Maculopathy is a complex ophthalmological disease, the main cause of which is diabetes mellitus. To prevent fatal complications caused by the progression of maculopathy, the patient needs timely and adequate medical care:
- clear interaction between specialists caring for a patient with diabetes mellitus (endocrinologist, angiosurgeon, neurologist, ophthalmologist);
- detailed consultation with an ophthalmologist and a full diagnostic examination;
- assessing the level of risk when identifying retinal damage leading to progressive deterioration of vision;
- timely prescription of adequate treatment.
Causes of maculopathy
Diabetic maculopathy is a consequence of generalized microangiopathy, in which the vascular bed in patients with diabetes is affected at the micro level. Risk factors that may be involved in the development of diabetic maculopathy include:
- A significant increase in the concentration of glucose in the patient’s blood plasma (severe glycemia).
- Arterial hypertension, accompanied by an increase in systemic blood pressure.
- Nephropathy, that is, kidney damage and dysfunction.
- Lipid metabolism disorders.
In the case of diabetic maculopathy, damage to the macula occurs as a result of diabetes mellitus, but maculopathy itself can occur in a patient even with initial signs of impaired carbohydrate metabolism.
Because visual function can suddenly deteriorate with diabetic maculopathy, patients with diabetes should visit their ophthalmologist regularly for preventive examinations. It is very important to clearly determine the topography of the macular region.
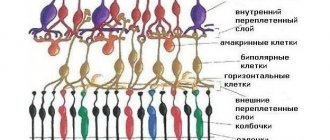
The macula area refers to the central region of the retina, which is responsible for clear vision. The diameter of the macula reaches 3500-5000 microns. This highly differentiated area is located on the side of the temple. It is deviated from the edge of the optic nerve by approximately 1500-2000 µm.
Reasons for development
The pathology is a consequence of vascular disorders, that is, the process of nutrition of the tissues responsible for central vision in the retinal area is disrupted. Due to insufficient blood flow, yellow pigment accumulates here, resulting in damage to the cones that are sensitive to light. The reasons for this condition may be:
- Genetic predisposition. It is believed that vascular sclerosis occurs more often in people whose relatives also had problems with the vascular system. These patients have an increased risk of developing maculopathy, but the individual can influence the reduction in the importance of such gene changes.
- Exposure to sunlight. Ultraviolet radiation damages retinal tissue, and someday regeneration processes will not be able to fully restore this area.
- Incorrect, poor nutrition. The lack of nutritional components in the diet is blood that is poor in vitamins and microelements. The result of this can be various diseases of systems and organs, and in a progressive form.
- Bad habits – smoking. Smoking has a particularly strong effect on the vascular system, damaging and thinning the walls of blood vessels.
- Arterial hypertension. Increased pressure in the bloodstream thins the vascular wall.
- Diabetes. Increased blood sugar levels (impaired carbohydrate metabolism) are one of the main causes of maculopathy.
There are other observations regarding individuals in whom ocular maculopathy appears more often:
- Women, especially after 50 years. Representatives of the fair sex are much more susceptible to this disease than men. Perhaps the reason is a sharp decrease in estrogen production during menopause.
- People of the white (European) race. Scientists have not yet found the reasons for this, but the fact remains a fact.
Diffuse maculopathy
In a patient with diabetic maulopathy (diffuse form), symptoms and diagnostic criteria for the disease include:
- Significant thickening of the retina, in which cystic changes can be detected. Against the background of obliteration, there is swelling, so it is not always possible to determine the location of the fovea.
- Fluorescein angiography reveals punctate plural hyperfluorescence, which corresponds to microaneurysms. You can also detect late edematous hyperfluorescence, which is more pronounced than during clinical examination.
- Due to the cystic edema of the macula, this area of the retina looks like a flower petal.
Edema maculopathy
With edematous maculopathy there is significant swelling. On fluorescein angiography, it appears as diffuse staining in the late phases of the study. With the initial manifestations of pathology, focal laser coagulation can be performed, which in most cases leads to stabilization of the retina.
Visual function in edematous maculopathy is most affected in elderly patients with insulin-dependent diabetes mellitus.
In any form of diabetic maulopathy, it is very important to eliminate the factors that damage the retina. In this regard, the primary task in this case is to compensate for the underlying pathological condition, that is, it is necessary to normalize the concentration of blood glucose. All this must be done as early as possible, since otherwise changes in the retinal vessels become irreversible.
In order to prevent or slow down the development of pathological changes in the retinal vessels, angioprotectors (dicinon, divascan, trental, angina) can be used. However, their effectiveness is not high, and in case of decompensated diabetes, there is no point in prescribing them.
Classification of diabetic maculopathy
In the practical work of an ophthalmologist, it is completely insufficient to simply state the fact of the presence of diabetic macular edema. Its manifestations must be classified accordingly in order to formulate a detailed diagnosis, which gives an idea not only of the degree of threat to the patient’s visual functions, but also determines treatment tactics aimed at preserving them.
However, until now, no single standard has been developed in approaches to the classification of diabetic maculopathy. It is generally accepted to divide diabetic macular edema into focal (exudative or circinate), diffuse (edematous), ischemic and mixed forms (Fig. 1-3, 4-7) [2, 6, 17, 18].
Subtypes of DM are also distinguished according to the localization of macular edema, the influence of systemic factors (nephropathy, hypertension, heart failure, pregnancy), macular edema as a complication of panretinal photocoagulation, or as a consequence of vitreoretinal traction. When classifying diabetic macular edema, some authors take into account secondary changes in the fundus tissue due to the long-term existence of retinal edema (changes in the pigment epithelium, microhemorrhages, epiretinal fibrosis, etc.), as well as clinical signs of concomitant diseases (macular drusen) [19].
Of course, any classification scheme is artificial, since in a real clinical situation the effect of a variety of clinical signs is always combined, the main of which in diabetic maculopathy are retinal edema due to disruption of the blood-ophthalmic barrier or vitreomacular traction, as well as retinal ischemia as a result of arteriolar and capillary occlusion. Secondary and concomitant changes in the membranes of the fundus have a significantly less impact on the dynamics of visual functions, so their consideration is not entirely justified, since it unreasonably complicates the classification of the underlying disease. Retinal ischemia has a strong impact on visual prognosis, but to date there are no effective methods for restoring retinal perfusion. For non-ischemic diabetic macular edema, multicenter studies have confirmed the effectiveness of laser coagulation [20-27]. It has also been established that early laser treatment is a fundamentally important condition for success. To this end, the ETDRS study developed the concept of “clinically significant macular edema.” Literally, this concept is defined as follows [27, 28]:
- retinal edema in the center of the macula or within 500 µm from it (Fig. 18a);
- hard retinal exudates in the center of the macula or within 500 µm from it with retinal edema (not residual, remaining in the coming months after laser treatment and disappearance of macular edema) (Fig. 18b);
- a zone or zones of retinal edema measuring more than one optic disc diameter when its nearest edge is removed from the center of the macula at a distance less than the diameter of the optic disc (Fig. 18c).
The concept of “clinically significant macular edema” has found wide use in modern ophthalmological literature and is a kind of standard when determining indications for laser treatment for the initial manifestations of diabetic maculopathy [17, 26, 29].
However, in practical work, an ophthalmologist often has to predict the result of laser treatment for long-standing retinal edema of the macula, which has led to the appearance of degenerative changes of varying severity and a decrease in visual acuity. For such cases, the American Academy of Ophthalmology proposes a four-level clinical classification of diabetic maculopathy (Table 1), which takes into account only the degree of involvement of the macula center in the pathological process.
Table 1. American Academy of Ophthalmology International Clinical Diabetic Maculopathy Severity Score.
| Severity level | Biomicroscopic signs |
| no DM | No retinal thickening or hard exudates in the posterior pole of the eye |
| Initial DM | Retinal thickening or hard exudates in the posterior pole of the eye away from the center of the macula |
| Moderate DM | Retinal thickening or hard exudates near the center of the macula, but not involving the center |
| Heavy DM | Retinal thickening or hard exudates involving the center of the macula |
Note: Hard exudates are a sign of existing or pre-existing retinal edema and require three-dimensional evaluation using slit-lamp biomicroscopy or stereophotography.
Meanwhile, it is known that focal and diffuse types of diabetic macular edema respond differently to laser treatment and have a different prognosis for the patient’s vision [30]. In this regard, there is every reason to assume that the above classification, proposed as an international one, does not sufficiently reflect the real clinical situation and is unlikely to find wide clinical application.
In the interests of clinical practice, a simple classification is urgently needed that allows one to reasonably link the main signs of the disease with the prognosis of the anatomical and functional results of modern methods of treating diabetic maculopathy. Based on this approach, we developed our own classification of diabetic macular edema (Table 2) [31-34].
Table 2. Classification of diabetic maculopathy.
| STAGE DM | DEFINITION (combination or any of the characteristics) | Treatment | REP. INSPECTION | FORECAST FOR READING |
| no DM | ¨ there is no evidence for the presence of diabetic macular edema. | — | ** | very good |
| DM-0, subclinical | ¨ There is no clinically significant macular edema. | — | * | good |
| DM-1, initial | ¨ focal macular edema with initial visual acuity of 0.5 or higher. | OK | 4 months* | good |
| DM-2, moderate | ¨ focal macular edema with initial visual acuity less than 0.5. | OK | 4 months* | often bad |
| DM-3, heavy | ¨ focal retinal edema with focal detachment of the neuroepithelium or with deposits of large hard exudates in the center of the foveola***; ¨ mixed or flat diffuse retinal edema***. | OK | 4-6 months* | usually bad |
| DM-4, far gone | ¨ diffuse retinal edema with traces of dense laser photocoagulation of the “lattice” type; ¨ transudative retinal detachment of the macular area; ¨ ischemic maculopathy with initial visual acuity less than 0.5; ¨ retinal fibrosis of the macula. | ZVE, IVVK | ** | bad |
| DM-5, outcome | ¨ old transudative retinal detachment with hard exudates; ¨ gross fibrous changes in the macula; ¨ deep atrophy of the pigment epithelium and choriocapillaris in the macula, retinal edema may be absent. | — | ** | bad |
* - the period for re-inspection can be determined or
** - determined by the level of severity of diabetic retinopathy.
*** - regardless of visual acuity at the time of laser treatment.
This classification is based on the results of treatment, as well as on the basis of taking into account only those clinical signs that affect the prognosis to preserve the patient’s ability to read. To determine the initial DM (DM 1), we used the concept of clinically significant macular edema ETDRS as a generally accepted standard of indications for laser coagulation. However, this implied focal macular edema while maintaining high visual functions of the patient (Vis = 0.5 and above). Initial MD responds well to laser treatment, which ensures long-term preservation of the patient's ability to read. Moderate diabetic maculopathy (DM 2) was defined by us as focal macular edema, but with significantly more significant visual disturbances (Vis < 0.5). Moderate DM also responds well to laser photocoagulation; in most cases, it is possible to achieve regression of diabetic macular edema, which has a beneficial effect on the patient’s prospects for central vision. However, the prognosis for reading is often poor. Diffuse and mixed types are classified as a severe stage of DM (DM 3), since they are characterized by a poor prognosis for reading and anatomical results of laser coagulation.
With severe focal macular edema, multifocal leakage leads to extensive retinal edema, which is quite legitimately classified as a mixed type of DM. It is characterized by a more uniform pattern of retinal edema than with the focal type and a much larger amount of hard exudates than with diffuse maculopathy. In turn, diffuse macular edema can be layered on the pre-existing focal type of DM and this clinical situation can also be classified as a mixed type of diabetic maculopathy. In such cases, differentiating advanced focal, mixed and diffuse macular edema can be extremely difficult, both according to biomicroscopy and the results of fluorescein angiography. However, since the listed clinical variants of DM have approximately the same prognosis for reading and anatomical treatment results, regardless of the initial visual acuity, it is legitimate to limit ourselves to determining the level of severity of diabetic macular edema - severe DM (DM 3). The remaining stages are also necessary to assess the severity of diabetic maculopathy, prognosis of visual function and the feasibility and effectiveness of laser treatment.
The presented classification of diabetic maculopathy is not complete. Improving knowledge about the pathogenesis of the disease, the emergence of new research methods, for example, the wider distribution of optical coherence tomography, and the introduction of new treatment methods will inevitably greatly change the classification we propose. However, the principle of its construction – linking the signs of the disease with the prognosis to preserve the patient’s ability to read after laser treatment, it seems to us, should stand the test of time.
Diagnostics
Maculopathy in diabetes mellitus can be diagnosed using retinal fluorescein angiography. This study allows you to identify areas of ischemia, points of active filtration, areas of cystic edema, signs of neovascular membrane formation, and symptoms of retinal rupture. Based on fluorescein angiography data, it is possible to decide on the advisability of laser coagulation of the retina.
Also, to diagnose maculopathy in diabetes mellitus, retinal photography in the red-free range and color photography of the fundus are used. At the same time, various changes in blood vessels caused by diabetes mellitus are recorded. Photography helps to perform an initial assessment of the condition of the retina, as well as monitor dynamic changes during treatment.
Treatment of macular retinal degeneration
Age-related Macular Degeneration of the Retina or MACULOPATHY is a disease that affects the posterior segment of the eye, and specifically the central part of the retina - the macula.
The macula is responsible for the central vision of the eye, that is, it allows us to see straight ahead.
Maculopathy is considered the number one cause of vision loss in people over the age of 60 and, according to statistics from the American Academy of Ophthalmology, affects approximately 5% of people who reach this age.
The disease “maculopathy” is progressive and can be diagnosed before complaints of decreased vision appear.
In the early stages, as a rule, maculopathy has no symptoms, but as the disease progresses, symptoms of loss of central vision gradually appear, which also progressively worsens.
Early diagnosis of the disease allows you to successfully combat it
There are 2 forms of Maculopathy:
1.Dry
2.Wet
DRY Maculoptia is the most
Dry maculopathy is characterized by the formation of yellow-white deposits (drusen) under the retina.
There is no specific treatment for dry retinal degeneration.
Taking vitamins, antioxidants and zinc supplements can slow down the progression of the disease. Over time, dry retinal degeneration can progress to wet maculopathy.
The WET form of Macular Retinal Degeneration occurs This abnormal vascular network is very fragile, the vessels break, resulting in the release of blood and fluid under the retina, which in turn causes damage to the macula with further formation of a scar on it and a significant decrease in vision. Loss of vision in this case can be permanent, since pathological vascular formation and the presence of scar tissue continue to destroy healthy retinal tissue, the damaged light receptors are not restored and are not replaced by new ones.
Symptoms of Wet Form of Age-Related Macular Degeneration:
If you notice the following changes in your vision, you should immediately consult an ophthalmologist:
1. Habitually straight lines do not look straight but are curved, or irregularities have appeared in the center of vision - clinical name - (metamorphopsia)
2.Dark or blind spots appeared in the center of the visual field (scotoma)
3. Faces or objects in front of you look unusually dark.
During examination and a special examination (OCT), the doctor will be able to exclude or confirm the diagnosis of maculopathy
Treatment of Maculopathy.
The wet form of Maculopathy is a disease that must be treated in the early stages and immediately after its detection.
Since the disease is chronic, it is necessary to carry out repeated therapy at a certain period of time, depending on the course of the disease.
Today, there are several proven treatments for wet maculopathy.
The sooner treatment is started, the greater the chance of maintaining central vision.
One type of therapy is intravitreal injection of drugs that cause the cessation of formation and partial disappearance of newly formed vessels under the retina.
In recent years, in Western Europe and the USA, the drug MACUGEN® (pegaptanib sodium) has been used: in a sterile operating room, the drug is dosed into the vitreous cavity in close proximity to the affected retina through a microneedle. Preliminary drip of anesthesia ensures complete painlessness of the surgical procedure. The manipulation is carried out on an outpatient basis, after which the patient can lead his usual lifestyle; it is only necessary to instill drops 3 times a day for 3-5 days after the operation.
After 6-8 weeks, it is necessary to conduct a control examination of the macula (CT) and, if necessary, re-introduce the drug into the vitreous cavity.
Treatment of maculopathy
Treatment of diabetic maculopathy can be divided into conservative therapy and laser surgery. Laser coagulation of the retina is the most effective, but this operation does not provide a guaranteed result.
Any patient with diabetes must adhere to a strict diet and also regularly monitor their blood glucose levels. To reduce the risk of complications, it is necessary to take all prescribed medications and periodically visit an ophthalmologist for routine examinations.
Prevention
The main preventive measure for edematous maculopathy is maintaining compensation for diabetes mellitus for as long and stable as possible. Patients with this disease need to carefully monitor glycemic levels in the laboratory and at home, and adhere to effective treatment for diabetes mellitus. Depending on how timely such measures are started, a long-term prognosis for the course of the disease can be drawn up.
To prevent changes in the retinal vessels themselves, as well as for medicinal purposes, angioprotectors can be prescribed: dicynon, divascan, sore throat, trental. Although, if there is insufficient compensation for carbohydrate metabolism disorders, their effect turns out to be ineffective.
Diabetes mellitus is a compelling argument to strictly adhere to a special diet, monitor blood glucose levels on an ongoing basis, be sure to take special medications, and regularly visit an ophthalmologist to examine the fundus of the eye.
The specialists of our clinic have accumulated extensive experience in treating patients with edematous maculopathy, including those of diabetic origin. Thanks to the technological equipment of the center, it is possible to identify the disease at the earliest stages and receive timely, modern treatment of European quality. In addition, in our clinic there is a service of clinical observation of patients with diabetic maculopathy, management of such patients, organization of long-term measures to prevent the development of the pathological process.