptomatic manifestations may differ depending on the type of angiopathy. The most common form is the hypertensive form, in which there is increased arterial and intraocular pressure, hemorrhages in the retina, and tortuosity of the arteries. Diabetic angioneuropathy causes redness of the iris, swelling and degeneration of the retina, as well as elevated blood glucose levels.
Symptoms of angiopathy
As the disease progresses, symptoms worsen from stage to stage. It develops in the following sequence:
- the retinal arteries spasm;
- retinal vessels narrow;
- blood clots appear in the arteries;
- irreversible vasoconstriction;
- blood vessels rupture, numerous hemorrhages appear in the eyes;
- the blood supply to the retina is catastrophically disrupted - ischemia occurs, requiring surgical intervention.
At the onset of the disease, there are no clinical signs. The first symptoms appear in the second stage of the disease.
Signs of GAS:
- vision deteriorates;
- “flies” and “stars” run before your eyes;
- the image becomes blurry;
- visual fields partially disappear.
At the second stage of the disease, the patient, in addition to the listed symptoms, maintains high blood pressure. If an ophthalmologist does an examination, he will see a narrowing of the arterial vessels. The manifestation of this symptom at different stages of GAS manifests itself differently. Due to vasoconstriction, the blood supply to the organ deteriorates. If the situation is advanced, blood circulation stops.
Retinal angiopathy: what is it?
If retinal angiopathy of both eyes progresses for a long time and is not treated, then irreversible changes and various complications may begin in the body. For example, a person may experience retinal detachment due to a lack of blood in the vessels of the eyeball.
This may appear as a yellow spot on the apple of the eye. As a result, visual impairment occurs. Subsequently, complete blindness may develop based on such symptoms.
Retinal angiopathy is a pathology in which the vessels of the fundus of the eye are affected. It occurs in both adults and children of all ages.
The affected vessels may be dilated, narrowed or tortuous. Changes in the structure and tone of the walls of blood vessels and disruption of their functions are not an independent disease, but a consequence of other diseases.
Since in these diseases the pathological process spreads to all the vessels of the body, angiopathy is usually observed in both eyes.
When the arteries are damaged, the retina is insufficiently supplied with blood, resulting in poor vision. If there is no treatment, the process becomes irreversible and blindness may develop.
Retinal angiopathy is not an independent disease, but a symptom of various diseases that cause dysfunction of the blood vessels of the eye and changes in the structure of the vascular wall. A manifestation of vascular damage is a change in their tone, temporary reversible spasms.
Angiopathy that exists for a long time leads to irreversible consequences: necrotic changes in the area of the retina that was supplied with blood by the affected vessel, its thinning, ruptures and detachment. All these consequences are combined under the name retinopathy.
The condition of the retina is highly dependent on the quality of the blood supply, and when affected areas occur, vision is impaired and is not subsequently restored. If the area in the macula area is affected, central vision is impaired. If the retina is completely detached, blindness develops.
Diagnostics
Diagnosis and treatment of angiopathy by a qualified physician is determined by the severity of the disease.
During the diagnostic process, the doctor may prescribe magnetic resonance therapy, ultrasound, and x-rays. For additional studies, fluorescein angiography may be needed, which clearly depicts the processes of inflammation. And for a more in-depth study of pathology, Doppler ultrasound, measurement of pressure in the retinal vessels, and graphic recording of blood circulation are used.
You may also find it useful to learn more about what retinal dystrophy looks like and what can be done about such a problem.
Retinal angiopathy of mixed type
The human body is a single whole and pathological processes occurring in one organ or system often have manifestations in a completely different place. For example, retinal angiopathy of both eyes is a secondary manifestation or consequence of certain diseases.
Mixed type retinal angiopathy is the simultaneous development of several types of the disease.
This condition requires a thorough examination by a doctor and observation by several specialists of different profiles. The pathology is considered reversible and is manifested by temporary spasms in blood vessels, vascular paresis and dystonia.
The medical term angiopathy refers to damage to blood vessels; a typical cause is considered to be a disorder of nervous regulation. This pathological condition is characterized by dystonia, vascular paresis and temporary reversible spasms in them.
This term is very often used to describe lesions of large (macroangiopathy) and small (microangiopathy) vessels (capillaries) in various diseases, as well as in the presence of diabetes mellitus - diabetic angiopathy.
Classification
Depending on the target organs, clinical and morphological differences, the following types of angiopathy are distinguished:
- macroangiopathy of neck vessels;
- micro- and macroangiopathy of the vessels of the lower extremities;
- microangiopathy of the stomach and duodenum;
- angiopathy of cerebral vessels;
- chronic ischemic heart disease
- diabetic angionephropathy;
- diabetic angioretinopathy.
Macroangiopathy
Macroangiopathy of the neck vessels is expressed in the form of obliterating atherosclerosis of the carotid artery system. This macroangiopathy causes certain diagnostic difficulties, since it is asymptomatic in the primary stages. A clear manifestation may be a stroke , which is usually preceded by cases of transient ischemic attack .
Results of angiographic study for stenosis of the internal and external carotid arteries
Diabetic angiopathy of the lower extremities
Typically, the pathogenesis involves large main and sometimes small vessels of the lower extremities - the femoral, tibial, popliteal arteries and arteries of the foot. They experience accelerated progression of obliterating atherosclerotic processes as a result of complex metabolic disorders. The most common is bilateral multiple localization of pathogenesis, occurring without specific symptoms. There are four stages of ischemia :
- preclinical;
- functional, expressed as intermittent claudication;
- organic , causing pain at rest and at night;
- ulcerative-necrotic, causing trophic disorders and gangrene directly.
Hypoxia and, as a consequence, necrosis and atrophy of the lower limb muscles in diabetic angiopathy are caused by morphological changes in the microvasculature - thickening of the basement membranes, proliferation of the endothelium and deposition of glycoproteins in the walls of capillaries, as well as the development of Mönckeberg mediacalcinosis , which is a pathology of the middle membranes of blood vessels and has a characteristic radiological and ultrasound picture.
Diabetic angiopathy of the lower extremities
Against the background of DAP, patients can also develop polyneuropathy , osteoartopathy and diabetic foot syndrome (DFS) . Patients experience a whole system of anatomical and functional changes in the vascular bed, disruption of autonomic and somatic innervation, deformation of the bones of the foot and even lower leg. Trophic and purulent-necrotic processes over time turn into gangrene of the foot, fingers, and legs and may require amputation or excision of necrotic tissue.
Angiopathy of cerebral vessels
Diabetic macroangiopathies of the brain cause apoplectic or ischemic disorders of cerebral circulation, as well as chronic cerebral circulatory failure. The main manifestations are dystonia , temporary reversible spasms and vascular paresis .
The clinical picture is most often caused by pronounced proliferation and hyperplasia of intimal connective tissue (thickening of the arterial wall), dystrophic changes and thinning of the muscular layer, deposits of cholesterol , calcium salts and the formation of plaques on the walls of blood vessels.
Microangiopathy
Thrombotic microangiopathy leads to narrowing of the lumen of arterioles and the formation of multiple ischemic foci of damage. Manifestations of microangiopathy can be acute (stroke) or chronic; they are usually caused by diffuse or focal organic changes of vascular origin. Cerebral microangiopathy of the brain causes chronic cerebral circulatory failure.
Microangiopathy of the brain - what is it? Unfortunately, it has been established that the disease is a complication of diabetes, which is characterized by rapid progression of atherosclerosis and microcirculation disorders, which are practically asymptomatic. The first alarm bells may be attacks of dizziness, lethargy, deterioration of memory and attention, but most often the pathology is detected in the later stages, when the processes are already irreversible.
Microangionephropathy
Another type of microangiopathy is diabetic angionephropathy, which disrupts the structure of the walls of the blood capillaries of the nephron glomeruli and nephroangiosclerosis , which causes a slowdown in glomerular filtration, a deterioration in the concentration and filtration function of the kidneys. In the process of diabetic glomerulosclerosis , nodular, diffuse or exudative, caused by impaired carbohydrate and lipid metabolism in the kidney tissues, all arteries and arterioles of the glomeruli and even the renal tubules take part.
This type of microangiopathy occurs in 75% of patients with diabetes. In addition, it can be combined with the development of pyelonephritis , necrotizing renal papillitis and necronephrosis .
Diabetic angioretinopathy
Angioretinopathy also refers to microangiopathies, because the network of retinal vessels is involved in the pathogenesis. It occurs in 9 out of 10 diabetics and causes such severe disorders as rubeous glaucoma , edema and detachment , and retinal hemorrhages , which significantly reduce vision and lead to blindness.