Description
Glaucoma (from the Greek - the color of sea water, azure) is a serious disease of the organ of vision, named after the greenish color that the dilated and motionless pupil acquires at the stage of the highest development of the disease process - an acute attack of glaucoma. This is also where the second name for this disease comes from – “green water” or “green cataract” (from the German “Grun Star”). Currently, there is no uniform understanding of the causes and mechanisms of development of this disease; certain difficulties are encountered even in the very attempt to define the concept of “glaucoma”. Today, glaucoma is commonly called a chronic eye disease, characterized by a constant or periodic increase in intraocular pressure (IOP) with the development of trophic disorders in the outflow pathways of intraocular fluid (IOG, aqueous humor), in the retina and in the optic nerve, causing the appearance of typical defects in the visual field and development marginal excavation (deepening, pushing) of the optic nerve head. Thus, the term “glaucoma” unites a large group of eye diseases (about 60) that have the following common features: 1. Intraocular pressure (IOP) constantly or periodically exceeds the individually tolerated (tolerant) level; 2. A characteristic lesion of the optic nerve fibers develops - glaucomatous optic neuropathy, leading in its final stage to its atrophy; 3. Visual dysfunction characteristic of glaucoma occurs. Glaucoma can occur at any age, starting from birth, but the prevalence of the disease increases significantly in old age and old age. Thus, the frequency of congenital glaucoma is 1 case per 10-20 thousand newborns; at the age of 40-45 years, primary glaucoma is observed in approximately 0.1% of the population. In the age group of 50-60 years, glaucoma occurs in 1.5% of cases, and in people over 75 years of age, in more than 3%. This disease ranks among the leading causes of incurable blindness and is of great social importance.
Diagnostics
Congenital glaucoma is identified by an ophthalmologist based on examination data and ophthalmological studies (tonometry, gonioscopy, keratometry, biomicroscopy, ophthalmoscopy, ultrasound biometry). Also, an important role in the diagnosis of this condition is played by genetic studies, the study of hereditary history and the course of pregnancy. Upon examination, enlarged (in the early form) or normal size of the eyes are detected; swelling of the tissues surrounding the eyeball may also be observed. The horizontal diameter of the cornea is increased, micro-tears and clouding are possible on it, the sclera is thinned and has a bluish tint, the iris is also affected in congenital glaucoma - atrophic processes occur in it, the pupil reacts sluggishly to light stimuli. The anterior chamber of the eye is deepened (1.5-2 times more than the age norm). No pathological changes occur in the fundus for a long time, since due to the increase in the size of the eyeball, intraocular pressure initially does not reach significant values. But then excavation of the optic disc develops quite quickly, however, as the pressure decreases, the severity of this phenomenon also decreases. Due to the increase in eye size, congenital glaucoma causes thinning of the retina, which, if left untreated, can lead to its rupture and rhegmatogenous detachment. Often, against the background of such changes, myopia is detected. Tonometry shows a slight increase in intraocular pressure, but this indicator should be compared with the anteroposterior size of the eye, since scleral stretching smoothes out IOP values. A study of the hereditary history can reveal similar changes in the patient’s relatives, and it is often possible to determine an autosomal recessive type of inheritance - this indicates in favor of primary congenital glaucoma. The presence of maternal infectious diseases, injuries, and exposure to teratogenic factors during pregnancy indicates the possibility of developing a secondary form of the disease. Genetic diagnosis is carried out through direct sequencing of the CYP1B1 gene sequence, which makes it possible to identify its mutations. Thus, only a geneticist can clearly prove the presence of primary congenital glaucoma. In addition, if one of the parents or their relatives has this condition, a search for the pathological form of the gene can be performed before conception or prenatal diagnosis through amniocentesis or other techniques.
Symptoms
There are congenital glaucoma, juvenile glaucoma (juvenile glaucoma, or glaucoma of young age), primary adult glaucoma and secondary glaucoma. Congenital glaucoma can be genetically determined (predetermined) or caused by diseases and injuries of the fetus during embryonic development or during childbirth. This type of glaucoma appears in the first weeks and months of life, and sometimes several years after birth. This is a fairly rare disease (1 case per 10-20 thousand newborns). Congenital glaucoma develops as a result of developmental anomalies (mainly in the angle of the anterior chamber), often resulting from various pathological conditions of the mother (especially before the 7th month of pregnancy). The development of congenital glaucoma is caused by infectious diseases (rubella, mumps, polio, typhus, syphilis, etc.), vitamin deficiency A, thyrotoxicosis, mechanical injuries during pregnancy, poisoning, alcoholism, exposure to ionizing radiation, etc. In 60% of cases, congenital glaucoma is diagnosed in newborns. This condition is sometimes referred to in the medical literature as “hydrophthalmos” (dropsy of the eye) or “buphthalmos” (bull’s eye). The cardinal signs of congenital glaucoma are high intraocular pressure (IOP), bilateral enlargement of the cornea, and sometimes the entire eyeball. Congenital glaucoma. Congenital glaucoma. Note the large diameter of the cornea. In the left eye, the cornea is swollen due to increased intraocular pressure (~35 mm. Juvenile (youthful) glaucoma occurs in children over three years of age. The age limit for this type of glaucoma is 35 years. Primary adult glaucoma is the most common type of glaucoma associated with age-related changes in the eye. Secondary glaucoma is a consequence of other ocular or general diseases, accompanied by damage to those ocular structures that are involved in the circulation of intraocular moisture or its outflow from the eye. Vomiting. Nausea.
Glaucoma
Congenital glaucoma
ICD-10 Category: Q15.0
Content
Definition and general information [edit]
Synonyms: buphthalmia, buphthalmos, primary congenital glaucoma
Congenital glaucoma is the result of abnormal development of the drainage structures of the eye, characterized by increased intraocular pressure, increased size of the eyeball (buphthalmos), corneal edema and excavation of the optic nerve, clinically manifested by a characteristic triad - epiphora, photophobia and blepharospasm.
Congenital glaucoma is the most common form of glaucoma in infants. The prevalence in Europe is estimated to be around 1/27,800 live births. Boys are more often affected than girls. Congenital glaucoma is bilateral in 70-80% of cases.
Most cases are sporadic, with approximately 10% of cases showing autosomal recessive inheritance with variable penetrance.
Etiology and pathogenesis[edit]
The etiology of congenital glaucoma is not yet fully understood; it is assumed that the obstruction to the outflow of moisture occurs in the area of the anterior chamber angle, at the level of the trabecula. Gene mapping of the affected families helped identify three chromosomal loci: GLC3A (2p22.2), GLC3B (1p36) and GLC3C (14q24.3-q31.1), of which the CYP1B1 gene (2p22.2) of the GLC3A locus contains mutations. Mutations in the LTBP2 (14q24.3) and MYOC (1q23-q24) genes were also identified.
Clinical manifestations[edit]
In approximately 80% of cases, congenital glaucoma is detected in the first year of life, but sometimes the age of onset may be delayed until early adulthood. The classic triad of symptoms includes epiphora, blepharospasm and photophobia. In children, attention is drawn to red, “wet” eyes, clouding of the cornea and an increase in eye size caused by stretching of the immature eye due to increased intraocular pressure. Children over 3 years of age develop progressive myopia and decreased visual fields. If left untreated, congenital glaucoma invariably leads to blindness.
Congenital glaucoma: Diagnosis [edit]
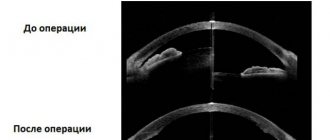
A complete ophthalmologic examination reveals opacification of an enlarged cornea and the presence of Haab's bands, increased intraocular pressure (more than 20 mm Hg or asymmetry more than 5 mm Hg), a deep anterior chamber, abnormally high insertion of the iris, a poorly developed scleral spur (with gonioscopy), an increase in the cup-to-disc ratio of the optic nerve head, and refractive tests detect myopia and astigmatism. If necessary, the examination is carried out under anesthesia.
Differential diagnosis[edit]
Differential diagnoses for redness and lacrimation include nasolacrimal duct obstruction, conjunctivitis, corneal abrasion, and uveitis. The differential diagnosis of corneal enlargement includes high axial myopia and megalocornea. The differential diagnosis of corneal opacities and edema includes congenital corneal dystrophies, birth injuries, keratitis, congenital ocular anomalies, or storage diseases. The differential diagnosis of optic nerve excavation includes physiological excavation, optic nerve coloboma, genetic atrophy, and optic nerve hypoplasia.
Congenital glaucoma: Treatment[edit]
Congenital glaucoma is mainly cured surgically, with medical therapy playing only a supporting role. Goniotomy is traditionally recommended for children aged 2 to 3 years with a clear cornea. Trabeculotomy is offered to children in whom the angle is inadequately visible and to older children. In refractory cases, trabeculectomy and glaucoma drainage devices are used. Amblyopia, corneal scarring and cataracts are late complications of the pathology. Early visual rehabilitation is important to prevent amblyopia. Patients may require regular lifelong surveillance with IOP monitoring.
Prevention[edit]
Other [edit]
The prognosis largely depends on the timing of manifestation; early diagnosis and surgical treatment significantly affect the visual prognosis. Most patients successfully treated in infancy have good IOP control and fully functional visual fields in adulthood.
ARTICLES ON THE TOPIC: Congenital glaucoma prognosis Dental glaucoma Glaucoma after lasik
Treatment
The goal of any glaucoma treatment technique is to normalize intraocular pressure. Today, there are three types of treatment for this disease: medication, laser and surgery. After a thorough diagnostic examination and identification of glaucoma, an individual treatment regimen is drawn up for each patient. It depends on the form, stage of the disease and the presence of concomitant pathology. In the early stages of glaucoma, conservative treatment (eye drops) can be used. Unfortunately, medication is not always effective. The most effective methods of stopping the development of glaucoma and preserving vision remain laser treatment and surgery. Iridectomy. This is a laser technique aimed at treating angle-closure glaucoma. During an iridectomy, a tiny laser hole is made in the iris of the eye to create additional drainage of intraocular fluid. Iridectomy is performed on an outpatient basis. Non-penetrating deep sclerectomy (NPDS). This is a non-penetrating surgical operation - without opening the eyeball. During this procedure, they do not use a through hole, but create a special valve in the outer shell of the eye - the sclera, through which the unhindered outflow of intraocular fluid is possible. This allows you to restore the balance of fluid in the eye and normalize pressure. The operation is performed on an outpatient basis and does not provoke the development of cataracts. The rehabilitation period for patients after NGSE is several days. Viscocanalostomy. An operation aimed at stabilizing vision in glaucoma is currently very popular in Europe and the USA. Refers to non-penetrating surgical operations. Its goal is to restore the physiological pathways of fluid outflow by creating a special “window” in the sclera. Its main difference from NGSE is that to restore the outflow of fluid, a special viscous substance is injected into the drainage tubules - Healon (Artivisk). By expanding the lumen of the drainage tubules, Gealon restores the permeability of moisture and allows you to restore fluid balance without opening the eyeball. The operation is performed on an outpatient basis, without causing the development of cataracts. The rehabilitation period for patients is 1–2 days.
Suspicion of glaucoma
ICD-10 code H40.0 for Suspected glaucoma
ICD-10
ICD-10-CM 10th Revision 2016
ICD-10-GM ICD-10 in Germany
ICD-10 ICD-10 in Russian
ICD-10 International Statistical Classification of Diseases and Related Health Problems 10th Revision
ICD-10
ICD-10 is the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD), a medical classification list by the World Health Organization (WHO).
It contains codes for diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases.
The Anatomical Therapeutic Chemical (ATC) Classification System is used for the classification of active ingredients of drugs according to the organ or system on which they act and their therapeutic, pharmacological and chemical properties.
It is controlled by the World Health Organization Collaborating Center for Drug Statistics Methodology (WHOCC).
The defined daily dose (DDD) is a statistical measure of drug consumption, defined by the World Health Organization (WHO).
It is used to standardize the comparison of drug usage between different drugs or between different health care environments.
SEE ALSO: Glaucoma how to treat it Post-traumatic secondary glaucoma History of the disease glaucoma An m-cholinomimetic is used to treat glaucoma The medicine bimatoprost for glaucoma
Classification
Glaucoma is classified according to: origin, age of the patient, mechanism of increased intraocular pressure, level of IOP, degree of change in visual fields and damage to the optic nerve head and type of course.
By origin: primary, secondary, combined with developmental defects of the eye and other body structures.
By patient age: congenital, juvenile, adult glaucoma.
According to the mechanism of IOP increase: open-angle, closed-angle, glaucoma with dysgenesis of the anterior chamber angle, glaucoma with pretrabecular block.
By IOP level: hypertensive, normotensive; with normal, moderately elevated and high IOP.
According to the degree of change in visual fields and damage to the optic nerve head: initial, developed, advanced, terminal.
According to the flow (dynamics of visual functions): stabilized, unstabilized.
Treatment with medication
Drops
The doctor will add Miotic drops – a 1% solution of pilocarpine – to the treatment regimen.
It is necessary to drip for 2 hours, 1 drop in each eye with an interval of 15 minutes. For the next 2 hours, drip every half hour, and then after 1 hour. Subsequent use of the drug is carried out 3-6 times a day. It all depends on the degree to which the pressure inside the eye is reduced. This treatment regimen is used if the test result for pilocarpine is positive.
Pilocarpine is used in the treatment of glaucoma
An additional drug is a 0.5% solution of Timolol. It should be taken 1 drop 2 times a day. The duration of therapy is prescribed by the doctor, taking into account the degree of the pathological process.
Preparations for internal use
When treating glaucoma, your doctor may prescribe medication to take internally. The treatment plan will include:
- Diacarb 0.25 g 3 times a day,
- Trusopt – 3 times a day,
- Azopt – 2 times a day.
Azopt drops are used in the treatment of glaucoma.
Diuretics may be prescribed orally or intravenously. The most commonly used solution is 50% glycerin. Its dosage will be 1.5-2 g/kg. If the pressure does not decrease, then a diuretic can be administered intramuscularly. Furosemide 20-40 mg is used.
If the treatment provided does not bring the desired result, then a “lytic mixture” is injected intramuscularly to reduce intraocular pressure:
- 1-2 ml of 2.5% solution of aminazine,
- 1 ml of 2% diphenhydramine solution,
- 1 ml of 2% promedol solution.
Component of the “lytic mixture” – Diphenhydramine
After administration of the medicine, the patient must remain in bed. The fact is that within 3-4 hours blood pressure may drop sharply.
Vitamins for vision
According to ongoing studies, it has been found that vitamins have a positive effect on the visual organs in the treatment of glaucoma. If you use lutein-containing drugs in addition to the main treatment, this will allow you to achieve fairly high efficiency in a short period of time. The most commonly used are Lutein Forte and Lutein Complex.
Lutein forte
Surgical method
If, when using conservative therapy methods, it is not possible to obtain the desired effect and intraocular pressure increases, then the doctor decides to perform surgery. Its essence is that pressure compensation is created on the iris between the anterior and posterior chambers of the organ of vision. Such an operation for glaucoma does not allow the blockade to recur during the outflow of intraocular fluid. This occurs due to the fact that an artificial drain is created for it so that after the operation the pressure does not increase. To perform the operation, the doctor uses local anesthesia. And it can be done on an outpatient basis.
Laser surgery for glaucoma
After the operation, a sterile bandage is applied to the patient's eye. He should not rub or apply mechanical pressure to the eye. In the first days after surgery, you should not watch TV or read a book for a long time. After the operation, the patient should avoid physical activity and not visit the bathhouse or sauna.
Folk remedies
It is impossible to cure glaucoma using folk remedies, but it is quite possible to relieve symptoms and reduce intraocular pressure. To do this, you need to choose one of the following recipes:
Take 20 g of honey, 10 ml of onion juice, 20 ml of dandelion juice. Mix all components and leave for 3 hours in a dark place. Drop the resulting mixture into the eyes, 2 drops 2-3 times a day.
- Every day on an empty stomach, drink 200 ml of tomato juice with a dissolved spoon of honey.
- Mix 100 ml of nettle and 10 g of lily of the valley flowers. Add a glass of warm water. Leave in a dark place for 9 hours. After this, add 5 g of soda to the solution. Use the solution as a compress on the eyes. The duration of the manipulation is 15-20 minutes. Carry out such procedures 2 times a day.
- Take equal quantities of rowan fruits, spring primroses, woodlice, and black currant leaves. Pour 20 g of raw material into 200 ml of boiling water. Leave for 30 minutes. Filter and take throughout the day.
- Wash the aloe leaf thoroughly and chop it finely. Pour a glass of water, simmer for 2-3 hours, filter and use the solution to wash the eyes 2-3 times a day.
- Buy a tincture of dill syrup and combine it in equal quantities with honey. Wait 2 hours and then use as an instillation solution. 2 drops in each eye. Carry out therapeutic measures 2 times a day.
- Take 150 g of celery, 200 g of carrots, 100 g of beets, 50 g of parsley, 100 g of cucumbers. Squeeze juice from all products, combine and consume throughout the day.
- Combine equal amounts of blueberries and honey. Consume 10-20 g per day.
Differential diagnosis
| Acute iridocyclitis | Acute attack of glaucoma | |
| Pain | Moderate | Strong |
| Injection | Deep ciliary | Deep ciliary |
| Pupil | Irregularly shaped narrowed | Extended, oval |
| IOP | Normal, decreased, or increased for the first few times. hours | High |
| Environments of the eye | Precipitates, exudate in the pupil area | Corneal edema |
| Vision | Slightly reduced | Sharply reduced |
| Secretion | Tearing | Tearing |
| Start | Usually gradual | Sudden |
| General complications | Little expressed | Prostration and vomiting |
H40.0 Suspicion of glaucoma
| Pharm. groups | Active substance | Trade names |
| Adrenergic and sympathomimetics (alpha, beta) | Dipivefrin* | Oftan ® Dipivefrin |
| Alpha adrenergic agonists | Brimonidine* | Luxfen ® |
| Phenylephrine* | Irifrin ® | |
| Neosynephrine-POS ® | ||
| Anticongestants | Phenylephrine* | Irifrin ® BK |
| Beta blockers | Betaxolol* | Betoptik ® |
| Betoptik ® S | ||
| Betoftan | ||
| Timolol* | Okumed ® | |
| Okupres-E ® | ||
| Oftan ® Timolol | ||
| Timolol Bufus | ||
| Timolol-MEZ | ||
| Timoptic | ||
| Timoptik-depot | ||
| Beta blockers in combinations | Brinzolamide + Timolol | Azarga |
| Dorzolamide + Timolol | Dorzopt Plus | |
| Pilocarpine + Timolol | Pilotimol ® | |
| Pilotimol ® mini | ||
| Timpilo | ||
| Fotil ® | ||
| Fotil ® forte | ||
| m-cholinomimetics | Pilocarpine | Oftan ® Pilocarpine |
| Ophthalmic products | Betaxolol* | Xonef ® |
| Xonef ® BK | ||
| Latanoprost* | Xalatamax | |
| Lanotan | ||
| Timolol* | Timolol-POS ® | |
| Timolollong ® | ||
| Phenylephrine* | Neosynephrine-POS ® | |
| Ophthalmic agents in combinations | DUOTRAV ® | |
| Latanoprost + Timolol | Xalacom ® | |
| Prostaglandins, thromboxanes, leukotrienes, their analogs and antagonists | Latanoprost* | Xalatan ® |
| Travoprost* | Travapress | |
| Travatan ® | ||
| Enzymes and antienzymes | Brinzolamide* | Azopt ® |
| Brinzopt | ||
| Dorzolamide* | Dorzolamide-SOLOpharm | |
| Dorzolan ® solo |
Information
Sources and literature
- Protocols for the diagnosis and treatment of diseases of the Ministry of Health of the Republic of Kazakhstan (Order No. 764 of December 28, 2007) 13. List of references: 1. American Academy of Ophthalmology. Guideline. Primary Angle Closure. 2000. 2. American Academy of Ophthalmology. Guideline. Primary Open-Angle Glaucoma. 2003. 3. American Academy of Ophthalmology. Guideline. Primary Open-Angle Glaucoma Suspect. 2002. 4. Prodigy Knowledge. Prodigy Guidance-Glaucoma. 2004. 5. EBM Guidelines. Glaucoma. 2004. 6. American Academy of Ophthalmology. Primary Open-Angle Glaucoma Suspect (Initial and Follow-up Evaluation). 2003. 7. ICO International Clinical Guidelines. . Primary Open-Angle Glaucoma (Initial and Follow-up Evaluation). 2005. 8. Rossetti L., Marchetti I., Orzalesi N. Randomized clinical trials on medical treatment of glaucoma: are they appropriare to guide clinical practice? //Arch. Ophalmol/ - 1993, 111: 96-103. 9. Glaucoma Laser Trial Group. The glaucoma laser trial (GLT) and glaucoma laser trial follow-up study: results. Am J Ophthalmol 1995, 120: 718-731. 10. Migdal C, Gregory W., Hitchins R., Kolker AE. Long-term functional outcome after early surgery compared with laser and medicine in open angle glaucoma. Ophthalmology 1994, 105: 1651-1657 11. Collaborative normal-tension glaucoma study group. The effectiveness of intraocular pressure reduction in the treatment of normal tension glaucoma. Am J Ophthalmol 1998, 126: 498-505. 12. Edwards RS. A study comparative of Ocuset Pilo 40, intensive pilocarpine and low-dose pilocarpine in the initial treatment of primary acute angle-closure glaucoma. Curr Med Res Opin 1997, 13:501-509. 13. Evidence-Based Medicine Guidelines. DUODEMECUM Medical Publications. 2001.
Information
List of developers: Kobtseva V.Yu., Research Institute of Eye Diseases of the Ministry of Health of the Republic of Kazakhstan
Clinics for treatment with the best prices
Price
Total: 196in 21 cities
| Selected clinics | Phones | City (metro) | Rating | Price of services |
| JSC "Medicine" in 2nd Tverskoy-Yamsky Lane | +7(495) 152..show Appointment +7(495) 152-59-88+7(495) 229-00-03+7(495) 775-74-78 | Moscow (m. Mayakovskaya) | rating: 4.4 | 87970ք (80%*) |
| First City Hospital named after. N.I. Pirogov | +7(499) 764..show+7(499) 764-50-02+7(495) 952-41-25+7(495) 536-91-16 | Moscow (m. Oktyabrskaya) | — | 48000ք (70%*) |
| KB No. 85 on Moskvorechye | +7(499) 782..show+7(499) 782-85-85+7(926) 010-84-87+7(499) 324-70-15+7(499) 324-86-65 | Moscow (m. Kantemirovskaya) | — | 53030ք (70%*) |
| Medic on Badaev | +7(812) 458..show Record +7(812) 458-00-00 | St. Petersburg (metro Prospekt Bolshevikov) | rating: 4.2 | 9100ք (60%*) |
| MedicCity on Poltavskaya | +7(495) 604..show Recording +7(495) 604-12-12 | Moscow (metro station Savelovskaya) | rating: 4.5 | 11520ք (60%*) |
| Euromedical clinic on Sirenevy Boulevard | +7(499) 519..show Appointment +7(499) 519-33-83+7(499) 519-33-73+7(495) 126-38-25 | Moscow (metro station Pervomaiskaya) | rating: 4.3 | 11550ք (60%*) |
| NEARMEDIC on Sretenka | +7(495) 152..show Recording +7(495) 152-58-65+7(495) 617-11-71 | Moscow (metro Sretensky Boulevard) | rating: 4.4 | 11840ք (60%*) |
| Clinic of functional disorders on Gabrichevsky | +7(495) 152..show+7(495) 152-58-35+7(495) 363-07-54+7(499) 654-08-00 | Moscow (metro station Shchukinskaya) | — | 13060ք (60%*) |
| President-Med on Yakornaya | +7(499) 618..show Appointment +7(499) 618-60-10+7(499) 618-81-10+7(966) 016-74-21 | Moscow (metro station Kolomenskaya) | — | 13500ք (60%*) |
| Family doctor on 1st Miusskaya | +7(495) 152..show Appointment +7(495) 152-59-85+7(499) 969-25-74+7(495) 126-99-31+7(926) 800-07-19 | Moscow (metro station Novoslobodskaya) | rating: 4.5 | 14885ք (60%*) |
| * — the clinic does not provide 100% of the selected services. More details by clicking on the price. | ||||
Attention!
If you are not a medical professional:
- By self-medicating, you can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Guide” cannot and should not replace a face-to-face consultation with a doctor. Be sure to contact a medical facility if you have any illnesses or symptoms that concern you.
- The choice of medications and their dosage must be discussed with a specialist. Only a doctor can prescribe the right medicine and its dosage, taking into account the disease and condition of the patient’s body.
- The MedElement website and mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Directory” are exclusively information and reference resources. The information posted on this site should not be used to unauthorizedly change doctor's orders.
- The editors of MedElement are not responsible for any personal injury or property damage resulting from the use of this site.
Source
Glaucoma (H40)
Excluded:
- absolute glaucoma (H44.5)
- congenital glaucoma (Q15.0)
- traumatic glaucoma due to birth trauma (P15.3)
Glaucoma (primary) (residual stage):
- capsular with false detachment of the lens
- chronic simple
- with low pressure
- pigmented
Angle-closure glaucoma (primary) (residual stage):
- acute
- chronic
- intermittent
If necessary, an additional code is used to identify the cause.
If necessary, an additional code is used to identify the cause.
If necessary, an additional code is used to identify the cause.
If it is necessary to identify the drug that caused the lesion, use an additional external cause code (class XX).
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without other instructions.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
Prevention of glaucoma
Prevention of glaucoma includes compliance with the following rules and recommendations:
- Avoid stressful situations, if necessary, change your place of work;
- Do not lift heavy weights, especially for women and the elderly;
- If you read a book, do any assignments (lessons, etc.), work at the computer, watch TV, do it in good lighting, and if your eyes are tired, put aside your hobby for a while, give your eyes a rest, at the rate of 1 hour work – 15 minute break;
- Try to eat foods enriched with vitamins and microelements, limit your intake of sugar and animal fats;
- Avoid excessive consumption of coffee, give up alcohol, smoking;
- When drinking water, do not drink more than 1 glass at a time;
- Do not leave various diseases to chance, especially those of the musculoskeletal system of the upper body (cervicothoracic region) - kyphosis, lordosis, osteochondrosis;
- Do not wear tight ties around your neck, do not pinch your neck with the collar; these things, by squeezing your neck, impair blood circulation in the head;
- Get enough sleep, follow your schedule - work/rest/sleep;
- Try not to take medications without a doctor’s prescription, because many of them have a number of side effects;
- If you are being treated for glaucoma, strictly follow the regimen of instilling eye drops for glaucoma;
- Visit your ophthalmologist regularly to prevent the development of glaucoma;
- Move more;