Megalocornea is a rare eye pathology in which the size of the cornea is noticeably increased. With megalocornea, concomitant abnormalities also appear: deterioration in the quality of vision, disturbances in other structures of the eye. The pathology does not require special treatment, but it is necessary to carry out therapeutic measures and correct vision.
The first significant description of megalocornea was made at the beginning of the 20th century, when it was identified as a separate disease. Before this, pathological enlargement of the cornea was considered a consequence of glaucoma. It has been proven that this occurs due to a mutation on the X chromosome, so it affects men in 90% of cases. An anomaly such as megalocornea is a genetic congenital disorder, so when examining the eyes of a newborn, this parameter is also checked. It happens that this disease is one of the symptoms of hydrophthalmos - a pathological increase in the size of the eyeball.
What disorders occur with megalocornea?
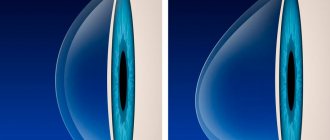
The pathology develops in both eyes at once - the cornea begins to increase in diameter, but retains its transparency. The course of the disease is individual: the anomaly may not have pronounced symptoms, but in some situations, especially against the background of other genetic syndromes, visual disturbances and pathologies of the eye parts develop.
Thus, a decrease in visual acuity may be observed, and sometimes iridodonesis is diagnosed - trembling of the iris during eye movements. Stretching of the muscular apparatus of the lens, glaucoma (due to impaired outflow of intraocular fluid), pupil constriction, cataracts and other negative consequences may occur. Megalocornea can provoke the development of myopia, hypermetropia and astigmatism due to changes in the refractive power of the enlarged cornea.
Megalocornea
Megalocornea is a bilateral disease, usually not prone to progression. The main symptom of this pathology is detected in early childhood during examination - the cornea is enlarged in diameter, with preserved transparency. Clinical manifestations of megalocornea depend on the severity of disturbances in the structure and thickness of the cornea. In the absence of changes, visual functions remain within normal limits. Bilateral damage to the cornea is often accompanied by dystrophic disorders (mosaic dystrophy) and pigment sputtering. Most often, patients experience a slight decrease in visual acuity (often both far and near) and a feeling of distortion of objects in front of the eyes, which is associated with the development of myopia and astigmatism. Sometimes megalocornea is complicated by subluxation of the lens, which is caused by stretching of the ligamentous apparatus. In this case, patients exhibit clinical symptoms of iridodonesis - trembling of the iris that occurs during sudden eye movements.
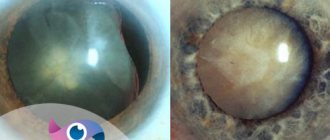
The clinical picture associated with increased intraocular pressure is detected only with such a complication as pigment dispersion syndrome with the subsequent development of secondary glaucoma. In this case, a redistribution of pigment occurs from the pigment layer of the posterior layer of the iris. Melanocytes settle on the structures of the posterior part of the eyeball. This leads to obstruction of the trabecular network of the anterior chamber angle with impaired outflow of intraocular fluid. Patients complain of fog before the eyes, pain, decreased visual acuity, and the appearance of “rainbow circles” when looking at a light source. In severe cases, stretching of the iris is possible, followed by stromal hypoplasia and increased pigmentation of the trabecular meshwork. The result of these changes is the formation of the Krukenberg spindle.
Megalocornea can develop as an independent disease or occur against the background of genetic pathologies such as Aarskog, Marfan and Kniest syndromes. The most common concomitant pathologies of the organ of vision are ectopia of the lens and pupil, congenital miosis, pigmentary glaucoma, subcapsular cataract. In turn, megalocornea can act as one of the symptoms of hydrophthalmos.
Diagnostics
The doctor conducts a visual examination and also prescribes additional methods for a detailed examination of all parts of the eye. This is important to understand whether pathological changes have begun in them.
Diagnostics consists of several studies:
- tonometry, viziometry;
- refractometry, ultrasound;
- coherence tomography, keratometry, keratotopography - these methods allow you to identify any changes in the cornea.
If necessary, the specialist prescribes additional methods to help most fully assess the condition of the visual organs. Based on the results of the data obtained, a further treatment plan is drawn up.
Complications
Megalocornea is dangerous due to a number of complications arising from the unnaturally large size of the anterior ocular chamber. This leads to an increase in the amount of interchamber fluid, which often affects the condition of the lens and retina.
- Ectopic lens (displacement or dislocation);
- cataract (clouding of the lens);
- pigment dispersion syndrome (pigmentary glaucoma);
- tendency to retinal detachment;
- pathological spastic miosis.
Megalocornea therapy
If, after diagnosis, the doctor does not identify obvious and health-threatening disorders - changes in refraction, increased intraocular pressure, then there is no need for therapy. If myopia, hypermetropia, or astigmatism occurs, correction means are prescribed - glasses or lenses. When cataracts develop, surgery is performed to install an artificial lens, etc.
What changes occur with megalocornea?
As a rule, pathology develops in both eyes at once - the cornea begins to grow in diameter, while maintaining its transparency. However, there are no general signs of eye damage during the course of the disease: they are individual for each person. With megalocornea, stretching of the muscular apparatus of the lens often occurs, the normal outflow of intraocular fluid is disrupted, which causes glaucoma to develop. Constriction of the pupil, cataracts and other changes may also occur. Megalocornea can contribute to the development of myopia, farsightedness and astigmatism due to the fact that the refractive power of the cornea is impaired due to its increased size. Iridodonesis can also be observed - trembling of the iris during eye movements.
Causes of megalocornea
The causes of megalocornea are that the pathology is transmitted from the owner of the defective gene or directly from mother to baby. The disease appears in the first trimester of pregnancy during the formation of the visual apparatus in the fetus. During normal development, the optic cup changes from a bell shape to a sphere. Changes occur at 6 weeks. In a fetus with megalocornea, transformation is observed later. Therefore, the diameter of the ciliary belt and adjacent structures increase in size. The anatomical distribution of the structural elements of the cornea does not differ from normal. However, it increases in diameter and becomes thinner.
Treatment of megalocornea
If visual acuity, refraction and intraocular pressure remain within normal limits, then no special therapy is required. If refractive errors such as astigmatism, myopia and farsightedness are detected, correction of visual perception is necessary using contact lenses or glasses. With megalocornea, surgical treatment is not always possible due to the constricted pupil and possible partial dislocation of the lens. There is also a possibility of rupture of the posterior lens capsule. If secondary cataracts occur due to the disease, then experts recommend phacoemulsification. After this, a special intraocular lens (artificial lens) is implanted. Surgery is performed through a corneoscleral incision. Retrobulbar anesthesia is used as anesthesia.
Diagnosis of anomaly
Taking an anamnesis is important in patients with this congenital pathology. The disease can be observed in relatives of the child, both in isolation and as part of common genetic diseases. With biomicroscopy, the doctor reveals an increase in the cornea and the depth of the anterior chamber. Measuring the thickness of the cornea (pachymetry) reveals central thinning. It is possible to additionally conduct keratotopography and keratotopometry, which will determine the degree of refractive error by measuring the curvature of the cornea.
Why is megalocornea dangerous?
First of all, pathology threatens the frequent development of complications. Due to dystrophic changes and redistribution of melanocytes, pigment accumulates in the structures of the anterior segment of the eye. Violation of the outflow of intraocular fluid is accompanied by pain, fog and the appearance of floaters, and decreased visual function. It is characterized by a sharp increase in intraocular pressure, up to the occurrence of a glaucomatous attack. Increased pigmentation of the trabecular meshwork, visible in transmitted light, is called the Krukenberg spindle.
Pigment closure of the anterior chamber angle in megalocornea is a serious complication that leads to progressive vision loss.
Complications of megalocornea
If pathology occurs, you should immediately seek help from a specialist.
Megalocornea is dangerous due to complications that appear due to an increase in the size of the anterior ocular chamber:
- the liquid level between the chambers increases;
- cataracts occur;
- retinal detachment occurs;
- pigmentary glaucoma appears;
- the lens moves.
Also, against the background of megalocornea, spastic miosis may appear.
Treatment
There is no specific treatment. The disease does not cause direct visual impairment and is not life-threatening, so all treatment is reduced to symptomatic therapy and prevention of complications. If mahalocornea is suspected, an enlarged cornea of the child is registered with an ophthalmologist and regular examinations are recommended.
To learn more about eye diseases and their treatment, use the convenient site search or ask a specialist a question.
We advise you to read the article about another congenital disease in babies.
Development of the disease
If, with the development of this pathology, a violation of the normal transparency of the cornea does not occur, the anterior chamber takes on a more enlarged and deeper state, in contrast to the norm. At the same time, the condition of the eyeball will be in a normal state, and no congestion will be observed. The state of palpation and ophthalmotonus also remains within normal limits.
When this disease has been discovered, it is imperative to consider the possibility that obtaining an enlarged cornea may be a very basic sign of the presence of congenital glaucoma (this disease is also called hydrophthalmos). In this case, a note is placed in the completed baby’s chart indicating that the patient was found to have an anomaly in the development of the cornea of the eye. There are suspicions of congenital glaucoma.
Megalocornea differs from hydrophthalmos mainly in that it does not tend to progress, which is why the cornea can remain transparent for a long time. Development of the disease:
- does not cause thinning and serious expansion of the limbus;
- does not cause any ruptures in Descemet's membrane;
- glaucomatous excavation and functional disorders are not observed;
- intraocular pressure is normal.
In the absence of the listed symptoms and signs, a final diagnosis can be made during the examination of the patient.
Symptoms of megalocornea
Megalocornea is a bilateral disease that often does not progress. The main symptom of megalocornea is a transparent cornea, which significantly increases in diameter. The clinical picture of the disease directly depends on the progression of pathological disorders of the cornea. If no changes are observed, then the functions of the visual organ remain normal.
If a patient develops a bilateral lesion of the cornea, dystrophy and pigment dispersion may occur. In patients, visual acuity decreases, the outlines of objects are distorted. Myopia and astigmatism may appear. Sometimes eye disease is aggravated by partial dislocation of the lens, which occurs from stretching of the ligamentous apparatus. In this case, symptoms of iridodonesis arise - trembling of the iris, which appears with a sudden movement of the eyes.
Prevention of megalocornea
There are no effective methods for preventing the development of megalocornea. If one of the parents has the disease, during pregnancy you must strictly follow all the specialist’s instructions, undergo an ultrasound examination and take care of your health. If there is a genetic mutation and the disease occurs, the first step is to differentiate the disease from other diseases, since megalocornea is rare. The disease does not endanger the patient's health, but after 30 years the chances of developing secondary cataracts increase. Experts advise periodically visiting an ophthalmologist and undergoing a detailed examination in order to notice the progress of the disease in time. Prof. The examination consists of procedures such as vision and tonometry. If you suspect an increase in the diameter of the cornea, it should be measured as quickly as possible.
Megalocornea is a fairly rare disease. Every little patient who is diagnosed with an illness is registered with a specialist and monitored throughout his life. The difficulty in preventing and treating the disease is explained by its genetic nature. However, even in the most difficult cases of megalocornea there is a possibility of partial recovery. A complete decrease in visual perception or blindness occurs only against the background of complications in the form of glaucoma or cataracts. Effective treatment methods help eliminate possible secondary diseases in this eye pathology.