Congenital glaucoma (also called infantile) can be hereditary or result from exposure of the fetus to various adverse factors.
There are three forms of congenital glaucoma in children:
- simple congenital glaucoma (hydrophthalmos);
- glaucoma in combination with eye development abnormalities;
- glaucoma in combination with systemic congenital pathology.
According to experts, in a fairly large number of children (55.6%), the first signs of glaucoma appear at an early age (up to 5–6 years).
Causes of congenital glaucoma in children
The disease is based on congenital anomalies in the development of the angle of the anterior chamber and the drainage system of the eye, which create an obstacle to the outflow of intraocular fluid or significantly complicate it, which leads to an increase in intraocular pressure. The causes of this anomaly are various pathological conditions of the woman, especially in the first months of pregnancy. They are caused by a wide variety of reasons: infections (measles, rubella, influenza, etc.), poisoning, alcoholism, ionizing radiation, etc.
Glaucoma of childhood
Sidorenko EI Authors reveals the problem of pathogenesis, imperfection of classification and treatment of infantile glaucoma. The classification of infantile glaucoma is listed in details. Unfortunately, childhood glaucoma has significantly more problems than adult glaucoma. Even on the issue of classification of childhood glaucoma, there is no consensus; in pediatric ophthalmology, non-perforating types of operations - viscocanaculostomy, excimer types of surgery for glaucoma - are not widely used; gonioscopy is not widely used due to the negative attitude of children towards this procedure. Many research methods are more suitable for adults, require a certain intelligence and cannot be used in children. The classification described in the textbook by Kovalevsky E.I. is completely out of date and does not reflect the advances in glaucoma science. A more progressive classification was proposed by A.V. Khvatova in 1982, but it was never completed. In 1991, Sidorov E.G. together with Krasnov M.M. proposed a new classification. It came much closer to the classification of adults, but never found widespread use in clinical practice due to its cumbersomeness. In 2001, we proposed a classification that is closest to the classification of glaucoma in adults, since we are convinced that the violation of hydrodynamics in glaucoma in adults and children is based on the same reasons - dysgenesis of the anterior chamber angle. Severe dysgenesis of the anterior chamber angle is more severe and manifests itself immediately after the birth of a child - congenital primary glaucoma. Less severe dysgenesis of the anterior chamber angle manifests itself as juvenile primary glaucoma. And, finally, small changes in the anterior chamber angle, acting as nuances in the structure of the anterior chamber angle (A.P. Nesterov), are realized in primary glaucoma in adults. Glaucoma in children and adults caused by dysgenesis of the anterior chamber angle should be classified as primary glaucoma. Based on this concept, one should distinguish between primary (children and adults) and secondary glaucoma. Primary congenital glaucoma (PCG) Congenital primary glaucoma is one of the most severe eye pathologies in newborns, leading to early blindness. The disease is relatively rare - one case per 10,000 children, but among blind children, congenital glaucoma causes vision loss in 2.5-7% of cases, that is, almost every 10 child becomes blind from congenital glaucoma. The disease in 15% of cases is hereditary (familial) in nature or may be caused by disorders in the prenatal period and is more common in boys (3/2). In general, congenital glaucoma is a pathology of the first year of a child’s life, since by this age it manifests itself in more than 90% of cases. With congenital glaucoma, there are gross signs of dysgenesis in the anterior chamber angle, so it manifests itself early and progresses quickly, leading to irreversible vision loss within 2–3 weeks. Therefore, early diagnosis and early surgical treatment, aimed at eliminating obstacles to fluid flow and creating artificial outflow pathways, play a special role. Early diagnosis of the disease, which is crucial for successful treatment, is only possible with a good knowledge of its early signs by obstetricians, neonatologists and micropediatricians of maternity hospitals, local pediatricians and nurses caring for small children, since a pediatric ophthalmologist examines all children only at 2–4 one month of age in order to exclude congenital pathology. Etiology: 1. Hereditary glaucoma is observed in 15% of cases, is transmitted in an autosomal recessive manner and is often combined with other anomalies in the eye. 2. Intrauterine glaucoma develops under the influence of teratogenic factors (X-ray studies, hypoxia, vitamin deficiency, toxicosis, infectious diseases). Pathogenesis. We have already spoken partially about it. Congenital glaucoma is a consequence of incorrect and incomplete splitting of tissue in the anterior chamber angle during embryogenesis. Dysgenesis and anomalies of the anterior chamber angle in congenital glaucoma are pronounced. The main role, like primary glaucoma in adults, is played by retention (obstruction) of the outflow of intraocular fluid. Changes in the angle of the anterior chamber can be very diverse, up to its complete non-splitting and the absence of many links in the outflow tract. According to the localization of retention in congenital glaucoma, one should distinguish: – pretrabecular open-angle glaucoma, which comes in first place in terms of frequency of occurrence (62%). The angle is open, but mesodermal tissue is defined pretrabecularly; – pretrabecular angle-closure glaucoma (14.7%), which may be caused by the closure of the trabecula by the root of the iris, the ciliary body; – trabecular glaucoma, which can be caused by underdevelopment of trabeculae, sclerosis, its absence, pathological inclusion of ciliary muscle fibers in the trabecula; – intrascleral retention, which occurs in the absence, deformation, dislocation of Schlemm’s canal, with underdevelopment of the scleral spur, intramural outflow tracts, up to their complete absence. These gross changes in the drainage system leave no hope for success from therapeutic treatment and require urgent surgical intervention. Diagnosis of congenital glaucoma With congenital glaucoma, intraocular fluid is produced, the outflow of which is sharply hampered, fluid accumulates, and intraocular pressure increases. The load on the outer shell of the eye increases sharply and it begins to stretch. The child’s eyes at the beginning of the disease are beautiful: the anterior chamber deepens, the eyes are large, expressive, the sclera becomes bluish from stretching (the vascular sclera becomes visible). With continued stretching of the eyeball, its size sharply increases (buphthalmos - “bull’s eye”), the cornea becomes cloudy, the sclera sharply thins and in the form of staphylomas unevenly protruding outward, the eyes are blind, oscillating in nystagmus. The initial signs of congenital glaucoma are the horizontal diameter of the cornea slightly larger than the age norm. You can focus on the following dimensions: the diameter of the cornea in newborns is 9 – 9.5 mm; at 1 year – 10–10.5 mm; at 2–3 years – 10.5–11 mm. The depth of the anterior chamber in newborns is 1.5–2 mm; at 1 year – 2.5 mm; at 2–3 years – 3–3.5 mm. After 6 years, these data approach the size of an adult human eye - the diameter of the cornea is about 11.5 mm, the depth of the anterior chamber is about 3.5 mm; – the anterior chamber deepens; – with an increase in IOP, the limbus begins to stretch (expand), since in this place the outer shell is thinned and fragile. The limbus becomes wider than 1 mm; – the anterior ciliary vessels dilate; – the sclera stretches and the vascular tissue is visible through it – the sclera receives a delicate bluish tint; – a gentle (like morning fog) swelling of the cornea appears – opalescence. Stretching of the cornea leads to cracks in the endothelium and leakage of fluid into its thickness. Normally, in 15% of cases, newborns experience physiological opalescence of the cornea, which disappears within 1 week. For differential diagnosis, a 5% glucose solution or glycerin is instilled into the child’s eye - the pathological edema disappears, the physiological opalescence remains; – by 2–3 months, cranial innervation improves and photophobia appears due to irritation of the corneal nerves; – the pupil dilates and its sluggish reaction appears due to muscle atrophy; – a shift of the vascular bundle is noted in the fundus; – the eyes are large, beautiful, the diameter of the cornea increases, especially along its horizontal meridian. Secondary congenital glaucoma Secondary congenital glaucoma differs significantly from adult glaucoma in the variety of forms and is a consequence of other diseases. Secondary congenital ophthalmic glaucoma (SCOG) – with anomalies of the anterior segment of the eye 1) Aniridia in 50% of cases can be complicated by an increase in IOP. Glaucoma most often appears in adolescence. Children with aniridia should be under clinical supervision, with systematic monitoring of intraocular pressure. 2) Ectopic lens often results in the root of the iris being pressed against the trabecula or cornea by the displaced lens, causing glaucoma. 3) Rieger syndrome – mesodermal dysgenesis of the iris and cornea, a hereditary disease with a dominant type of transmission. The syndrome includes hypoplasia of the anterior layer of the iris, embryotoxon, mesodermal bridges extending from the basal part of the iris to the embryotoxon. Glaucoma usually develops after the first decade of life, and therefore the eyeball usually does not enlarge. 1) Frank-Kamenetsky syndrome is observed in men and is transmitted by a recessive, X-linked type. A distinctive feature of this iris hypoplasia is its two-colored appearance: the pupillary zone of 1.5–2 mm is grayish or blue or brown in color, the wider ciliary zone looks chocolate brown due to the exposure of the pigment layer. Glaucoma develops in the second decade of life. Secondary congenital syndromic glaucoma (SCSG) 1) Sterzh-Weber syndrome (encephalooculofacial hemiangiomatosis, encephalotrigeminal angiomatosis). The etiology is not fully understood, but heredity is of great importance. A systemic disease manifested by capillary hemangioma of the face, hemangioma and focal changes in the brain. A characteristic feature is capillary hemangioma of the face along the branches of the trigeminal nerve in the form of extensive purple spots. Neurological symptoms, which can manifest as epilepsy, hydrocephalus, paresis, mental disorders, and mental retardation, depend on the degree of intracranial angiomatosis. Glaucoma develops on the side of the nevus when the eyelids, especially the upper, and conjunctiva are affected. Such patients require systematic monitoring of IOP. 2) Neurofibromatosis. Congenital glaucoma can be observed in its generalized form with damage to the skin, bones, brain, endocrine system, and especially when localized in the area of the upper eyelid and temple. 3) Marfan syndrome, Marchesani - family-hereditary diseases, with damage to connective tissue, cardiovascular, musculoskeletal, endocrine and other body systems, accompanied by ectopia of the lens and, as a consequence, secondary glaucoma. Secondary acquired glaucoma (SAG) This type of glaucoma develops after diseases or injuries of the eye. The immediate cause of increased IOP in all forms of secondary glaucoma is a violation of the outflow of aqueous humor from the eye. A large number of different forms of secondary glaucoma can be combined into several groups: 1) uveal post-inflammatory glaucoma; 2) phacogenic glaucoma; 3) vascular glaucoma; 4) traumatic glaucoma; 5) glaucoma caused by degenerative processes; 6) neoplastic glaucoma. In uveal glaucoma, an increase in IOP is caused by the formation of goniosynechia, accumulation of exudate in the trabecular zone, fusion and fusion of the pupil. Anamnesis and detection of the described changes in the eye allows us to make a diagnosis. Phacogenic glaucoma occurs due to diseases of the lens: – phacotopic glaucoma is caused by a change in the position of the lens when it is subluxated or dislocated; – swelling of the cataract can also cause impaired hydrodynamics and increased ophthalmotonus – phacomorphic glaucoma; – overripe cataract causes phacolytic glaucoma due to the resorption of its masses and the macrophages involved in this close the trabecular membranes; Secondary vascular glaucoma often develops as a result of thrombosis of the central retinal vein, diabetes. Neovascularization in the angle of the anterior chamber impedes the outflow of fluid from the gas. Phlebohypertensive glaucoma occurs when pressure in the venous vessels of the orbit increases due to vascular tumors or compression of the superior vena cava. Traumatic glaucoma is divided into contusion and wound. In case of contusion from a hydrodynamic shock, the tabecular apparatus is often damaged and the angle of the anterior chamber is split, which complicates the outflow of fluid from the eye. Traumatic glaucoma is caused by adhesions in the angle of the anterior chamber. Degenerative secondary glaucoma occurs with uveopathy, phakomatoses, old retinal detachment, and with retinopathy of various origins. Neoplastic glaucoma develops from intraocular tumors, when their breakdown products obstruct the outflow of fluid from the eye.
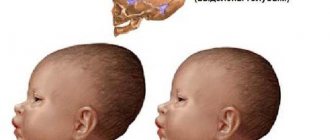
Main signs of congenital glaucoma
Congenital glaucoma is characterized by peculiar clinical manifestations due to age-related characteristics of the eyes in children.
If the child has glaucoma, symptoms may include the following:
- increased intraocular pressure;
- photophobia, lacrimation;
- an increase in the size of the eyeball (the child is born with large, “expressive eyes”), and the increase progresses rapidly;
- an increase in the diameter of the cornea (in later stages, the diameter of the cornea can reach 20 mm or more), the width of the limbus;
- swelling of the cornea (it looks cloudy);
- slowing of pupillary reactions;
- changes in the optic nerve head.
Congenital glaucoma is often combined with the simultaneous development of defects in other systems and organs (microcephaly, heart defects, deafness, phakomatoses, etc.) and in the eye (microcornea, aniridia, cataracts, etc.).
Congenital glaucoma develops in both eyes in 75% of cases. According to the observations of specialists, congenital and childhood glaucoma in most children is not accompanied by complaints, excluding those caused by corneal syndrome. In other words, the disease proceeds like open-angle glaucoma . In the later stages of glaucoma, staphylomas may appear, scleral ruptures are possible, and stretching and thinning of the conjunctiva is observed. Complicated cataracts often develop. In the initial stage of development of congenital glaucoma, the fundus is normal. As the disease progresses due to circulatory disorders, the optic nerve head undergoes dystrophic changes.
Congenital glaucoma is characterized by progressive deterioration of visual function. In the early stages, vision loss is mainly caused by changes in the cornea (swelling, clouding), refractive error, and farsightedness. During the development of congenital glaucoma, visual functions decrease as the optic nerve and retina are affected.
Treatment of juvenile glaucoma
Treatment begins with a conservative method, prescribing both local drugs and general agents. In the future, if the results are unsatisfactory or if the disease progresses rapidly, surgical treatment is resorted to.
Conservative treatment
- A course of blood pressure lowering medications
- Local miotic drugs: Carbacholin, Phosphacol, Armin,
- Diuretics, for example Diacarb,
- Specific agents that reduce intraocular pressure: reducing the production of intraocular fluid (Timolol, Trusopt), improving the outflow of fluid (Pilocarpine, Travatan), combined agents (Fotil, Proxofelin).
Treatment of congenital glaucoma
In the complex treatment of glaucoma in children, in addition to surgical methods, drug therapy plays an important role, including:
- reduction of IOP using a complex of antihypertensive drugs;
- prevention of severe postoperative scarring;
- the use of neurotrophic drugs to preserve and improve visual functions;
- desensitizing and restorative therapy.
Functional treatment is also necessary - correction of ametropia, pleoptic treatment (in children with congenital glaucoma, moderate and high myopia is more often detected).
Diagnosis and treatment
To accurately determine the presence of the disease, an examination is necessary to assess the anatomy and functionality of the eye. Then intraocular pressure is measured and the condition of the optic nerve is examined.
Carrying out diagnostic measures can cause certain difficulties, since not all diagnostic measures that are carried out for adults are applicable for children.
At the first stage of treatment, conservative methods are used. The goal of drug therapy is to normalize eye pressure and accelerate the outflow of fluid. Unfortunately, conservative treatment methods are often not effective enough. In this case, surgery is indicated for treatment.
The success of surgery depends on the correct choice of technique. This takes into account the transparency or degree of opacification of the cornea, the nature of damage to the optic nerve, other pathological changes, and the presence of concomitant diseases in the child. The operation can be performed at any age.
The following types of surgery for glaucoma are possible:
- goniotomy;
- trabeculotomy;
- sinustrabeculectomy;
- implantation of tubular drainage;
- application of laser technologies.
After surgery, the child will need some time for rehabilitation. For a month you should not visit a bathhouse or sauna, stay in dusty rooms, or lift heavy objects. Adults should ensure that children do not touch their eyes with their hands. For two weeks, it is necessary to instill eye drops with medications prescribed by your doctor.
Children with congenital glaucoma after surgery should remain under medical supervision in order to avoid further progression of the disease and preserve vision.
Dispensary observation
Children with suspected congenital glaucoma or with an established diagnosis are registered at a dispensary with a mandatory examination once a month: measurement of IOP, corneal diameter, limbal width, determination of visual functions (if possible).
Clinic licenses
Causes
Why does eye glaucoma occur? Often the disease is caused by a group of factors. The main thing that causes the disease is intraocular hypertension syndrome.
Genetic reasons:
- If glaucoma is detected in close relatives, then the likelihood of developing the disease increases 2–4 times. Specific genes responsible for the occurrence of glaucoma have been identified;
- The anatomical features of the eye (small vitreous body, large lens, narrow angle of the anterior chamber of the eye) prevent proper outflow of fluid.
Anomalies of eye development:
Age-related changes in the eye:
- in adults, due to the occurrence of degenerative changes, the capacity of the pectineal ligament decreases;
Metabolic disorders:
- pseudoexfoliation syndrome (an exfoliant substance is deposited in the trabecular system);
- pigment syndrome (desquamated iris pigment clogs the corner of the eye).
Factors causing narrowing of the iridocorneal angle:
- farsightedness (focusing the eye on distant objects leads to the expansion of the lens, which closes the entrance to the angle between the cornea and the iris);
- the use of drops that dilate the pupil (a fold forms at the base of the iris, preventing the outflow of aqueous humor).
Extraocular causes:
- diabetes mellitus, which leads to retinopathy;
- taking steroid drugs.
Considering the causes of the pathological process, the disease is divided into several varieties. Experts distinguish primary, secondary and congenital forms of the disease, each of which is characterized by its own provoking factors.
Doctors have not identified the main reasons that provoke the development of glaucoma in children. Experts are inclined to believe that the disease can manifest itself due to hereditary predisposition or due to the influence of other factors while the child is in the womb.
The following prerequisites for the disease are identified:
- pathologies of the nervous, cardiovascular, or endocrine systems;
- infectious diseases of the mother during pregnancy (typhoid, rubella, polio, syphilis, mumps, toxoplasmosis, vitamin deficiency);
- abnormal structure of the child's eyes;
- mother's bad habits;
- hypoxia suffered by the fetus in the womb.
Treatment methods
When congenital glaucoma is detected, experts insist on surgical intervention. Otherwise, all types of this disease result in complete loss of vision, as they stimulate optic nerve atrophy or retinal detachment.
Medication
It is quite difficult to select drugs that reduce blood pressure in a child, since most of them do not allow testing on children, and therefore cannot be recommended for the treatment of children. At the same time, if there are serious reasons, the ophthalmologist can prescribe a similar medicine to the child with the consent of the parents. Throughout the therapy, the attending physician monitors the baby’s condition.
Classification of congenital glauca
This disease has several varieties. Let's list them:
- hydrophthalmos (manifests in the 1st year of a child’s life);
- delayed (infantile) glaucoma (noted between the ages of 3 and 10 years);
- juvenile glaucoma (manifests after 11 years).
A special form of pathology is combined glaucoma, which is accompanied by developmental anomalies of other organs. Experts also use a classification of the disease by degree (there are three degrees of pathology).
Another way to classify congenital glaucoma is by the characteristics of the disease:
- typical - the clinical picture becomes clear when the child reaches the age of 3-4 months;
- benign - the clinical picture becomes clearer by the second year of life, the eye increases in size slightly;
- malignant - pronounced signs of glaucoma are recorded at the birth of the baby, or in the first months of his life, often the process is bilateral, the eyeball is greatly enlarged, the cornea is cloudy;
- abortive - intraocular pressure returns to normal, the disease does not progress.
Misconception #2
It is not difficult to detect glaucoma. She "hurts".
In fact. It depends on what form and stage of the disease we are talking about. Angle-closure glaucoma really manifests itself with attacks of sharp and severe pain that affects the forehead and temple area. At this time, the eyes turn red, visual acuity decreases, and photophobia appears. Sometimes the symptoms can be so severe that they even resemble an attack of acute indigestion, cerebrovascular accident or other acute conditions.
The open-angle form of glaucoma, which accounts for the majority of all cases of the disease among people of the European race, behaves differently, sometimes without reminding itself for years. It is no coincidence that it was called “silent”. At the same time, a person may feel normal and not suspect that he is standing at the fatal line. In 60% of cases, glaucoma is detected at “advanced” stages. Hence the confusion in morbidity statistics. It is believed that there are 1 million 200 thousand patients with glaucoma in our country. But, according to experts, there are much more of them - about 2 million. That is, almost 800 thousand patients with glaucoma do not even suspect their disease.
There is only one way out - to visit an ophthalmologist as soon as possible and undergo the examination recommended by a specialist. Starting from the age of 30, this must be done once a year. Then the doctor will have guidelines that, if a patient develops glaucoma, will help him choose the right treatment tactics and understand what IOP is optimal (target) for a given person.
Misconception #6
Glaucoma leads to sudden loss of vision.
In fact. With glaucoma, the fibers of the optic nerve do suffer, but (with the exception of an acute attack of glaucoma) this does not happen at lightning speed. As a rule, loss of visual fields in glaucoma is detected already when 30–40% of the optic nerve fibers are irreversibly atrophied. At the same time, patients do not even notice this for the time being. Only special devices can record such changes. What this leads to, alas, is known: gradually the field of view can narrow to... a small point. Experts call this tube vision. As a rule, this (like any other vision loss due to glaucoma) is an irreversible situation.
Types of glaucoma
Glaucoma has quite a large number of types. But, first of all, it is divided into two groups:
- primary (as an independent disease);
- secondary (occurs in other diseases as a complication).
Primary glaucoma is divided mainly into the following types:
- congenital (we will dwell on it in more detail);
- juvenile (occurs in adolescence);
- age-related (its development occurs in old age).
Secondary glaucoma develops as a complication of other diseases of the eyeball. which are very diverse. Let us name only some of the diseases in which secondary glaucoma is most common: inflammation of the choroid (uveitis), vascular disorders, pathology of the lens (subluxation, cataract, trauma), and post-traumatic conditions.
Misconception #8
If vision is lost, surgery is pointless.
In fact. The main goal of surgical treatment of glaucoma is to maintain vision at the level at which the disease was diagnosed. Even when it comes to residual visual functions. After all, glaucoma is often the fate of elderly, lonely people, for whom vision loss is a tragedy.
There is another - medical and social direction of such operations, when it is necessary to preserve an already blind eye, which is especially important for young patients from a psychological point of view. After all, a real doctor must think not only about the health, but also about the quality of life of his patient.
Diagnostic methods
At the moment when the child’s medical history begins to be filled out, a thorough anamnesis is collected. The child's parents may need to obtain extracts from their outpatient records. The mother will need to contact the antenatal clinic to make a copy of the documents that were kept during pregnancy. Based on these data, the doctor will be able to suggest the cause of the development of the pathology.
The next stage is a complete diagnosis, which includes:
- measurement of intraocular pressure;
- examination of the condition of all parts of the eye;
- determination of visual acuity;
- skiascopy;
- examination using a flashlight or slit lamp.
Some types of diagnostics that are applicable for adults cannot be performed on young patients. If surgery is planned, they may undergo a full examination, which is carried out under general anesthesia. It includes studies:
- pressure inside the eye;
- gonioscopy;
- pachymetry;
- ophthalmoscopy.
In some cases, several ultrasound examinations are included in the diagnosis. With them, the anteroposterior axis is measured. In newborns it should be 17 millimeters, and by one year it should be 20.
Prevention
Prevention of congenital glaucoma consists of preventing complications of pregnancy and prematurity. When planning a pregnancy, both parents should undergo genetic testing to determine the presence of genes responsible for the development of glaucoma. This study is especially relevant for parents who already have children with ocular hypertension.
During pregnancy, it is necessary to avoid infecting a woman with measles, rubella and influenza viruses. During planning, you should take a blood test to determine the strength of your immune system and, if necessary, undergo revaccination against these diseases. To prevent toxoplasmosis, a pregnant woman should avoid contact with pet excrement and consume only meat and milk that have been heat-treated.
The most important thing for preventing congenital glaucoma remains the prevention of prematurity. A woman should strictly follow the doctor’s instructions, take hormonal medications if necessary, and undergo an ultrasound examination at all screening times. If, according to the results of an ultrasound, there is a possibility of premature birth, a pessary is installed for the woman as prescribed by the gynecologist, and bed rest is prescribed.
After the birth of a child, prevention consists of a mandatory visit to a pediatric ophthalmologist in the first month and 1 year. If signs of glaucoma appear, you should not delay visiting your doctor. The sooner a newborn is diagnosed, treatment is started and surgery is performed, the better the prognosis and the higher the likelihood of maintaining high vision.
Diagnostics
When diagnosing glaucoma, not only a standard examination is performed, but also a study of heredity, as well as the course of pregnancy. With severe hydrophthalmos, it is much easier to determine the diagnosis of the baby. Significant difficulties arise with less pronounced symptoms and delayed manifestation of pathology.
An examination reveals an increase in the size of the eyeballs, which occurs with early disorders. The ophthalmologist also detects a weak reaction of the pupil to light and swelling of the intraocular tissues.
Due to the normalization of the baby’s pressure due to the elasticity of the sclera, tonometry indicators are commensurate with the normal size of the organ of vision. Enlargement of the eyeballs contributes to thinning of the retina with subsequent rupture, which increases the risk of a sharp decrease in visual acuity.
Examination of the structures of the eye at the microscopic level reveals iris atrophy, micro-tears, depressions of the anterior chamber and clouded areas on the cornea.
Standard ophthalmological examination methods include:
- ophthalmoscopy – examination of the fundus of the eye;
- visometry - checking the degree of visual acuity;
- biomicroscopy - examination of the elements of the organ of vision under a binocular microscope;
- refractometry - conducting refraction analysis;
- ophthalmotonometry – determination of intraocular pressure indicators;
- ultrasound biometry – study of the size of the eyeball;
- B-scan – (examination of eye clouding using ultrasound).
During the examination, a heredity analysis is carried out in order to identify similar symptoms in the baby’s closest relatives. If the mother suffered an injury or infection during pregnancy, this is taken into account when making a diagnosis.