Lens replacement is a radical way to treat refractive errors. It is often used for cataracts. The patient is immediately relieved of a clouded lens and refractive problems. There are other indications. Does this procedure help with astigmatism? Let us consider the features of correction of this pathology.
Astigmatism is a fairly common disease that occurs in almost every fourth inhabitant of the Earth. But not all people know about its presence. Mild degrees of this refractive error can only be detected with the help of modern computer equipment. A few decades ago, this diagnosis was not made; with poor vision, the patient was prescribed ordinary spherical glasses, which caused discomfort: dizziness, headaches, etc.
Today, astigmatism of any degree is detected within a few minutes during autorefractometry. It is corrected with glasses with a cylindrical component or contact optics with a toric design. This pathology can also be corrected using laser surgery, during which the shape of the cornea changes. A radical method of treating astigmatism is surgical lens replacement.
When is lens replacement prescribed for myopia?
Lens replacement for myopia is prescribed in the following cases:
- 1) High myopia – from -15 to -20 D
- 2) Refractive errors
- 3) Changing the shape of the lens
- 4) Hereditary lens diseases
- 5) Lens opacities
- 6) Contraindications to laser vision correction.
- 7) Patient's reluctance to wear glasses or contact lenses
Lens replacement for myopia is performed only on patients over 18 years of age.
Until this age, the eye continues to grow and its systems and tissues are in the process of formation. Also, surgery is not performed if vision is rapidly deteriorating - myopia must first be “stabilized”. Remember - surgery is a last resort method, it is prescribed only when other methods of combating the disease have not been effective. In the early stages, they try to correct vision with glasses, scleroplasty, and keratotomy.
Symptoms of lens clouding
The first symptom is that the image becomes blurry and visual acuity decreases. This reduces the quality of life: you can’t drive a car, work on a computer, and so on.
Refractive amblyopia is asymptomatic. It is detected during examination (prophylactic examination) more often in children 3-7 years old.
Occurs with hyperopic anisometropia, astigmatism, and high myopia. With myopic anisometropia it occurs less frequently, because the worst eye is used for near vision.
Amblyopia develops with the following refraction: the hypermetropic difference of both eyes is more than 0.5 diopters, the astigmatic difference is more than 1.5 diopters in any meridian, the myopic difference is more than 2.0 diopters.
Ametropic amblyopia develops in the absence of different refraction in both eyes, but with high degrees of myopia (more than 8 diopters bilaterally), hypermetropia (more than 5 diopters on both sides) and astigmatism (more than 2.5 diopters in any meridian). It is detected mainly in children under 7 years of age and is rarely accompanied by strabismus.
Vision with astigmatism and myopia
Nearsightedness or myopia is a visual defect characterized by poor distance vision. With myopia, the refractive ability of the cornea is impaired due to an increase in the size of the eyeball. The rays of light form an image not on the retina itself, but directly in front of it, as a result of which objects that are far from it appear blurry to a person. With high myopia, it is difficult for the patient to see even the face of the interlocutor.
Astigmatism is an equally severe visual defect. It occurs due to the curvature of the eyeball, cornea or lens of the eye. Light rays fall on two points of the retina, which leads to blurriness of the resulting image. A person with astigmatism almost constantly squints to make the image clearer.
Reviews from myopic patients about lens replacement
Due to blurred images and visual discomfort, patients who have recently undergone surgery are often depressed, but this does not mean that the surgical intervention did not produce positive results.
As numerous reviews of myopic patients who have undergone lens prosthetics show, vision improves in 98% of cases, although an increase in refraction cannot always be achieved immediately after surgery.
According to experienced ophthalmologist-surgeons, such symptoms will disappear after the wound heals and swelling subsides. So the main thing in this situation for patients is to wait until the rehabilitation period is completed.
It is very important to provide the person with absolute peace before and after surgery, since excessive anxiety often leads to negative consequences.
There are some known cases where older people ignored medical recommendations because they were afraid of worsening their condition. As a result, they lost their sight. Some patients say that after surgery the eye becomes more vulnerable to infection, but again this depends on the individual.
Complications after replacing the lens of the eye for cataracts
An effective and gentle method of phacoemulsification does not eliminate the risk of complications after replacing the eye lens for cataracts .
The advanced age of patients, concomitant diseases, and violation of sterility requirements by medical staff provoke undesirable consequences of the operation. Complications after cataract surgery occur in the form of swelling, astigmatism and other physical abnormalities.
People who have encountered such an unpleasant eye disease know firsthand that surgical intervention often ends badly, and there are complications after surgery.
Eye cataracts still require treatment. And unfortunately, the only way to get rid of the pathology is to perform an operation to remove the lens and replace it with an artificial one.
The procedure itself does not take much time and does not pose any threat to life and health, however, to avoid complications, you must adhere to certain rules and recommendations.
Types of complications
Complications that arise after the procedure include the following: Intraocular pressure in the eye increases. Inflammatory process. The retina of the eye peels off. Hemorrhage occurs in the anterior chamber.
The development of a disease such as secondary cataract. The new lens shifts slightly to the side. Below we will look at each type of complication in more detail. Inflammatory process.
After two to three days, all symptoms of inflammation should subside. Hemorrhage. This complication is rare; in most cases, it is associated with damage to the membrane or cornea of the eye at the time of surgery.
As a rule, the patient does not hurt anything, he sees everything, and after a few days there will be no trace of blood left, it will simply resolve. If this does not happen, the doctor will have to forcefully flush the anterior chamber.
Additional fixation of the lens is also performed. Intraocular pressure increases. This type of complication can occur because the drainage system becomes clogged with drugs of a viscous consistency.
The doctor uses them to protect the cornea of the eyes. You can solve the problem by dropping drops into the eye. In rare cases, the specialist makes a small puncture through which the eyes are subsequently washed. Swelling of the eye or cornea and astigmatism are also observed, but it goes away quickly.
Retinal disinsertion. This complication can be considered one of the most severe; it occurs due to injury during lens replacement. People who develop astigmatism also experience this complication.
Many ophthalmologists insist on performing an operation during which the sclera is sealed. If the area of detachment is insignificant, then restrictive laser coagulation can be performed.
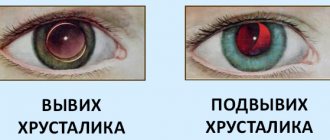
Retinal detachment In addition, due to the fact that the retina detaches, another unpleasant problem arises - the lens moves. Patients complain of astigmatism, the eye hurts greatly, is constantly accompanied by a feeling of discomfort, and swelling occurs.
All symptoms last only for a while; after rest, this condition goes away. But with a significant displacement, visual discomfort will occur constantly. In order to solve the problem, it is necessary to perform repeated surgery.
The lens is completely displaced. Lens displacement is a dangerous and serious complication that requires immediate intervention from specialists. During the operation, the lens is lifted and then securely fixed in its new position.
Myopia in children
Today, myopia is increasingly being diagnosed in pediatric patients. This is due to the fact that from a young age children already use phones, tablets, and computers, which negatively affect the health of their visual organs. As a rule, false myopia (a consequence of accommodation spasm) precedes true myopia.
The main task of the doctor is to prevent the development of myopia and prevent its progression if it is present. Stretching of the eye during progressive myopia leads to thinning of the sclera, especially in the posterior pole of the eye. In this regard, many changes in the fundus of the eye are possible: dystrophic changes in the macular region (the area of the fundus that provides 90% of our vision), peripheral dystrophy and retinal detachment.
What to pay attention to
What should parents pay attention to in order not to miss the moment and maintain the health of their child’s eyes?
- Children squint when trying to see distant objects.
- They try to sit closer to the TV.
- They complain about poor perception of what is written on the school board.
- Poor orientation in the twilight.
Tips for parents
- Children take their low vision for granted for a long time. Therefore, in order to detect myopia in a timely manner, it is important to undergo regular preventive examinations by a pediatric ophthalmologist.
- From an early age, teach your child simple rules: do eye exercises regularly, avoid prolonged continuous eye strain.
- Limit the use of devices for watching videos and games.
For children over 3 years of age, hardware and physiotherapeutic treatment may be recommended.
Company manufacturer
- Russian. They can be obtained free of charge if the operation itself is carried out under a compulsory medical insurance policy. These lenses are bifocal. At the moment, in Russia, at the Nizhny Novgorod company Reper NN, trifocal lenses are being designed.
- American. These lenses are the most famous. They are produced by world-famous companies - Acrisof, Alcon, Crystalens. Crystalens offers multifocal and accommodating lenses, which have become increasingly popular recently. Doctors' opinions about this product are contradictory; some believe that it is more of a promoted brand than a high-quality product.
- English, Rainer brands. It was in this country that they first began to produce artificial lenses and carry out operations to replace them. The company focuses on the optimal shape of its prostheses, which reduce the invasiveness of the operation and the recovery period.
- German. The most famous products are Human Optics and Carl Zeiss. Distinctive features of the first brand's prostheses are an aspherical edge and a high degree of light transmission. HumanOptics appeared on the Russian market approximately 3 years ago, but many doctors recommend their products. Artificial lenses from Carl Zeiss are manufactured using high-precision equipment. They offer multi- and monofocal prostheses, as well as toric lenses, recommended for cataracts complicated by astigmatism.
Prosthesis price
The cost of prostheses can range from 20,000 to 100,000 rubles. Companies that are still little known on the market, such as Human Optics, usually offer products cheaper than companies such as Alcon. Accommodating and multifocal lenses are the most expensive. For paid treatment, their price is usually included in the cost of the operation. Ordering lenses yourself is quite difficult; companies usually work only with wholesale buyers.
What documents are needed to return 13 percent from the purchase of an apartment?
A property transaction must undergo mandatory registration at the cadastral chamber or multifunctional center (MFC) at the location of the property. Registration is regulated by the norms of Federal Law No. 218-FZ of July 13, 2015 and Article 131 of the Civil Code of the Russian Federation.
According to the indicated sources, the owner receives a package of papers for the tax refund declaration when purchasing housing, which must be presented to the Federal Tax Service.
The following documents are provided to the tax office:
- A civil law agreement for the purchase and sale of an apartment certified by Rosreestr. This is the main document establishing the eligibility of individuals to receive the legal 13%.
- Certificate of ownership of the apartment issued by Rosreestr upon registration.
It is allowed to certify a property transaction at a notary’s office, which has the same authority as certification by Rosreestr.
This list of documents is attached to the following:
- owner's statement;
- receipt or bank receipt for payment of money;
- the applicant's civil passport.
The entire list of papers listed must be presented in the form of originals and photocopies.
Now let’s find out what documents are needed if registration takes place at the tax office. Additionally, originals are provided:
- certificates from the accounting department at the place of work in form 2-NDFL;
- completed tax return in form 3-NDFL.
Certificate of income of an individual, form 2-NDFL: form, sample filling.
Sample of filling out a certificate of income in form 2-NDFL
Tax return in form 3-NDFL: form, example of filling.
This is what a sample of filling out a declaration on form 3-NDFL looks like
Possible complications
Complications of eye surgeries depend on the method and extent of the intervention. Laser methods of treating myopia carry the least risks in terms of complications, while classical surgery has a wider range of possible consequences.
Possible complications of laser correction:
- erosive change or clouding of the cornea;
- hypercorrection;
- inflammation of the corneal layer – keratitis;
- scars and adhesions on the lens, causing irregular astigmatism;
- excessive dryness of the eye.
Possible complications of radial keratotomy:
- inflammatory processes in the tissues of the eye;
- adhesions and scars;
- persistent eye pain in the postoperative period.
Possible complications of lens replacement:
- postoperative swelling;
- inflammatory processes;
- retinal dystrophy or detachment.
Any unpleasant or unusual sensations experienced by the patient after correction is a reason to consult a doctor for additional examination. The ophthalmologist will prescribe the necessary treatment for complications and prevent their consequences.
Possible consequences
Cataracts can cause other diseases. such as phacogenic glaucoma, phacolytic iridocyclitis, obscurative amblyopia.
Important! Treatment with medications will only help to temporarily prolong the period of remission, but the risk factors for vision loss will remain. After a while, the cataract will make itself felt again.
Phacogenic glaucoma
Phacogenic glaucoma is a complication process or a consequence of various pathologies, including cataracts, as well as a consequence of mechanical damage to the eyeball.
The disease is accompanied by an increase in intraocular pressure. The risks of being left without vision are very high.
The main cause of the disease is an increase in intraocular pressure, which occurs due to an increase in the outflow of fluid from the eye area. Eventually, nerve cell atrophy develops, causing vision to rapidly deteriorate. Even early cataracts can provoke such a pathology.
Vision deteriorates in the dark or if a person enters a room from the street during the day or vice versa. If vision is significantly reduced, this indicates an advanced stage of the disease. It is dangerous due to loss of vision in the affected eye.
Important! The primary stages of glaucoma develop asymptomatically. These are the risk factors that cause blindness.
The disease is diagnosed against the background of cataracts only during a random examination. People who have crossed the 45th birthday should undergo eye examinations at least 2-3 times a year to eliminate the risk of developing blindness.
Treatment of pathology is carried out with medication and surgery. The main goal is to eliminate cataracts and normalize vision.
As in the case of cataract damage to the eye, surgery for glaucoma is the ideal option to eliminate the risks of complications and restore vision.
Phacolytic iridocyclitis
Phacolytic iridocyclitis is an inflammation of the iris and ciliary body. The inflammatory process is provoked by cataracts that are at the stage of overripening.
Doctors want to reach people and say that there is no cure for cataracts.
It is impossible to cure clouding of the lens with drops and tablets, and even more so with herbal decoctions. All these techniques are effective for preventing the disease or in the postoperative period.
Medicines and folk recipes can only prolong the course of the disease and improve vision for a while, but the clouding process, unfortunately, is irreversible.
Cataract is a hereditary disease.
The above criteria provoke the development of cataracts, especially in people who are at risk.
Complications, even with the laser method of treating the disease, still occur. But they are detected in the first days after the intervention, when there is still an opportunity to correct everything.
The main risk with laser dissection is damage to the intraocular lens by the beam. This happens very rarely, if the laser device is poorly calibrated.
What is long-term investing
What is the difference between a trader and a long-term investor
A trader tries to benefit from price fluctuations over short periods of time. Therefore, speculators often take advantage of local events on the Russian market or expectations from them.
The investor is trying to make money on fundamental principles and large-scale changes in the companies' business.
For ease of perception, I will transfer some differences to the table.
Trader Investor Short-term trading Investing for the long term Making quick decisions to buy and sell shares based on a single factor or local event Analyzing the entire issuer, making careful trade decisions Using technical indicators or specific financial triggers Focusing on the operating performance of the business or global changes in the company Establishing time or risk restrictions on a position Exiting a position in accordance with the achievement of the goals of a long-term idea or due to its cancellation Counting on small but frequent profits Counting on a large increase in the value of shares and receiving dividends Operating with small capital in transactions Large investments and creating diversified portfolios
Why long-term investing is sometimes combined with trading
Different ideas may translate differently into the nature of investing. The Russian market is influenced by many factors, and trading participants are not always able to predict and control risks. Therefore, investors are looking to diversify their approaches. This is called diversification of strategy.
As an example, I will immediately move on to the Russian stock market.
The geopolitical situation around our country has been in a tense state for a long time. The stock prices of our companies are affected by sanctions pressure and associated risks. Therefore, securities of Russian issuers maintain a significant discount to their global counterparts over a long period.
Why long-term investments are not popular in Russia
Recently, the situation with long-term investing has been changing for the better. Products have appeared in the form of individual investment accounts, which have gained well-deserved popularity, and more and more participants in the Russian market prefer investing.
Some people, influenced by advertising, choose exclusively speculative strategies in the hope of getting rich quickly. Subsequently, such people, having lost money, switch to more conservative and long-term approaches using fundamental analysis of company shares.
As for investing on the stock exchange in general, the matter here is complicated by the Russian mentality and historical aspects. Shares are vested rights to own part of a company's business. And when in our country the rights of citizens are violated with enviable regularity, people are reluctant to give their money to the stock market.
How much can you earn
The main benchmark for determining profitability on the Russian market is the Moscow Exchange index. Dividends should also be taken into account. Over the past 10 years, the Moscow Exchange index with total return (MICEX Total Return) brought about 13% per annum.
If we talk about real numbers, then a more or less diversified portfolio with separately selected promising shares of companies can on average bring 15-35% per annum, taking into account dividends.
How is lens replacement performed for astigmatism?
Before the procedure, the patient undergoes tests and undergoes a full examination. The operation is performed under local anesthesia. The patient must follow all doctor's instructions during procedures. The surgeon makes a small incision in the cornea, emulsifies the contents of the lens, removes it, and inserts an intraocular lens (IOL) into the posterior chamber of the lens. The eye is then washed with a special solution and covered with a protective bandage.
Complications are also possible after this procedure. Early side effects include swelling of the cornea, redness of the eyes, and increased sensitivity to light. Late complications include cataracts and insufficient accommodative ability. The quality of vision largely depends on the type of IOL chosen.
What types of IOLs are used to replace the lens for astigmatism?
There are three types of artificial lenses that replace the natural lens:
- toric, which are the most effective and therefore expensive;
- multifocal, providing good vision at all distances;
- phakic - lenses that are placed in front of the lens without removing it.
Causes and symptoms of the disease
The development of pathology is based on cortical inhibition, which “switches off” the poorly seeing eye from the visual process, preventing the development of diplopia (double vision).
Primary amblyopia occurs when the development of the eyeball is impaired in the prenatal period.
- obscuration (due to long-term opacities of the optical media of the eye, most often the lens).
- post-obscuration (amblyopia that persists after the cause of the obscuration has been eliminated). For example, after replacing the lens with an intraocular lens, visual acuity does not improve
During surgery to remove a damaged lens, doctors preserve its capsule, where they implant an intraocular lens. The artificial lens is hidden in a thin elastic bag.
But epithelial cells can begin to grow around this capsule. Do not think that the reasons for this are the incompetence of surgeons.
Rather, they lie in the body's ability to perform certain cellular reactions.
Replacing the lens of the eye for myopia (myopia)
We have all heard the concept of “myopia” or “myopia”. A person with this disease has difficulty seeing objects located at a great distance. This is where the name of the disease comes from - good vision is preserved only at arm's length. You need to start treating myopia as early as possible - then you can avoid many complications and you won’t have to resort to surgery. However, in some cases, conservative methods do not help and the doctor prescribes a lensectomy - a refractive lens replacement that can be used to restore normal vision to the patient.
When is lens replacement prescribed for myopia?
Lens replacement for myopia is prescribed in the following cases:
- 1) High myopia – from -15 to -20 D
- 2) Refractive errors
- 3) Changing the shape of the lens
- 4) Hereditary lens diseases
- 5) Lens opacities
- 6) Contraindications to laser vision correction.
- 7) Patient's reluctance to wear glasses or contact lenses
Lens replacement for myopia is performed only on patients over 18 years of age.
Until this age, the eye continues to grow and its systems and tissues are in the process of formation. Also, surgery is not performed if vision is rapidly deteriorating - myopia must first be “stabilized”. Remember - surgery is a last resort method, it is prescribed only when other methods of combating the disease have not been effective. In the early stages, they try to correct vision with glasses, scleroplasty, and keratotomy.
How is the operation performed?
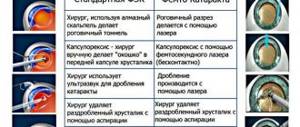
Replacement of the lens of the eye for myopia is carried out using the phacoemulsification method, which practically does not cause complications.
The operation takes 15-30 minutes and is performed under a microscope on an outpatient basis.
Through an incision, ultrasound is used to emulsify the patient's lens and then remove it. In its place, an intraocular lens (an artificial lens) is implanted, which will subsequently be responsible for focusing the image on the retina. Sometimes it becomes necessary to install not one, but two lenses, which is also not a big problem. IOLs for myopia and other operations on the lens are selected individually, taking into account the patient’s vision characteristics. Only a doctor can do this.
Possible complications
Complications during surgical treatment of myopia (myopia) are associated primarily with the course of the underlying disease. The fact is that with myopia, the eyeball becomes enlarged, which affects all systems of the visual organ. There may be:
- 1) Dystrophic changes in the retina
- 2) Retinal tears due to thinning
- 3) Reducing the thickness of the outer shell of the eye (sclera)
- 4) Retinal detachment
That is why lens replacement for high myopia is prescribed only after a thorough examination and taking into account all possible consequences.
The optimal age for surgery is after 40 years.
By this time, the ability to accommodate is partially lost, and the first signs of cataracts may appear. After surgery, the patient needs to visit an ophthalmologist regularly to monitor his vision and detect complications at the earliest stage.
After operation
Replacing the lens for myopia is a fairly well-established operation. The postoperative period is usually well tolerated. The patient is discharged the next day after the follow-up examination, and vision is restored almost immediately
However, it is necessary to observe some precautions, which are mainly related to the need to protect the operated eye from damage. Recommended:
- 1) Do not bend over sharply
- 2) Do not touch your eyes with dirty hands
- 3) Wear a special bandage
- 4) Avoid physical activity
- 5) Do not visit the bathhouse or sauna for a week
- 6) Wear glasses on sunny and windy days
- 7) Follow all doctor’s recommendations.
Cost of lens replacement for myopia
The cost of replacing a lens for myopia is determined mainly by the cost of an artificial lens. You can choose a monofocal lens - it is cheaper, but you will need glasses for correction, since you will only see well at a certain distance. If you give preference to a multifocal lens, then you will not need glasses - such an lens has several focusing points for different distances. The price also includes consumables. You can find out the exact cost in our price list in the section on cataract surgery - phacoemulsification.
Treatment of amblyopia
Treatment is impossible without an ophthalmologist, and untimely treatment of amblyopia leads to permanent loss of visual function.
First, the optimal correction is selected. in older children, it is possible to use contact or night lenses, laser correction, especially with anisometropia (different refraction of both eyes).
Eliminate the cause of obscurative amblyopia (eyelid surgery for ptosis, photorefractive surgery for corneal opacities, phacoemulsification and IOL implantation for cataracts, resorption therapy or vitrectomy for hemophthalmos).
For strabismic amblyopia, passive and active pleoptics are used.
Pleoptics
Passive is carried out through occlusion of the dominant eye (visual acuity in the squinting eye increases), and then variable occlusion for the transition of strabismus to alternating (in this case, an image from one or the other eye is recorded on the central fovea).
After this, active pleoptics methods are used. With adequate correction, the leading eye is closed and the retina of the squinting eye is stimulated (with light, laser, electrical impulses and special computer programs).
Pleoptic treatment is carried out 3-4 times a year to achieve the desired effect.
Hardware treatment is the mainstay for amblyopia. For example, training on "Amblyocor", while depending on the activity of the cerebral cortex, recorded during electroencephalography, the characteristics of the image on the computer change.
Amblyocor
ASO stimulation (using colored light pulses), FEM, PS-1, Mosaic PS-2, Panorama, etc. are also used.
In children who cannot tolerate occlusion, the method of penalization with atropine is used in the better seeing eye. A wide pupil sharply reduces visual acuity, thereby forcing the amblyopic eye to “work.” Atropine is instilled 1-2 times a week and care is taken to ensure that mydriasis is constant.
Physiotherapy methods are widely used - vibration massage, reflexology.
Treatment is completed after achieving approximately the same visual acuity in both eyes. If strabismus remains, it is eliminated surgically.
The prognosis of amblyopia in adults is unfavorable; in children, adequate treatment with complete correction is necessary.
Ophthalmologist Letyuk T.Z.
Why is it worth resorting to surgery?
Myopia imposes serious restrictions on a person’s life, including in professional activities and sports. Among other things, the pathology progresses non-stop if there is no proper treatment.
As mentioned earlier, in initial and moderate forms of the disease, the ophthalmologist prescribes glasses or contact lenses to the patient
However, it is important to understand that these remedies only correct a visual defect, but are not able to cure it. You can completely get rid of high myopia only by replacing the natural lens with an artificial one.
Vision with astigmatism and myopia
Nearsightedness or myopia is a visual defect characterized by poor distance vision. With myopia, the refractive ability of the cornea is impaired due to an increase in the size of the eyeball. The rays of light form an image not on the retina itself, but directly in front of it, as a result of which objects that are far from it appear blurry to a person. With high myopia, it is difficult for the patient to see even the face of the interlocutor.
Astigmatism is an equally severe visual defect. It occurs due to the curvature of the eyeball, cornea or lens of the eye. Light rays fall on two points of the retina, which leads to blurriness of the resulting image. A person with astigmatism almost constantly squints to make the image clearer.
Indications and contraindications
Indications for refractive lens replacement are high degrees of myopia (more than -20D) and hypermetropia (more than 20D). The procedure is also performed if it is impossible to correct vision using laser techniques.
Refractive lensectomy is the operation of choice for the development of glaucoma against the background of hypermetropia and age-related farsightedness. as well as with a rapid decrease in visual acuity throughout the year.
Among the contraindications to refractive lens replacement are dystrophic changes in the retina with the threat of retinal detachment, and the small size of the anterior chamber of the eye. Inflammatory diseases of the visual structures in the acute phase, decompensation of chronic diseases and the presence of a viral or bacterial infection are reasons to cancel the operation until the patient’s condition normalizes.
Replacement of the eye lens is necessary in the following cases:
- cataract;
- lens luxation;
- intolerance to glasses and lenses;
- astigmatism;
- presbyopia;
- myopia;
- deterioration of accommodation processes;
- age-related farsightedness.
Attention! Many experts recommend simultaneous surgical treatment of glaucoma and lens replacement.
There are a number of contraindications to refractive lens replacement:
- inflammatory processes in the visual apparatus;
- the anterior chamber is too small;
- retinal detachment;
- diabetes;
- hypertension;
- progressive farsightedness, accompanied by a small size of the eyeball;
- suffered a stroke or heart attack.
Answers to popular questions
Before surgery, patients often ask certain questions that concern them most.
How long does the operation take?
The minimum duration of the procedure is 15-20 minutes, and the maximum can reach 2 hours, but this happens rarely. On average, the operation lasts 30-40 minutes.
How much does eye lens replacement surgery cost (average price in St. Petersburg and Moscow)?
The cost of the operation depends primarily on the implant used. In capital cities, minimum prices start from 35-40 thousand rubles and can reach 140 thousand.
When will vision be restored?
When vision returns after lens replacement is greatly influenced by the general health of the patient, his retina and the optic nerve. The rehabilitation period after surgery is at least 4 weeks, by the end of which vision should fully return.
After lens replacement, the eye sees cloudy - why and what to do?
Normally, after lens replacement, the eyes are very afraid of light. During the first week, decreased vision and a hazy effect persist. This is a natural state of the body, it does not require correction, but the doctor’s recommendations must be strictly followed.
To combat complications in which fog in the eyes persists for a long time after lens replacement, the following measures must be taken:
- clouding of the lens capsule, or secondary cataract - after the intervention, the patient in rare cases begins to see worse. Correction requires laser discision - a small operation that lasts 10-15 minutes and does not require long-term rehabilitation;
- increased intraocular pressure - along with the fact that the eye, after replacing the lens, does not see as it should, painful sensations arise. Correction requires drug therapy as prescribed by a doctor;
- infection - the bacterium enters at the time of surgery or during the rehabilitation period, various symptoms occur, including acute pain and discharge from the eyes. To prevent it, it is necessary to undergo a course of antibacterial therapy during the recovery period;
- Corneal edema is a complication that affects the ability to see normally, but lasts no longer than 1-2 days. No specific treatment is needed;
- retinal detachment – accompanied by pain and requires consultation with a doctor. Laser and cryotherapy are used for treatment; in severe cases, repeated surgery is required.
Other reasons why complications arise after cataract removal with lens replacement are extremely rare (less than 1%).
When does vision return after eye lens replacement?
During the first week, vision remains cloudy, but if you follow medical recommendations, complete recovery occurs after 2-3 weeks. The replaced lens is fully rehabilitated after 4 weeks of rehabilitation. Laser vision correction after lens replacement is required in very rare cases complicated by eye pathologies.
In general, reviews of lens replacement for high myopia, cataracts and other diseases are positive, and patients note the following:
- no serious consequences;
- quick opportunity to return home;
- simple rehabilitation with strict adherence to the doctor’s recommendations.
However, patient reviews often describe minor disadvantages: a cloudy look on the first day after surgery, the high cost of the procedure for complex interventions, the presence of edema. Some people are very nervous before surgery.
In the video, a man shares his impressions after replacing the lens of his eye:
When can you watch TV?
You can watch TV after replacing the transparent lens within a few days - the exact period is determined by the doctor. Reading and working on a computer is allowed after 1-2 weeks.
Diagnosis of amblyopia
— determination of visual acuity with and without correction. For children who do not know letters, tables with pictures are used (for example, Orlova’s table)
— biomicroscopy
— determination of the angle of strabismus using the Hirschberg method — normally, the reflex from the ophthalmoscope is located in the center of the pupil. With strabismus, asymmetrical
— determination of the type and angle of strabismus using a synoptophore
Synoptophore
- refractometry for complete cycloplegia (preferably atropinization for 3-4 days)
- skiascopy - determination of refraction by the characteristic movement of the shadow in the pupil area
- examination in transmitted light to determine the transparency of the eye media
- examination of the fundus with a Goldmann lens
— electroretinography to determine the functional state of the retina
- critical frequency of flicker fusion - studies the states of neurons. The indicator is the minimum number of flashes of light, which is perceived as a single whole
— Ultrasound of the eye – examines the state of the media of the eye if they are opaque and the length of the anterior-posterior segment of the eye (important for refractive errors)
— computed tomography, magnetic resonance therapy, consultation with a neurologist to exclude pathologies of the nervous system
Why do you have to change the lens for myopia and astigmatism?
Both types of ametropia greatly complicate a person’s life, impose certain restrictions on him in professional activities, and interfere with his ability to play sports. These pathologies constantly progress if left untreated. For initial and moderate degrees of myopia and astigmatism, the patient is prescribed to wear glasses or contact lenses.
However, correction means are not means of treatment; they only correct a refractive error, that is, they allow a person to see well, despite the presence of visual pathology. Myopia and astigmatism can be treated with laser surgery or lens replacement surgery. The latter treatment method is usually used for high degrees of myopia and astigmatism.
What are IOLs?
Lenses of this type are one of the most significant achievements of modern science in the field of ophthalmology. To eliminate severe degrees of myopia, implants in the form of phakic IOLs are used.
Phakic lenses have the form of concave plates that follow the shape of the anterior parts of the organ of vision, the thickness of which is only 30 microns. They are implanted into the eye, and the lens is not removed. Made from high-quality hypoallergenic types of medical silicone. It is completely biocompatible and retains its properties for 80-100 years. In other words, these are the same contact lenses, only much more advanced. They are not placed over the eye, but are surgically implanted. With their help, the patient acquires the ability to see well both near and far.
The lenses are implanted into the anterior or posterior chambers of the eye. They differ slightly in shape. The former are implanted in the space between the cornea and the iris, the latter in the space between the iris and the lens.